Abstract
Aberrant signaling pathways are a hallmark of cancer. A variety of strategies for inhibiting signaling pathways have been developed, but monoclonal antibodies against receptor tyrosine kinases have been among the most successful. A challenge for these therapies is therapeutic unresponsiveness and acquired resistance due to mutations in the receptors, upregulation of alternate growth and survival pathways, or inadequate function of the monoclonal antibodies. Vaccines are able to induce polyclonal responses that can have a multitude of affects against the target molecule. We began to explore therapeutic vaccine development to antigens associated with these signaling pathways. We provide an illustrative example in developing therapeutic cancer vaccines inducing polyclonal adaptive immune responses targeting the ErbB family member HER2. Further, we will discuss new strategies to augment the clinical efficacy of cancer vaccines by enhancing vaccine immunogenicity and reversing the immunosuppressive tumor microenvironment.
Similar content being viewed by others
Introduction
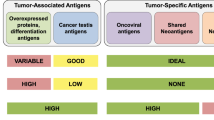
Manipulating the immune system to target malignancies, though approaches ranging from autologous dendritic cell–based vaccines to therapeutic immune-modulation [1–4], is now leading to clinical benefit, but a number of opportunities and challenges remain. Identifying novel tumor antigens continues to be a priority, and insights from sequencing the cancer genome have revealed a number of genetic changes in cancer cells including somatic mutations, translocations, and amplifications which can lead to novel cancer-specific antigens [5–7]. The role of post-translational modification in the generation of novel cancer antigens is also an opportunity to be explored [7]. Characterizing the immunosuppressive environment of tumors and developing strategies to counter or evade these suppressive influences has been receiving considerable attention, and an emphasis on the generation and regulation of antigen-specific T cells has also been central to research in cancer immunotherapy. However, we believe that the emerging recognition that cancer signaling pathways play pivotal roles in the biologic behavior of tumor cells creates an opportunity to rethink modern cancer immunotherapy strategies [8–10]. For example, there are clinically validated antigens found on cancer which have been targeted by both monoclonal antibodies and small molecules (Table 1). Interestingly, these targeted approaches are also generally associated with high rates of therapeutic resistance which does not typically involve loss of antigen expression, making them potential targets for alternative immunotherapeutic strategies [11, 12]. One such strategy is to develop polyclonal humoral immune responses by active immunotherapy.
The therapeutic potential of polyclonal immune responses to HER2
An example of a credentialed tumor-associated antigen is the human epidermal growth factor receptor 2 (HER2), overexpressed in 20–30% of breast cancers and associated with more aggressive tumors and inferior overall survival [13]. Combinations of the anti-HER2 antibody trastuzumab and chemotherapy lengthen survival in metastatic HER2-overexpressing breast cancer [14]. However, progressive disease typically occurs within 1 year. Lapatinib, a potent reversible inhibitor of HER2 and EGFR tyrosine kinases [15], in conjunction with chemotherapy, enhances time to progression in these patients [16]. Unfortunately, responses to lapatinib are generally short lived, and progression remains a significant clinical problem.
As mentioned earlier, the overexpression of HER2 persists in trastuzumab and lapatinib-refractory tumors [11, 12, 17–19], and thus targeting HER2 with a polyclonal adaptive immune response that includes both T cells and antibodies is a potential strategy. More than a dozen phase I and II studies of cancer vaccines have been conducted in breast cancer patients [20]. These vaccines have included proteins, peptides, modified tumor cells, and dendritic cells loaded with breast tumor antigens. In these studies, HER2 has been demonstrated to be immunogenic, with a suggestion that immunized patients had an improved clinical outcome [21–25].
We have developed an adenoviral vector vaccine expressing a kinase-inactive, full-length human HER2 gene (Ad-HER2-ki), which we have demonstrated is non-oncogenic [26] to overcome safety the potential safety issues around using an oncogene as a vaccine. We have shown that this vector induces HER2-specific T-cell responses and polyclonal antibody responses capable of mediating both antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC). This is distinct from the effects of trastuzumab that mediates ADCC but not CDC. Similar results have recently been reported by another group using a similar adenoviral vector strategy [27].
In addition to these classical immune functions, the antibodies induced by Ad-HER2-ki had potent antiproliferative effects on HER2-expressing tumor cells [28]. Similar results had previously been reported in animals and in human cancer patients (unpublished data) [29, 30]. We hypothesized that this antiproliferative effect might be due to receptor downregulation and subsequently demonstrated that the HER2-vaccine induced antibodies within serum produced significant receptor internalization that did not occur when tumor cells were treated with trastuzumab, distinguishing the polyclonal serum antibodies from conventional monoclonal antibody approaches (Fig. 1). We and others have observed that HER2 receptor internalization is not a function of trastuzumab [31–33]. Combining two monoclonal antibodies targeting different epitopes on HER2 has been observed to cause HER2 internalization [32, 34], and there is other evidence that supports the contention that multiple antibodies to different epitopes are more efficient at internalizing receptors [34–37]. We have identified 14 epitopes recognized by the HER2-vaccine-induced antibodies [26]. The importance of the internalization lies in the possibility that internalized receptors may meet one of two fates, either being recycled to the cell surface or degraded. Receptors recycled to the cell surface may continue to stimulate tumor growth, while receptor degradation would block growth factor signaling and clearly be the more desirable outcome for an antitumor strategy. There is also the possibility that receptor degradation may lead to more efficient antigen presentation to promote T-cell responses against tumors cells expressing the receptor.
