Abstract
Background
The process of discontinuing neurological patients from mechanical ventilation is still controversial. The aim of this study was to report the outcome from extubating patients undergoing elective craniotomy and correlate the result with the measured f/V t ratio.
Materials and Methods
In a cohort prospective study, all consecutive patients who required mechanical ventilation for up to 6 h after elective craniotomy were eligible for inclusion in this study. Patients passing daily screening criteria automatically received a spontaneous breathing trial (SBT). Immediately previous to the extubation, the expired minute volume (VE), breathing frequency (f), and tidal volume (V t) were measured and the breathing frequency-to-tidal volume ratio (f/V t) was calculated; consciousness level based on Glasgow Coma Scale (GCS) was evaluated at the same time. The extubation was considered a failure when patients needed reintubation within 48 h.
Results
Ninety-two patients were extubated and failure occurred in 16%. Despite 15 patients failed extubation just one of them presented the f/V t score over 105. The best cutoff value for f/V t observed was 62, but with low specificity (0.53) and negative predictive values (0.29). Area under the ROC curve for the f/V t was 0.69 ± 0.07 (P = 0.02). Patients who failed the extubation process presented higher incidence of pneumonia (80%), higher need for tracheostomy (33%) and mortality rate of 40%.
Conclusion
The f/V t ratio does not predict extubation failure in patients who have undergone elective craniotomy. Patients who fail extubation present higher incidence of pneumonia, tracheostomy and higher mortality rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The process of discontinuing patients from mechanical ventilation is still controversial and consists of two components: weaning from ventilatory support and extubation. Both delayed and premature extubation have been associated with adverse outcomes. Delayed extubation is associated with increased length of hospital stay, increased risk for ventilator-associated pneumonia, and increased mortality in brain-injured patients [1]. On the other hand, extubation failure is also associated with adverse outcomes as increased hospital mortality, prolonged hospital stay, higher costs, and greater need for tracheostomy [2–6].
Different strategies have been documented for weaning neurosurgical patients from mechanical ventilation and extubation [7, 8]. Neurosurgical patients are predisposed to a number of complications related to mechanical ventilation and retrospective and prospective investigations have documented increased rates of reintubation, pneumonia, and prolonged mechanical ventilation among these patients [9–11]. However, a weaning protocol based on traditional respiratory physiologic parameters may have limitations for use in neurosurgical patients [8].
Several studies [12–20] have addressed objective criteria to predict weaning from mechanical ventilation in the intensive care unit. Attention has now moved toward redefining the decision of patient extubation, as 10–20% of extubations may still fail and require reintubation [21–25]. Multiple weaning parameters have been investigated as possible predictors of extubation outcome [26–31]. Breathing frequency–tidal volume ratio (f/V t) has been the one most studied, although it has not been proven to be accurate [32]. Cutoff value of 105 has been pointed out as a predictor for extubation success/failure. As far as we know an f/V t score has not yet been developed to predict extubation success in neurosurgical patients. This ratio has been developed for mechanical ventilated patients with heterogeneous diagnosis and they usually are very awake. However, it is not uncommon for neurosurgical patients under mechanical ventilation to present an abnormal consciousness level, which should be a factor accounted for during weaning process.
The aim of this study was to report the outcome from extubating patients undergoing elective craniotomy and correlate the result with the measured f/V t ratio.
Materials and Methods
Population Studied
Between July 2002 and July 2006, consecutive patients who required mechanical ventilation for more than 6 h after elective craniotomy for tumor, aneurysm, and arterio-venous malformation (AVM) were enrolled from the neurosurgical ICU in the Sao Paulo Federal University Hospital. Patients who underwent tracheostomy or died before weaning trial; unplanned extubation and patients intubated before surgery were excluded from this study. This study was approved by the Ethics Committee for Human Research of the University and informed consent was obtained from all patients.
