Abstract
Background
Propofol infusion syndrome (PRIS) is a rare but frequently fatal condition. It is characterized by cardiovascular collapse and metabolic derangement due to propofol exposure. The pathophysiology of PRIS is poorly understood, and its study has previously been limited to animal models and clinical observations. We present the first in vivo brain biochemical data in a patient with PRIS.
Methods
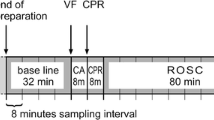
We report the case of a 37-year-old woman with PRIS following aneurysmal subarachnoid hemorrhage who was monitored by cerebral microdialysis (CMD). A CMD catheter was inserted into the brain and provided near real-time monitoring of brain energy-related metabolites, including lactate and pyruvate, during the time period surrounding the diagnosis of PRIS. We recorded propofol exposure, clinical manifestations, and relevant laboratory measurements.
Results
CMD revealed a temporal association between propofol exposure and the cerebral lactate-to-pyruvate ratio (LPR). The LPR increased linearly after propofol was restarted following an off period, and the LPR decreased linearly after propofol was discontinued. Serum lactate correlated with clinical worsening after the onset of PRIS, whereas cerebral LPR correlated with propofol exposure.
Conclusions
Cerebral LPR may be a sensitive marker of PRIS. Increases in LPR following propofol exposure should alert clinicians to the possibility of PRIS and might prompt early discontinuation of propofol thereby avoiding fatal complications.



Similar content being viewed by others
References
Zaccheo MM, Bucher DH. Propofol infusion syndrome: a rare complication with potentially fatal results. Crit Care Nurse. 2008;28(3):18–26. quiz 27.
Marik PE. Propofol: an immunomodulating agent. Pharmacotherapy. 2005;25(5 Pt 2):28S–33S.
Rosen DJ, Nicoara A, Koshy N, et al. Too much of a good thing? Tracing the history of the propofol infusion syndrome. J Trauma. 2007;63(2):443–7.
Bray RJ. Propofol infusion syndrome in children. Paediatr Anaesth. 1998;8(6):491–9.
Kam PC, Cardone D. Propofol infusion syndrome. Anaesthesia. 2007;62(7):690–701.
Fudickar A, Bein B. Propofol infusion syndrome: update of clinical manifestation and pathophysiology. Minerva Anestesiol. 2009;75(5):339–44.
Wolf A, Weir P, Segar P, et al. Impaired fatty acid oxidation in propofol infusion syndrome. Lancet. 2001;357(9256):606–7.
Ypsilantis P, Politou M, Mikroulis D, et al. Organ toxicity and mortality in propofol-sedated rabbits under prolonged mechanical ventilation. Anesth Analg. 2007;105(1):155–66.
Delgado JM, DeFeudis FV, Roth RH, et al. Dialytrode for long term intracerebral perfusion in awake monkeys. Arch Int Pharmacodyn Ther. 1972;198(1):9–21.
Tisdall MM, Smith M. Cerebral microdialysis: research technique or clinical tool. Br J Anaesth. 2006;97(1):18–25.
Frontera JA, Claassen J, Schmidt JM, et al. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery. 2006;59(1):21–7 (discussion 21–27).
Marcoux J, McArthur DA, Miller C, et al. Persistent metabolic crisis as measured by elevated cerebral microdialysis lactate-pyruvate ratio predicts chronic frontal lobe brain atrophy after traumatic brain injury. Crit Care Med. 2008;36(10):2871–7.
Vasile B, Rasulo F, Candiani A, et al. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med. 2003;29(9):1417–25.
Schulz MK, Wang LP, Tange M, et al. Cerebral microdialysis monitoring: determination of normal and ischemic cerebral metabolisms in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2000;93(5):808–14.
Cray SH, Robinson BH, Cox PN. Lactic acidemia and bradyarrhythmia in a child sedated with propofol. Crit Care Med. 1998;26(12):2087–92.
Mehta N, DeMunter C, Habibi P, et al. Short-term propofol infusions in children. Lancet. 1999;354(9181):866–7.
Persson L, Hillered L. Chemical monitoring of neurosurgical intensive care patients using intracerebral microdialysis. J Neurosurg. 1992;76(1):72–80.
Koch M, De Backer D, Vincent JL. Lactic acidosis: an early marker of propofol infusion syndrome? Intensive Care Med. 2004;30(3):522.
Haase R, Sauer H, Eichler G. Lactic acidosis following short-term propofol infusion may be an early warning of propofol infusion syndrome. J Neurosurg Anesthesiol. 2005;17(2):122–3.
Kill C, Leonhardt A, Wulf H. Lacticacidosis after short-term infusion of propofol for anaesthesia in a child with osteogenesis imperfecta. Paediatr Anaesth. 2003;13(9):823–6.
Veldhoen ES, Hartman BJ, van Gestel JP. Monitoring biochemical parameters as an early sign of propofol infusion syndrome: false feeling of security. Pediatr Crit Care Med. 2009;10(2):e19–21.
Engstrom M, Polito A, Reinstrup P, et al. Intracerebral microdialysis in severe brain trauma: the importance of catheter location. J Neurosurg. 2005;102(3):460–9.
Johnston AJ, Steiner LA, Chatfield DA, et al. Effects of propofol on cerebral oxygenation and metabolism after head injury. Br J Anaesth. 2003;91(6):781–6.
Acknowledgments
We thank Suzanne Frangos, RN, CNRN and the Neurosurgery Clinical Research Division for assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pisapia, J.M., Wendell, L.C., Kumar, M.A. et al. Lactate-to-Pyruvate Ratio as a Marker of Propofol Infusion Syndrome After Subarachnoid Hemorrhage. Neurocrit Care 15, 134–138 (2011). https://doi.org/10.1007/s12028-010-9467-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9467-6