Binding of HER2-VIA results in HER2 receptor internalization. Human HER2+ breast cancer cells (SKBR3) were stained with DAPI (nuclear stain, blue) and an anti-HER2 MAb (red). Cells were then incubated with HER2-VIA from Ad-HER2 vaccinated mice for 5 min (Upper panel) or 2 h (lower panel) and then visualized by fluorescence microscopy
Finally, because the monoclonal HER2 targeting antibody trastuzumab synergizes with lapatinib, we tested whether vaccine-induced antibodies induced by vaccinations against HER2 would synergize with lapatinib in vitro and whether combining lapatinib and Ad-HER2-ki immunization would lead to enhanced control of breast tumors in vivo. Our results establish that the combination was superior to either agent alone in vitro and in vivo. Although lapatinib and HER2-VIA target the same molecule, their effects on signaling are different. Alone, the HER2-vaccine induced antibodies had their greatest effect on HER2 protein levels. As expected, lapatinib interrupted signaling through HER2 and thus the phosphorylation of downstream molecules. The combination of the two reagents resulted additionally in a reduction in levels of the anti-apoptotic protein survivin, which would result in enhanced tumor cell apoptosis. Thus, although combining lapatinib and trastuzumab has shown favorable clinical results [38], it is possible that the combination of lapatinib and a polyclonal anti-HER2 antibody response induced by vaccination will be superior because of the additional effects provided by polyclonal antibodies over a monoclonal antibody targeting a single epitope. It is also intriguing that lapatinib treatment can lead to stabilization and accumulation of HER2, enhancing trastuzumab-mediated cytotoxicity [39]. We expect similarly that it will potentiate the activity of vaccines targeting HER2.
The potential benefits of a vaccine strategy over a monoclonal antibody approach, with the induction of both T-cell and polyclonal antibody responses, and multiple mechanisms of action resulting from polyclonal antibody induction, encourage the use of vaccine strategies. And there is increasing evidence that cancer vaccines can improve patient survival, renewing enthusiasm for cancer vaccine approaches. [40–43]. The synergy seen with the vaccine plus lapatinib suggests that their use in combination should also be evaluated clinically. And we will initiate this clinical study in the next 12 months. More broadly, we believe our results suggest that targeting receptor molecules using vaccines as a means to perturb signaling offers new opportunities to target cancer beyond the conventional lytic killing of cancer cells by the immune system.
The therapeutic potential of polyclonal immune responses to other cancer signaling antigens- HER3
Cancer immunotherapy has most often targeted antigens preferentially if not exclusively expressed by cancer cells. Due to the chronic nature of the progression of cells from pre-invasive to invasive and then metastatic disease, the long-term expression of tumor antigens in the absence of appropriate costimulation can be associated with immunologic unresponsiveness [44]. Strategies that overcome this antigen-specific unresponsiveness appear clinically promising including treatment with anti-CTLA4 antibodies [45–48]. An alternative strategy would be to target antigens that are not constitutively overexpressed by tumor cells but, rather, are rapidly induced in response to therapeutic interventions. Therapeutic resistance, either intrinsic or acquired following an initial period where a patients’ cancer is responsive to the therapy, is a major obstacle to effective and sustained cancer treatment. It is almost universally true that despite sometimes impressive clinical results with kinase-targeted therapies, clinical experience dictates that most, if not all, treatment-responsive patients will eventually experience relapse as a result of acquired drug resistance [17, 18]. We hypothesize that these induced antigens would represent ideal antigens to target by vaccination, as their acute expression would not be associated with immunologic unresponsiveness.
One such example is the overexpression of HER3 as a mechanism of induced resistance to EGFR- and HER2-targeted therapies [49–51]. Although HER3 itself is not a tractable target for small-molecule drug approaches because it lacks intrinsic tyrosine kinase activity, alternative approaches can be considered to ablate its signaling effects, either alone or as a potent heterodimer formed with EGFR or ERB2. One such alternative is the active immunization targeting HER3, which we have recently demonstrated generates HER3-specific immune responses that have antitumor effects in vivo and in vitro (manuscript in preparation).
Thus, we believe that antigens that are upregulated by tumors in response to therapy represent a particularly good target for a cancer vaccine strategy.
Resistance to immune-mediated killing by T cells
Despite the utility demonstrated in experimental animal models, the application of this strategy must address shortcomings in current clinical cancer vaccine technologies. Although the benefits of therapeutic vaccination with autologous dendritic cells have been recently demonstrated, new technologies and insight into the requirements for inducing clinically relevant adaptive immune response provide an opportunity for use to improve the potency of cancer vaccines. For example, in tumor types that are refractory to conventional chemotherapy, immune effector cells remain highly capable to inducing killing when directed toward tumor cells. We demonstrated that metastatic human colorectal cancer (CRC) previously treated with conventional chemotherapy would be sensitive to T-cell killing mediated by carcinoembryonic antigen (CEA)/CD3-bispecific T-cell-engaging BiTE antibody (MEDI-565) [52]. We analyzed proliferation and lysis of CEA-positive (CEA+) CRC specimens that had survived previous systemic chemotherapy and biologic therapy to determine whether they could be killed by patient T cells engaged by MEDI-565 in vitro. At low concentrations (0.1–1 ng ml(−1)), MEDI-565+ T cells caused reduced proliferation and enhanced apoptosis of CEA+ human CRC specimens. High levels of soluble CEA did not impair killing by redirected T cells, and there was no increase in resistance to T-cell killing despite multiple rounds of exposure. This study shows for the first time that metastatic CRC specimens derived from patients previously treated with conventional chemotherapy can be lysed by patient T cells.