Data Collection
Preoperative Assessment
All patients answered a questionnaire on the presence of respiratory symptoms, lung and other clinical diseases and smoking. Physical examination included the observation of the type of cough and expectoration, pulmonary auscultation, chest evaluation and determination of the level of consciousness based on Glasgow Coma Scale (GCS).
Postoperative Assessment
Patients who remained intubated after the surgery were referred to the ICU and maintained under mechanical ventilation using a Bear 1000 ventilator (Allied Health Care Productions, USA), Monterey ventilator (Takaoka, Brazil) or Bird 8400 STI PC Vaps ventilator (Bird, USA). Patients were followed-up daily during the postoperative period by the same team that assessed the preoperative period, until they were discharged or died.
Patients passing daily screening criteria automatically received a spontaneous breathing trial (SBT). The following criteria had to be satisfactory to pass the daily screening: (a) responsible neurosurgeon consent; (b) GCS ≥ 8; (c) core temperature not >38°C; (d) no therapy with vasoactive drugs (dobutamine or dopamine was allowed in doses ≤5 μ/kg body weight/min); and (e) adequate gas exchange, as indicated by a PO2 of at least 60 mmHg with an inspired fraction of oxygen of ≤0.4 and a positive end-expiratory pressure not >5 cmH2O. The weaning consisted of a minimum 30 to 120-min trial of spontaneous breathing performed on a T-tube or pressure support of ≤8 cmH2O and peep level ≤5 cm H2O. All patients ultimately passed a SBT and were extubated. The criteria used to define failure to tolerate the SBT were (a) oxygen saturation <90%; (b) respiratory rate of >35 breaths/min for >10 min; (c) decrease or increase in the systolic blood pressure by >20%; (d) signs of increase of work of breathing for >15 min; and (e) diaphoresis or agitation. For the SBT to be considered a failure, any two criteria above had to be met. The SBT was terminated and mechanical ventilation reinstituted at the original settings if the physician identified two of the set predictors for poor tolerance.
After successful completion of a SBT and immediately prior to extubation, the expired minute volume (VE), breathing frequency (f), and tidal volume (V t) were measured using a ventilometer attached to the endotracheal tube (model RM 121, Ohmeda, Japan) without ventilatory support and the breathing frequency-to-tidal volume ratio (f/V t) was calculated; consciousness level based on GCS was evaluated at the same time. Physicians caring for the patients were blinded to ventilometry results.
Extubation failure was considered when patients needed reintubation within 48 h. The decision to reintubate the patient was based on clinical deterioration as evidenced by at least one of the following criteria: decreased mental status; worsening in arterial pH or PCO2; decrease in the oxygen saturation to <90%, despite inspired fraction of oxygen >0.5; and increased signs of respiratory work (tachypnea, use of accessory respiratory muscles, thoracoabdominal paradox).
Patients were divided into two groups based on the level of consciousness at the moment of extubation: GCS of 10–11T and 8–9T, where the letter T shows that patients were submitted to orotracheal intubation at the time of evaluation. We considered the group with GCS of 10–11T basically normal once they were able to respond to simple commands and the group with GCS of 8–9T altered because they did not show logical response to simple commands.
Pulmonary infection complications were monitored. Pneumonia was defined as the presence of pulmonary infiltration on the chest X-ray associated with at least two of the following signs: purulent tracheobronchial secretion and increased body temperature (above 38.3°C) and blood leukocytes (over 25% above the base line count) [33].