Antigen discovery
In addition to well-known tumor antigens, other antigens are being identified in subsets of common tumors, and there is increasing interest in their utility, particularly if they are in tumor subsets with a particularly poor prognosis. For example, cell surface proteoglycan, chondroitin sulfate proteoglycan 4 (CSPG4), is a potential target for monoclonal antibody–based immunotherapy for many types of cancer [53]. The lack of effective therapy for triple-negative breast cancer (TNBC) prompted us to examine whether CSPG4 is expressed in TNBC and can be targeted with CSPG4-specific mAb. CSPG4 protein expression was assessed in 44 primary TNBC lesions, in TNBC cell lines HS578T, MDA-MB-231, MDA-MB-435, and SUM149, and in tumor cells in pleural effusions from metastatic breast cancer patients. CSPG4 protein was preferentially expressed in 32 of the 44 (72.7%) primary TNBC lesions tested, in TNBC cell lines, and in tumor cells in pleural effusions from 12 metastatic breast cancer patients.
The effect of CSPG4-specific mAb 225.28 on growth, adhesion, and migration of TNBC cells was tested in vitro. CSPG4-specific mAb 225.28 statistically significantly inhibited growth, adhesion, and migration of TNBC cells in vitro. mAb 225.28 induced 73.1% regression of tumor metastasis in a TNBC cell–derived experimental lung metastasis model (mAb 225.28 vs. control, mean area of metastatic nodules = 44590.8 vs 165950.8 μm(2); difference of mean = 121360.0 μm(2), 95% confidence interval = 91010.7 to 151709.4 μm(2); P < 0.001). Additionally, mAb 225.28 statistically significantly reduced spontaneous lung metastases and tumor recurrences in an orthotopic xenograft mouse model. The mechanisms responsible for antitumor effect included increased apoptosis and reduced mitotic activity in tumor cells, decreased blood vessel density in the tumor microenvironment, and reduced activation of signaling pathways involved in cell survival, proliferation and metastasis.
This study identified CSPG4 as a new target for TNBC. The antitumor activity of CSPG4-specific mAb was mediated by multiple mechanisms, including the inhibition of signaling pathways crucial for TNBC cell survival, proliferation, and metastasis.
New cancer vaccine strategies in clinical trials at duke
In addition to the recent activities in identifying important new antigens, improvement in antigen delivery for vaccination has occurred. For example, potent recombinant viral vectors have been clinically suboptimal due to the presence of neutralizing vector-specific immune response. One alternative is the use of next-generation vectors that can immunize in the setting of pre-existing vector immunity. A specific example involves the first-generation recombinant serotype 5 adenovirus (Ad5) vectors that lack E1 expression and induce robust immune responses against encoded transgenes in pre-clinical models but have muted responses in human trials because of widespread pre-existing anti-adenovirus immunity. Attempts to circumvent Ad5-specific immunity by using alternative serotypes or modifying capsid components have not yielded profound clinical improvement. To address this issue, we explored a novel alternative strategy, specifically reducing the expression of structural Ad5 genes by creating E1 and E2b deleted recombinant Ad5 vectors. We demonstrated that [E1-, E2b-]vectors retaining the Ad5 serotype are potent immunogens in pre-clinical models despite the presence of significant Ad5-specific immunity, in contrast to [E1-] vectors [54].
We extended these observations to pre-clinical models of cancer immunotherapy. A vector containing the carcinoembryonic antigen (CEA) gene insert was constructed to induce cell-mediated immunity (CMI) against the tumor-associated target and the CEA immunogenicity, and in vivo antitumor effects of repeated immunizations with Ad5 [E1-, E2b-]-CEA compared with those observed with current generation Ad5 [E1-]-CEA were tested in Ad5 pre-immunized mice. We demonstrated that Ad5-immune mice immunized multiple times with Ad5 [E1-, E2b-]-CEA induced CEA-specific CMI responses that were significantly increased over those detected in Ad5-immune mice immunized multiple times with a current generation Ad5 [E1-]-CEA. Ad5 immune mice bearing CEA-expressing tumors that were treated with Ad5 [E1-, E2b-]-CEA had increased antitumor response when compared with Ad5 [E1-]-CEA-treated mice. These results demonstrate that Ad5 [E1-, E2b-]-CEA can induce antigen-specific immune responses that result in tumor growth inhibition despite the presence of pre-existing Ad5 immunity. These results have lead to an ongoing phase I clinical testing this viral construct in patients with advanced colorectal cancers that express CEA. An important endpoint of this study will be whether immune responses may be induced in patients with high titer anti-Ad antibodies [55].
Although adenoviral vectors have been a mainstay in gene transfer studies, even more novel vector systems can be generated with properties that exploit the role of dendritic cells to present antigen. One approach is to use a viral vector to deliver antigen to in situ DCs, which then activate tumor-specific T-cell and antibody responses. However, vector-specific neutralizing antibodies and suppressive cell populations such as Tregs remain great challenges to the efficacy of this approach. We constructed a novel alphavirus vector that expressed CEA, and demonstrated that it, packaged in virus-like replicon particles (VRP), was capable of efficiently infecting DCs, could be repeatedly administered to patients with metastatic cancer expressing the tumor antigen carcinoembryonic antigen (CEA) and that it overcame high titers of neutralizing antibodies and elevated Treg levels to induce clinically relevant CEA-specific T-cell and antibody responses [56]. The CEA-specific antibodies mediated antibody-dependent cellular cytotoxicity against tumor cells from human colorectal cancer metastases. In addition, patients with CEA-specific T-cell responses exhibited longer overall survival. These data suggest that VRP-based vectors can overcome the presence of neutralizing antibodies to break tolerance to self-antigen and may be clinically useful for immunotherapy in the setting of tumor-induced immunosuppression.
New cancer vaccine strategies
We can also improve immunogenicity by enhancing the innate and adaptive responses by augmenting the activation signals to antigen-presenting cells. For example, although critical for initiating and regulating immune responses, the therapeutic use of individual cytokines as anticancer immunotherapeutic agents has achieved only modest clinical success. Consequently, many current strategies have focused on the use of specific immunotherapeutic agonists that engage individual receptors of innate immune networks, such as the Toll-like receptor (TLR) system, each resulting in specific patterns of gene expression, cytokine production, and inflammatory outcome. However, these immunotherapeutics are constrained by variable cellular TLR expression and responsiveness to particular TLR agonists, as well as the specific cellular context of different tumors. We demonstrated that overexpression of MyD88, a pivotal regulator of multiple TLR signaling pathways, could circumvent these constraints and mimic coordinated TLR signaling across all cell types in a ligand-independent fashion [57, 58]. We generated an adenoviral vector expressing MyD88 and show that Ad-MyD88 infection elicits extensive Th1-specific transcriptional and secreted cytokine signatures in all murine and human cell types tested in vitro and in vivo. Importantly, in vivo intratumoral injection of Ad-MyD88 into established tumor masses enhanced adaptive immune responses and inhibited local tumor immunosuppression, resulting in significantly inhibited local and systemic growth of multiple tumor types. Finally, Ad-MyD88 infection of primary human dendritic cells, tumor-associated fibroblasts, and colorectal carcinoma cells elicited significant Th1-type cytokine responses, resulting in enhanced tumor cell lysis and expansion of human tumor antigen-specific T cells. Thus, Ad-MyD88 initiated robust antitumor activity in established murine tumor microenvironments and in human contexts, suggesting its potential effectiveness as a clinical immunotherapeutic strategy.
Approaches to overcoming the immunosuppressive tumor microenvironment
Finally, despite the advances in antigen identification, antigen delivery, and enhancement in immunogenicity, we need to explore strategies to overcome the profound suppressive tumor microenvironment (TME) and Treg population found in cancer patients that diminish antitumor immunity. Impairment of dendritic cells (DC), the most effective activators of anticancer immune responses, is one mechanism for defective antitumor immunity, but the causes of DC impairment are incompletely understood. We evaluated the association of impaired DC differentiation with angiogenesis-associated molecules D-dimer, vascular endothelial growth factor (VEGF), urokinase plasminogen activator (uPA), and plasminogen activator inhibitor (PAI-1) in peripheral blood from 41 patients with lung, breast, and colorectal carcinoma. Subsequently, we studied the effect of administration of the anti-VEGF antibody (bevacizumab) on DC maturation and function in vivo [59, 60]. Compared with healthy volunteers, cancer patients had a bias toward the immunoregulatory DC2, had deficits in DC maturation after overnight in vitro culture, and had a significant increase in immature myeloid cell progenitors of DC (0.50 ± 0.31% vs. 0.32 ± 0.16% of peripheral blood mononuclear cells, respectively, P = 0.011). A positive correlation was found between the percentage of DC2 and PAI-1 (R = 0.50) and between immature myeloid cells and VEGF (R = 0.52). Bevacizumab administration to cancer patients was associated with a decrease in the accumulation of immature progenitor cells (0.39 ± 0.30% vs. 0.27 ± 0.24%, P = 0.012) and induced a modest increase in the DC population in peripheral blood (0.47 ± 0.23% vs. 0.53 ± 0.30%). Moreover, anti-VEGF antibody treatment enhanced allo-stimulatory capacity of DC and T-cell proliferation against recall antigens. These data suggest that DC differentiation is negatively associated with VEGF levels and may be one explanation for impaired anticancer immunity, especially in patients with advanced malignancies.