Statistical Analysis
Results are shown as mean and standard deviation. Clinical threshold value for frequency-to-tidal volume ratio (f/V t) of ≤62 breath/min/l was derived from the current study and threshold values for respiratory rate of ≤25 breaths/min and minute volume ≤10 l/min from previous studies [13, 32, 34]. A true positive (TP) test was defined as one which predicted extubation success when extubation was successful; true negative (TN), one which predicted failure and the patient was reintubated; false positive (FP), one which predicted success and the patient failed; false negative (FN), one which predicted failure and the patient succeeded. Sensitivity (TP/TP + FN), specificity (TN/TN + FP), positive predictive value (TP/TP + FP) and negative predictive value (TN/TN + FN) were determined for rate/volume ratio, minute volume, and respiratory rate. Receiver operator curves (ROC) were constructed for f/V t, minute volume and respiratory rate. For univariate analysis, the chi-square test was used for 2 × 2 and 3 × 2 tables and Fisher’s exact test for 2 × 2 tables when one or more of the expected frequencies was less than five. Statistical analysis was performed with SPSS (version 13.0; SPSS, Chicago, IL). A P-value ≤ 0.05 was considered to be significant for all tests.
Results
Four hundred and twenty patients submitted to intracranial surgery were admitted in the neurosurgical ICU during the study period, 173 under mechanical ventilation and 92 of them were enrolled in the study. Out of the 81 excluded patients, 10 had had a tracheostomy before the weaning process, 17 died before weaning, 20 were extubated within 6 h after surgery, seven had an unplanned extubation, 10 were submitted to endovascular procedure and five to ventricular derivation, and 12 patients were intubated before surgery. The characteristics of the 92 patients included in this study are listed in Table 1.
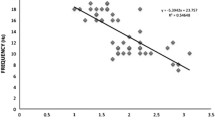
All 92 patients were successfully weaned from mechanical ventilation and extubated, but 15 of them (16%) required reintubation within 48 h. Reasons for failed extubation were: decrease in consciousness level in 53%, worsening in work of breathing with normal consciousness level in 20%, inability to protect airway (witnessed aspiration or an inability to maintain airway patency because of pulmonary secretions) in 13.5% and seizures in 13.5%. Ninety out ninety-two patients had an f/V t ratio <105. Table 2 lists the predictive characteristics of f/V t ratio, respiratory rate and minute volume. Areas under the ROC curves for the respiratory rate and the f/V t were 0.74 ± 0.07 (P = 0.003) and 0.69 ± 0.07 (P = 0.02), respectively (Fig. 1).
Patients with normal consciousness levels had more chance of success, patients who failed extubation presented a higher incidence of pneumonia, tracheostomy, and higher mortality rate (Table 3).
Discussion
We evaluated a homogeneous cohort of 92 neurosurgical patients submitted to elective craniotomy and found no association between the f/V t ratio and extubation failure. In addition we found an incidence of 16% of reintubation, in agreement with another study with similar population [8].
Yang and Tobin [12], first described that a value of 105 or over for the f/V t ratio would predict unsuccessful extubation. However, they evaluated a heterogeneous population. Subsequent studies showed that the different results observed for the relation of f/V t ratio and extubation success was mainly related to the point in time of the extubation process, the test was applied and to the kind of patients evaluated [3, 5, 8, 13, 18, 20, 26, 32, 34].
Currently, the predictive extubation indexes are being applied at the moment of extubation, as it is considered to be more important to detect the failure in the extubation process than in the weaning process.
We observed that the 105 score for f/V t is not applicable to neurosurgical patients. Despite 15 patients failed extubation just one of them presented a score of over 105. The best cutoff value observed by us was 62, but with low specificity (0.53) and negative predictive values (0.29). Even though, sensitivity was 0.75 and positive predictive value 0.89, we believe that the most important aspect in a predictive index should be its ability to predict failure but not success.
Other studies have also observed different cutoff points for population with homogeneous diagnosis, such as COPD patients [32] with a cutoff of 84 or aging patients with cutoff of 130 [26]. In a recent multicenter study, Frutos-Vivar et al., found a cutoff value for f/V t ratio of 57 in patients who had undergone invasive mechanical ventilation for >48 h and had been extubated following a successful SBT [5].
Yang and Tobin [12], demonstrated that the f/V t ratio measured during 1 min of spontaneous breathing through the endotracheal tube had a very high negative predictive value (NPV = 0.95) and a high positive predictive value (PPV = 0.78) for weaning failure. Several subsequent reports have noted a significantly lower predictive accuracy for f/Vt [7, 26, 27, 34, 35] and in our study we also found a low NPV (0.29) and high PPV (0.89) even with a cutoff of 62. A recent randomized study showed that including the f/V t ratio in a protocol prolonged weaning time did not confer survival benefit or reduce the incidence of extubation failure or tracheostomy [20].
Fast and shallow breathing frequency usually indicates an abnormal lung condition. Breathing frequency over 35 is considered as tachypnea and these patients are expected to have a more difficult evolution from the perspective of extubation and mechanical ventilation [4, 36, 37]. We considered 25 respirations per minute in our patients as a cutoff point for unsuccessful extubation. However taken isolatedly, breathing frequency showed low specificity (0.33) and negative predictive value (0.38). Minute ventilation of 10 l was not a good predictor either, with a specificity of 0.53 and negative predictive value of 0.28.
The accuracy of the f/V t test depends on how well it separates those patients that will be successful and those with failure extubation. Accuracy is measured by the area under the ROC curve. An area of 1 represents a perfect test; an area of 0.5 represents a worthless test. A rough guide for classifying the accuracy of a diagnostic test is the traditional point system: 0.9–1 = excellent; 0.8–0.9 = good; 0.7–0.8 = fair; 0.6–0.7 = poor; and 0.5–0.6 = fail. The values for the area under the ROC curve in this study for the respiratory rate was 0.74 and for the f/V t ratio 0.69, confirming they were not good predictors of extubation failure [38].
Multiple weaning parameters have been investigated as possible predictors of extubation outcome and studies have shown that they are not accurate predictors [18, 27–29, 39–42]. On the basis of the difficulty to find predictors of failure extubation, few studies have been reported, however, that link the relationship between preoperative/intraoperative characteristics and postoperative extubation outcome [43–45].
Clinical and surgical characteristics of the patients who succeeded or failed extubation were not significantly different, but we observed that patients with a consciousness level at the moment of extubation considered to be normal (10–11T) were more likely to be successful. In other words, the chance of a patient with a normal consciousness level is higher for him/her to be among the ones with successful extubation that among the ones who fail. However, the f/V t ratio did not seem to be influenced by the level of consciousness, since patients with a low consciousness level presented an f/V t ratio mean of 50 ± 24, while patients with normal consciousness levels presented 56 ± 28 (P = 0.51).
Results have been controversial concerning the level of consciousness and the ability to maintain a satisfactory airway after extubation. Namen et al., found more extubation failure on neurosurgical patients with low consciousness level [8]. Chevron et al., in a prospective case–control study, found that a low consciousness level correlated with unplanned extubation and the need for reintubation [46]. On the contrary, others studies have shown that patients with a low consciousness level may be extubated successfully [1, 7]. Currently, a normal level of consciousness is still considered as a main variable for extubation.
Extubation failure is considered to be a risk factor for pulmonary complications and death [19]. Some studies have suggested an increased incidence of nosocomial pneumonia in patients undergoing reintubation [5, 9, 47, 48]. The patients of this study, who failed the extubation process presented a higher incidence of pneumonia (80%), a higher need for tracheostomy (33%), and a mortality rate of 40%.
A limitation on our study was the low median time of orotracheal intubation, 20.6 (11.2–34.0) h, but was similar to findings in a population of surgical patients (24 h) who also had the f/Vt ratio evaluated [34]. Heterogeneous populations may present a longer orotracheal intubation length of time.
In summary, we have found that the f/V t does not predict extubation failure in patients who have undergone elective craniotomy. Patients with a normal consciousness level presented a higher success rate for extubation. The extubation failure was associated to a higher incidence of pneumonia, tracheostomy, and death.