VEGF is increasingly emerging as a central player in the activity of immunosuppressive cell types that have been shown to be a major factor in the immunosuppressive TME, including specific subsets of TAMs (reviewed in:[61–63]) and MDSC (reviewed in: [64–66]). TAMs have diverse immunosuppressive functions including inhibition of CTL function and influencing the influx of Treg into the TME. MDSC are related to TAMs but represent a distinct and diverse population of myeloid cells based on phenotypic markers and gene expression studies. MDSC suppress innate and adaptive immune responses, affecting T-, NK, and NKT cell function and blocking DC maturation. Both TAMs and MDSC are associated with the onset of resistance to anti-VEGF therapies.
Some therapeutic strategies are focused on enhancing maturation of MDSC precursors into mature myeloid cells and thus avoiding the suppressive effects of accumulating MDSC (reviewed in: [67]). Therapeutic strategies to bias macrophages to a more M1/antitumor macrophage population are also being studied, including blockade of the macrophage CSF1R [68, 69]. An alternate strategy is to block the development of MDSC and TAMs from their precursors by targeting VEGF. Using an anti-VEGF strategy is appealing for a number of reasons, including that it will starve the tumor blood supply as well as potentially reverse immunosuppression by MDSC and TAMS and thereby enhance immune function. Multiple studies have shown that VEGF plays a role in DC dysfunction in cancer patients and has led to studies targeting VEGF [60]. For example, Manning et al. [70] showed that an anti-VEGF MAb was able to trigger antitumor immunity in mice. However, Gabrilovich and colleagues have reported that although an anti-VEGF therapy in cancer patients improved the differentiation of dendritic cells, it alone was not sufficient to induce antitumor immunity [71]. These findings suggest that an anti-VEGF strategy might enhance the response to a cancer vaccine in patients. To date, there has been only a single clinical study combining a cancer vaccine with avastin and that study showed the vaccine could elicit immune responses and modulate PSA levels in patients with biochemically recurrent prostate cancer, despite the negative effects of avastin on DC function [72]. Further studies are warranted.
Another major factor that hampers the use of cancer vaccines to elicit clinically effective antitumor immunity are CD4(+)CD25(high)FoxP3(+) regulatory T (Treg) cells [73]. To directly address the role of regulatory T cells, we have performed clinical trials depleting human Tregs during cancer immunotherapy. In preclinical and clinical studies, we assessed the immune consequences of FoxP3(+) Treg-cell depletion in patients with advanced malignancies [74]. We demonstrated that a CD25(high) targeting immunotoxin (denileukin diftitox) depleted FoxP3(+) Treg cells, decreased Treg-cell function, and enhanced antigen-specific T-cell responses in vitro. We then attempted to enhance antitumor immune responses in patients with carcinoembryonic antigen (CEA)-expressing malignancies by Treg-cell depletion. In a pilot study (n = 15), denileukin diftitox, given as a single dose or repeated dosing, was followed by immunizations with dendritic cells modified with the fowlpox vector rF-CEA(6D)-TRICOM. By flow cytometric analysis, we report the first direct evidence that circulating CD4(+)CD25(high)FoxP3(+) Treg cells are depleted after multiple doses of denileukin diftitox. Earlier induction of, and overall greater exposure to, the T-cell response to CEA was observed in the multiple-dose group, but not the single-dose group. These results indicate the potential for combining Treg-cell depletion with anticancer vaccines to enhance tumor antigen-specific immune responses and the need to explore dose and schedule of Treg depletion strategies in optimizing vaccine efforts. Alternative approaches to modulate Treg levels include cyclophosphamide (Cy) [75], and recent data also suggest that letrozole has effects on Treg [76]. One report has compared ONTAK and Cy and suggested that while Cy mediated double the reduction in Treg numbers when compared to ONTAK, only Cy had a negative impact on other T-cell subsets and resulted in a lack of effective T-cell priming [77], and we have observed similar effects using the predominant active Cy metabolite 4- hydroxycyclphosphamide (unpublished).
In addition to regulatory T cells, other “suppressor” cells have been described by us and others [78, 79]. We have identified a subset of CD4+ NKT cells in humans that diminish antigen-specific CD8+ T-cell expansion and are pursuing the biology of these cells in our cancer vaccine studies. And Matsushita et al., have recently reported on B10 cells, a regulatory B-cell subset that plays a role in preventing the onset of EAE in a mouse model but whose role in tumor immunity is yet to be defined. Thus, we face a myriad of different cell types whose suppressive function can impair the effectiveness of cancer vaccines, and it is in the area of immunomodulation to counteract these cells that new approaches are needed to tip the balance in favor of antitumor immunity.
Conclusions
Although a variety of strategies have been employed to prioritize the development of therapeutic strategies directed toward these antigens, the emerging recognition of the role of aberrant signaling in cancer has lead to immunologic therapies, usually monoclonal antibodies targeting critical signaling pathways. Because adaptive immune responses are capable of inducing polyclonal immune effector responses that have different biologic effects than monoclonal antibodies or small molecule kinase inhibitors, we have begun to explore therapeutic vaccine development to antigens associated with these signaling pathways. We have shown that therapeutic cancer vaccines inducing polyclonal adaptive immune responses targeting the Erb family member HER2 have classical and non-classical antitumor effects, and these strategies should be explored to target other antigens associated with signaling pathways critical for survival of tumor cells or resistance mechanisms induced by therapy. More broadly, we are seeking to develop more potent cancer vaccines through the use of new adjuvant strategies with TLR adaptor agonists, new vector platforms that overcome antivector immunity and Treg, and we are developing strategies to overcome the immunosuppressive tumor microenvironment. Collectively, these studies will lead to increasingly better vaccines, and we hope will build on the recent success of Provenge, which was the first cancer vaccine to be approved by the FDA and represents a new class of anticancer therapy.
References
Kantoff PW, et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28(7):1099–105.
Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;2010:5.
Finn OJ. Cancer immunology. N Engl J Med. 2008;358(25):2704–15.
Kantoff PW, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–22.
Sjoblom T, et al. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314(5797):268–74.
Wood LD, et al. The genomic landscapes of human breast and colorectal cancers. Science. 2007;318(5853):1108–13.
Leary RJ, et al. Integrated analysis of homozygous deletions, focal amplifications, and sequence alterations in breast and colorectal cancers. Proc Natl Acad Sci USA. 2008;105(42):16224–9.
Doyle HA, et al. Isoaspartyl post-translational modification triggers anti-tumor T and B lymphocyte immunity. J Biol Chem. 2006;281(43):32676–83.
Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nat Rev Cancer. 2009;9(1):28–39.
Baselga J, Swain SM. Novel anticancer targets: revisiting ERBB2 and discovering ERBB3. Nat Rev Cancer. 2009;18:18.
Ritter CA, et al. Human breast cancer cells selected for resistance to trastuzumab in vivo overexpress epidermal growth factor receptor and ErbB ligands and remain dependent on the ErbB receptor network. Clin Cancer Res. 2007;13(16):4909–19.
Martin AP, et al. Lapatinib resistance in HCT116 cells is mediated by elevated MCL-1 expression and decreased BAK activation and not by ERBB receptor kinase mutation. Mol Pharmacol. 2008;74(3):807–22.
Paik S, et al. Pathologic findings from the national surgical adjuvant breast and bowel project: prognostic significance of erbB-2 protein overexpression in primary breast cancer. J Clin Oncol. 1990;8(1):103–12.
Slamon DJ, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Xia W, et al. Anti-tumor activity of GW572016: a dual tyrosine kinase inhibitor blocks EGF activation of EGFR/erbB2 and downstream Erk1/2 and AKT pathways. Oncogene. 2002;21(41):6255–63.
Geyer CE, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med. 2006;355(26):2733–43.
Engelman JA, Settleman J. Acquired resistance to tyrosine kinase inhibitors during cancer therapy. Curr Opin Genet Dev. 2008;18(1):73–9.
Nahta R, et al. Mechanisms of disease: understanding resistance to HER2-targeted therapy in human breast cancer. Nat Clin Pract Oncol. 2006;3(5):269–80.
Burris HA 3rd, et al. Phase I safety, pharmacokinetics, and clinical activity study of lapatinib (GW572016), a reversible dual inhibitor of epidermal growth factor receptor tyrosine kinases, in heavily pretreated patients with metastatic carcinomas. J Clin Oncol. 2005;23(23):5305–13.
Emens LA, Reilly RT, Jaffee EM. Breast cancer vaccines: maximizing cancer treatment by tapping into host immunity. Endocr Relat Cancer. 2005;12(1):1–17.
Peoples GE, et al. Clinical trial results of a HER2/neu (E75) vaccine to prevent recurrence in high-risk breast cancer patients. J Clin Oncol. 2005;23(30):7536–45.
Disis ML, et al. Effect of dose on immune response in patients vaccinated with an her-2/neu intracellular domain protein–based vaccine. J Clin Oncol. 2004;22(10):1916–25.
Murray JL, et al. Toxicity, immunogenicity, and induction of E75-specific tumor-lytic CTLs by HER-2 peptide E75 (369–377) combined with granulocyte macrophage colony-stimulating factor in HLA-A2+ patients with metastatic breast and ovarian cancer. Clin Cancer Res. 2002;8(11):3407–18.
Salazar LG, et al. Immunization of cancer patients with HER-2/neu-derived peptides demonstrating high-affinity binding to multiple class II alleles. Clin Cancer Res. 2003;9(15):5559–65.
Disis ML, et al. Generation of T-cell immunity to the HER-2/neu protein after active immunization with HER-2/neu peptide-based vaccines. J Clin Oncol. 2002;20(11):2624–32.
Hartman ZC, et al. An adenoviral vaccine encoding full-length inactivated human Her2 exhibits potent immunogenicty and enhanced therapeutic efficacy without oncogenicity. Clin Cancer Res. 2010;16(5):1466–77.
Triulzi C, et al. Antibody-dependent natural killer cell-mediated cytotoxicity engendered by a kinase-inactive human HER2 adenovirus-based vaccination mediates resistance to breast tumors. Cancer Res. 2010;70(19):7431–41.
Morse MA, et al. Synergism from combined immunologic and pharmacologic inhibition of HER2 in vivo. Int J Cancer. 2009;23:23.
Xia W, et al. Combining lapatinib (GW572016), a small molecule inhibitor of ErbB1 and ErbB2 tyrosine kinases, with therapeutic anti-ErbB2 antibodies enhances apoptosis of ErbB2-overexpressing breast cancer cells. Oncogene. 2005;24(41):6213–21.