References
Coplin WM, Pierson DJ, Cooley KD, et al. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med 2000;161:1530.
Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest 1997;112:186–92.
Esteban A, Alía I, Gordo F, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. Am J Respir Crit Care Med 1997;156:459–65.
Esteban A, Alía I, Tobin MJ, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1999;159(2):512–8.
Frutos-Vivar F, Ferguson ND, Esteban A, et al. Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest 2006;130(6):1664–71.
Rothaar RC, Epstein SK. Extubation failure: magnitude of the problem, impact on outcomes, and prevention. Curr Opin Crit Care 2003;9(1):59–66.
Vallverdú I, Calaf N, Subirana M, et al. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med 1998;158:1855–62.
Namen AM, Ely EW, Tatter SB, et al. Preditors of successful extubation in neurosurgical patients. Am J Respir Crit Care Med 2001;163:658–64.
Torres A, Gateli JM, Aznar E, et al. Re-intubation increases the risk of nosocomial pneumonia in patients needing mechanical ventilation. Am J Respir Crit Care Med 1995;152:137–41.
Epstein SK, Ciubotaru RL. Independent effects of etiology of failure and time to reintubation on outcome for patients failing extubation. Am J Respir Crit Care Med 1998;158(2):489–93.
Hsieh AH, Bishop MJ, Kubilis PS, et al. Pneumonia following closed head injury. Am Rev Respir Dis 1992;146(2):290–4.
Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445–50.
Chatila W, Jacob B, Guaglionone D, et al. The unassisted respiratory rate–tidal volume ratio accurately predicts weaning outcome. Am J Med 1996;101:61–7.
Jaeschke RZ, Meade MO, Guyatt GH, et al. How to use diagnostic test articles in the intensive care unit: diagnosing weanability using f/V t. Crit Care Med 1997;25:1514–21.
Vassilakopoulos T, Zakynthinos S, Roussos C. The tension–time index and the frequency/tidal volume ratio are the major pathophysiologic determinants of weaning failure and success. Am J Respir Crit Care Med 1998;158:378–85.
Zeggwagh AA, Abouqal R, Madani N, et al. Weaning from mechanical ventilation: a model for extubation. Intensive Care Med 1999;25:1077–83.
Shikora SA, Benotti PN, Johannigman JA. The oxygen cost of breathing may predict weaning from mechanical ventilation better than the respiratory rate to tidal volume ratio. Arch Surg 1994;129(3):269–74.
Lee KH, Hui KP, Chan TB, et al. Rapid shallow breathing (frequency–tidal volume ratio) did not predict extubation outcome. Chest 1994;105:540–3.
Epstein SK. Decision to extubate. Intensive Care Med 2002;28:535–46.
Tanios MA, Nevins ML, Hendra KP, et al. A randomized, controlled trial of the role of weaning predictors in clinical decision making. Crit Care Med 2006;34(10):2530–5.
Epstein SK. Extubation failure: an outcome to be avoided. Crit Care 2004;8(5):310–2.
Esteban A, Frutos F, Tobin MJ, et al. A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med 1995;332(6):345–50.
Brochard L, Rauss A, Benito S, et al. Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation. Am J Respir Crit Care Med 1994;150(4):896–903.
Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 1996;335(25):1864–9.
Cohen JD, Shapiro M, Grozovski E, et al. Extubation outcome following a spontaneous breathing trial with automatic tube compensation versus continuous positive airway pressure. Crit Care Med 2006;34(3):682–6.
Krieger B, Isber J, Breitenbucher A, et al. Serial measurements of the rapid-Shallow-breathing index as a predictor of weaning outcome in elderly medical patients. Chest 1997;112:1029–34.
Epstein SK. Etiology of extubation failure and the predictive value of the rapid shallow breathing index. Am J Respir Crit Care Med 1995;152:545–9.