Montgomery RB, et al. Endogenous anti-HER2 antibodies block HER2 phosphorylation and signaling through extracellular signal-regulated kinase. Cancer Res. 2005;65(2):650–6.
Longva KE, et al. Herceptin-induced inhibition of ErbB2 signaling involves reduced phosphorylation of Akt but not endocytic down-regulation of ErbB2. Int J Cancer. 2005;116(3):359–67.
Hommelgaard AM, Lerdrup M, van Deurs B. Association with membrane protrusions makes ErbB2 an internalization-resistant receptor. Mol Biol Cell. 2004;15(4):1557–67.
Austin CD, et al. Endocytosis and sorting of ErbB2 and the site of action of cancer therapeutics trastuzumab and geldanamycin. Mol Biol Cell. 2004;15(12):5268–82.
Friedman LM, et al. Synergistic down-regulation of receptor tyrosine kinases by combinations of mAbs: implications for cancer immunotherapy. Proc Natl Acad Sci USA. 2005;102(6):1915–20.
Roepstorff K, et al. Endocytic downregulation of ErbB receptors: mechanisms and relevance in cancer. Histochem Cell Biol. 2008;129(5):563–78.
Kirisits A, Pils D, Krainer M. Epidermal growth factor receptor degradation: an alternative view of oncogenic pathways. Int J Biochem Cell Biol. 2007;39(12):2173–82.
Spangler JB, et al. Combination antibody treatment down-regulates epidermal growth factor receptor by inhibiting endosomal recycling. Proc Natl Acad Sci USA. 2010;107(30):13252–7.
J O’Shaughnessy, KLB, H Burstein, AM Storniolo, G Sledge, J Baselga, M Koehler, S Laabs, A Florance, D Roychowdhury, A randomized study of lapatinib alone or in combination with trastuzumab in heavily pretreated HER2+ metastatic breast cancer progressing on trastuzumab therapy. J Clin Oncol. 2008; 26(May 20 suppl): abstr 1015.
Scaltriti M, et al. Lapatinib, a HER2 tyrosine kinase inhibitor, induces stabilization and accumulation of HER2 and potentiates trastuzumab-dependent cell cytotoxicity. Oncogene. 2009;28(6):803–14.
Schlom J, Gulley JL, Arlen PM. Paradigm shifts in cancer vaccine therapy. Exp Biol Med (Maywood). 2008;233(5):522–34.
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. IMPACT Study Investigators. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–22.
Disis ML et al. Cellular immune parameters associated with improved long-term survival in advanced stage breast cancer patients after active immunization with a HER2-specific vaccine. 2008; p. 3015.
Morse MA, et al. Long Term Disease-Free Survival and T Cell and Antibody Responses in Women with High-Risk HER2+ Breast Cancer Following Vaccination Against HER2+. J Transl Med. 2007;5(1):42.
Pardoll D, Pardoll DM. Does the immune system see tumors as foreign or self?. Spinning molecular immunology into successful immunotherapy. Annu Rev Immunol. 2003;21(4):807–39.
Yuan J, et al. CTLA-4 blockade enhances polyfunctional NY-ESO-1 specific T cell responses in metastatic melanoma patients with clinical benefit. Proc Natl Acad Sci USA. 2008;105(51):20410–5.
Peggs KS, et al. Principles and use of anti-CTLA4 antibody in human cancer immunotherapy. Curr Opin Immunol. 2006;18(2):206–13.
Agarwala SS, Ribas A. Current experience with CTLA4-blocking monoclonal antibodies for the treatment of solid tumors. J Immunother. 2010;33(6):557–69.
Ribas A, et al. Dendritic cell vaccination combined with CTLA4 blockade in patients with metastatic melanoma. Clin Cancer Res. 2009;15(19):6267–76.
Sergina NV, et al. Escape from HER-family tyrosine kinase inhibitor therapy by the kinase-inactive HER3. Nature. 2007;445(7126):437–41.
Lee-Hoeflich ST, et al. A central role for HER3 in HER2-amplified breast cancer: implications for targeted therapy. Cancer Res. 2008;68(14):5878–87.
Amin DN, Campbell MR, Moasser MM. The role of HER3, the unpretentious member of the HER family, in cancer biology and cancer therapeutics. Semin Cell Dev Biol. 2010;21:944–50.
Osada T, et al. Metastatic colorectal cancer cells from patients previously treated with chemotherapy are sensitive to T-cell killing mediated by CEA/CD3-bispecific T-cell-engaging BiTE antibody. Br J Cancer. 2009;102(1):124–33.
Wang X, et al. CSPG4 protein as a new target for the antibody-based immunotherapy of triple-negative breast cancer. J Natl Cancer Inst. 2010;2010:17.
Osada T, et al. Optimization of vaccine responses with an E1, E2b and E3-deleted Ad5 vector circumvents pre-existing anti-vector immunity. Cancer Gene Ther. 2009;20:20.
Gabitzsch ES, et al. Anti-tumor immunotherapy despite immunity to adenovirus using a novel adenoviral vector Ad5 [E1-, E2b-]-CEA. Cancer Immunol Immunother. 2010;59(7):1131–5.
Morse MA, et al. An alphavirus vector overcomes the presence of neutralizing antibodies and elevated numbers of Tregs to induce immune responses in humans with advanced cancer. J Clin Invest. 2010;120(9):3234–41.
Hartman ZC, et al. Ligand-independent toll-like receptor signals generated by ectopic overexpression of MyD88 generate local and systemic antitumor immunity. Cancer Res. 2010;70(18):7209–20.
Hartman ZC, et al. Adenovirus infection triggers a rapid, MyD88-regulated transcriptome response critical to acute-phase and adaptive immune responses in vivo. J Virol. 2007;81(4):1796–812.
Osada T, et al. The effect of anti-VEGF therapy on immature myeloid cell and dendritic cells in cancer patients. Cancer Immunol Immunother. 2008;10:10.
Johnson B, et al. Physiology and therapeutics of vascular endothelial growth factor in tumor immunosuppression. Curr Mol Med. 2009;9(6):702–7.
Allavena P, et al. The Yin-Yang of tumor-associated macrophages in neoplastic progression and immune surveillance. Immunol Rev. 2008;222:155–61.
Ostrand-Rosenberg S. Immune surveillance: a balance between protumor and antitumor immunity. Curr Opin Genet Dev. 2008;18(1):11–8.
Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51.
Nagaraj S, Gabrilovich DI. Tumor escape mechanism governed by myeloid-derived suppressor cells. Cancer Res. 2008;68(8):2561–3.
Ostrand-Rosenberg S. Myeloid-derived suppressor cells: more mechanisms for inhibiting antitumor immunity. Cancer Immunol Immunother. 1593;59(10):1593–600.
Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9(3):162–74.
Ugel S, et al. Therapeutic targeting of myeloid-derived suppressor cells. Curr Opin Pharmacol. 2009;9(4):470–81.
Priceman SJ, et al. Targeting distinct tumor-infiltrating myeloid cells by inhibiting CSF-1 receptor: combating tumor evasion of antiangiogenic therapy. Blood. 2010;115(7):1461–71.
Conway JG, et al. Inhibition of colony-stimulating-factor-1 signaling in vivo with the orally bioavailable cFMS kinase inhibitor GW2580. Proc Natl Acad Sci U S A. 2005;102(44):16078–83.
Manning EA, et al. A vascular endothelial growth factor receptor-2 inhibitor enhances antitumor immunity through an immune-based mechanism. Clin Cancer Res. 2007;13(13):3951–9.
Fricke I, et al. Vascular endothelial growth factor-trap overcomes defects in dendritic cell differentiation but does not improve antigen-specific immune responses. Clin Cancer Res. 2007;13(16):4840–8.
Rini BI, et al. Combination immunotherapy with prostatic acid phosphatase pulsed antigen-presenting cells (provenge) plus bevacizumab in patients with serologic progression of prostate cancer after definitive local therapy. Cancer. 2006;107(1):67–74.
Nishikawa H, Sakaguchi S. Regulatory T cells in tumor immunity. Int J Cancer. 2010;127(4):759–67.
Morse MA, et al. Depletion of human regulatory T cells specifically enhances antigen-specific immune responses to cancer vaccines. Blood. 2008;112(3):610–8.
Lutsiak ME, et al. Inhibition of CD4(+)25+ T regulatory cell function implicated in enhanced immune response by low-dose cyclophosphamide. Blood. 2005;105(7):2862–8.
Generali D, et al. Immunomodulation of FOXP3+ regulatory T cells by the aromatase inhibitor letrozole in breast cancer patients. Clin Cancer Res. 2009;15(3):1046–51.
Matsushita N, et al. Comparative methodologies of regulatory T cell depletion in a murine melanoma model. J Immunol Methods. 2008;333(1–2):167–79.
Osada T, et al. Ex vivo expanded human CD4+ regulatory NKT cells suppress expansion of tumor antigen-specific CTLs. Int Immunol. 2005;17(9):1143–55.
Matsushita T, et al. Regulatory B cells (B10 cells) and regulatory T cells have independent roles in controlling experimental autoimmune encephalomyelitis initiation and late-phase immunopathogenesis. J Immunol. 2010;185(4):2240–52.
Jonker DJ, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007;357(20):2040–8.
Douillard JY, et al. Randomized, phase iii trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010;28:4697–705.
Cohen MH, et al. United States food and drug administration drug approval summary: gefitinib (ZD1839; Iressa) tablets. Clin Cancer Res. 2004;10(4):1212–8.
Leget GA, Czuczman MS. Use of rituximab. the new FDA-approved antibody. Curr Opin Oncol. 1998;10(6):548–51.
Hurwitz H, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–42.
Llovet JM, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90.
Motzer RJ, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–24.
Acknowledgments
This work was supported by grants from the National Cancer Institute [NCI P50 CA89496-01 and 5P50CA068438 to HKL, NCI R01 CA95447 to TMC]; Department of Defense Breast Cancer Research Program Clinical Translational Research Award [BC050221 to TMC]; and Susan G. Komen for the Cure Awards [HKL and Postdoctoral Fellowship Award KG080627 to ZCH].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clay, T.M., Osada, T., Hartman, Z.C. et al. Polyclonal immune responses to antigens associated with cancer signaling pathways and new strategies to enhance cancer vaccines. Immunol Res 49, 235–247 (2011). https://doi.org/10.1007/s12026-010-8186-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-010-8186-6