Capdevila XJ, Perrigault PF, Perey PJ, et al. Occlusion pressure and its ratio to maximum inspiratory pressure are useful predictors for successful extubation following T-piece weaning trial. Chest 1995;108(2):482–9.
El-Khatib MF, Baumeister B, Smith PG, et al. Inspiratory pressure/maximal inspiratory pressure: does it predict successful extubation in critically ill infants and children? Intensive Care Med 1996;22(3):264–8.
Fernández-Crehuet R, Díaz-Molina C, De Irala J, et al. Nosocomial infection in an intensive-care unit: identification of risk factors. Infect Control Hosp Epidemiol 1997;18:825–30.
Gandia F, Blanco J. Evaluation of indexes predicting the outcome of ventilator weaning and value of adding supplemental inspiratory load. Intensive Care Med 1992;18:327–33.
Alvisi R, Volta CA, Righini ER, et al. Predictors of weaning outcome in chronic obstructive pulmonary disease patients. Eur Respir J 2000;15:656–62.
Murphy TF, Sethi S. Bacterial infection in chronic obstructive disease: state of the art. Am Rev Respir Dis 1992;146:1067–683.
Jacob B, Chatila W, Manthous CA. The unassisted respiratory rate/tidal volume ratio accurately predicts weaning outcome in postoperative patients. Crit Care Med 1997;25:253–7.
Fessler HE. Does weaning postpone liberation? Crit Care Med 2006;34(10):2676–7.
Jubran A, Tobin MJ. Pathophysiologic basis of acute respiratory distress in patients who fail a trials of weaning from mechanical ventilation. Am J Respir Crit Care Med 1997;155:906–15.
Tobin MJ, Perez W, Guenther SM, et al. The pattern of breathing during successful and unsuccessful trials of weaning from mechanical ventilation. Am Rev Respir Dis 1986;134:1111–8.
Thomas G. Tape, MD. Interpreting Diagnostic Tests. Available online at: http://gim.unmc.edu/dxtests/Default.htm. Accessed 1 May 2007.
Epstein SK. Endotracheal extubation. Respir Care Clin N Am 2000;6(2):321–60.
Meade M, Guyatt G, Cook D, et al. Predicting success in weaning from mechanical ventilation. Chest 2001;120(6 Suppl):400S–24S.
Krieger BP, Ershowsky PF, Becker DA, et al. Evaluation of conventional criteria for predicting successful weaning from mechanical ventilatory support in elderly patients. Crit Care Med 1989;17(9):858–61.
Leitch EA, Moran JL, Grealy B. Weaning and extubation in the intensive care unit. Clinical or index-driven approach? Intensive Care Med 1996;22(8):752–9.
Ingersoll GL, Grippi MA. Preoperative pulmonary status and postoperative extubation outcome of patients undergoing elective cardiac surgery. Heart Lung 1991;20:137–43.
Rady MY, Ryan T. Perioperative predictors of extubation failure and the effect on clinical outcome after cardiac surgery. Crit Care Med 1999;27:340–7.
Engoren M, Buderer NF, Zacharias A, et al. Variables predicting reintubation after cardiac surgical procedures. Ann Thorac Surg 1999;67(3):661–5.
Chevron V, Menard JF, Richard JC, et al. Unplanned extubation: risk factors of development in predictive criteria for reintubation. Crit Care Med 1998;26:1049–53.
Dupont H, Le Port Y, Paugam-Burtz C, et al. Reintubation after planned extubation in surgical ICU patients: a case–control study. Intensive Care Med 2001;27(12):1875–80.
Fagon JY, Chastre J, Hance AJ, et al. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med 1993;94(3):281–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vidotto, M.C., Sogame, L.C.M., Calciolari, C.C. et al. The Prediction of Extubation Success of Postoperative Neurosurgical Patients Using Frequency–Tidal Volume Ratios. Neurocrit Care 9, 83–89 (2008). https://doi.org/10.1007/s12028-008-9059-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-008-9059-x