Abstract
Frank’s sign (named after American pulmonologist Sanders T. Frank) refers to a diagonal skin fold between the tragus and outer edge of the earlobe. Gradation is based on the bilateral presence and/or degree of the earlobe fold. The presence of this sign, referred to as the diagonal earlobe crease (DELC), has been associated with coronary artery disease (CAD), independent of other cardiovascular risk factors. Corresponding studies are predominantly based on clinical or angiographic assessments, and few autopsy studies exist. The association of DELC with CAD, cardiovascular risk factors, and causes of death was investigated via retrospective and prospective evaluations. It was also investigated whether the degree of DELC correlated with the macroscopic severity of coronary heart disease. Furthermore, the influence of age on the appearance of DELC was analyzed and compared using two age groups. Additionally, binomial logistic regression analysis was performed to investigate the influence of age on the presence of higher-grade DELC and CAD. In cases related to a lethal cardiac event, the majority (78%) showed high-grade DELC. The DELC grade correlated significantly with CAD severity (rs = 0.474, p < 0.001) and with the severity of general atherosclerosis (rs = 0.606, p < 0.001) with medium and large effects sizes, respectively. Age was predominantly more suitable than DELC concerning the sensitivity, specificity, and positive prognostic value for preexisting cardiac disease and cardiac-related causes of death. In both DELC and CAD, age has a significant influence on the presence of higher-grade manifestation, but the influence of age in CAD appears to be even more significant than in DELC. The main results of previous autopsy studies and the prognostic value could have been confirmed, but these findings appear to be limited to younger patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Frank sign was first established in 1973 by American pulmonologist Sanders T. Frank to describe a unilateral or bilateral diagonal fold of skin between the tragus and outer edge of the earlobe, which is also called a diagonal earlobe crease (DELC) [1]. Gradation may be based on the bilateral occurrence and/or degree of the earlobe crease (Fig. 1). Grade 1 is a slight wrinkling of the skin around the earlobe. Grade 2a involves a superficial skin fold that partially covers the earlobe at least halfway; grade 2b involves a superficial skin fold that covers the earlobe completely. Grade 3 involves a deep skin fold that covers the entire earlobe [2]. Frank described a correlation between the occurrence of this skin fold and the presence of coronary heart disease [1]. This correlation is assumed to exist because both the earlobe and heart are supplied by “end arteries” and therefore lack collateral circulation. Another assumption is that the general loss of elastin and elastic fibers observed in biopsy specimens from the earlobes reflects the presence of microvascular disease in the coronary arteries [3,4,5].
Since its first description by Frank, various studies have confirmed the association between a DELC and coronary heart disease [6,7,8,9,10,11,12] as well as an association with increased cardiac morbidity and mortality [13]. In 1996, Elliott and Powell postulated a relative risk for a cardiac event for a unilateral earlobe crease of 1.33 and a bilateral earlobe crease of 1.77 [14]. The occurrence of a DELC is reported be more common in patients with myocardial infarction than in patients without myocardial infarction [15, 16]. However, the occurrence of a DELC in association with coronary artery disease (CAD) has been reported to be influenced by the individual’s age, as noted by Mehta and Hamby in 1974 [17]. Since then, several studies have denied the association between a DELC and atherosclerotic disease, proposing that it is simply a phenomenon of age [18,19,20].
An important consideration is that these studies were based mainly on clinical or angiographic assessments, and few autopsy studies have been conducted [2, 21,22,23,24]. In this study, the associations between the degree of Frank’s sign with cardiovascular diseases and cardiac-related causes of death in the context of forensic autopsies were investigated, and their prognostic values were compared based on the age of the deceased.
Materials and methods
We conducted retrospective and prospective evaluations of photographic material obtained from the Institute of Legal Medicine of the University Hospital Bonn between January 2015 and April 2020. Inclusion criteria included cases that had clearly assessable images of at least one earlobe. Exclusion criteria were cases with putrefaction, anasarca, the presence of earrings, and/or a generally strong skin wrinkling of the head and facial regions.
Macroscopically visible alterations of the coronary and main arteries of the body on postmortem examination were estimated and classified into four grades: grade 1: fatty deposits in the vessels without calcification; grade 2: calcification without stenosis; grade 3: calcification with moderate stenosis (< 70% in a major coronary vessel or main artery); and grade 4: calcification with significant (> 70% in a major coronary vessel or main artery) or complete stenosis. A preexisting cardiac disease was assumed when a CAD grade ≥ 3, ventricular hypertrophy, cardiomyopathies, and/or previous myocardial infarction was present.
To determine the prognostic value of Frank’s sign, we divided the collective into two groups with either low grade (grade up to 2a) or high grade DELC (grade higher than 2b) and carried out Student’s t-tests for two independent samples using a 95% confidence interval. In the next step, we divided the collective into two groups based on their age to evaluate the influence on the appearance of the DELC. Based on the median age calculated, we formed one group with age < 63 years and the other with age ≥ 63 years. We also tested the correlation between the DELC grade and CAD degree, atherosclerosis, heart weight, visible preexisting cardiac diseases during autopsy, and cardiac-related cause of death by using Spearman’s rank correlation coefficient and Cohen’s effect sizes (0.10 = small, 0.30 = medium, 0.50 = large). In addition, we calculated the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for the DELC, and assessed the age of diagnosis of preexisting cardiac disease and cardiac-related cause of death. To examine the influence of age on the presence of higher-grade DELC (above 2b) and CAD (above 2), a binomial logistic regression analysis was performed. Prior to this analysis, the study population was divided into four approximately equal age groups: 1 to 47 years (n = 39), 49 to 62 years (n = 42), 63 to 75 years (n = 43), and 76 to 96 years (n = 41). The age group first mentioned served as a reference.
Results
The study collective comprised 165 deceased persons (115 male, 50 female) with an mean age of 61 years (range 11–96 years, median 63 years, SD 19.01), of which 27 persons (16.3%) had no visible DELC, 12 (7.3%) showed DELC grade 1, 18 showed DELC grade 2a, 53 (32.1%) showed DELC grade 2b, and 55 (33.3%) showed DELC grade 3.
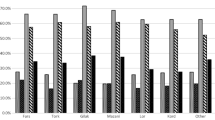
Tables 1 and 2 show the statistical analyses of the two groups divided by the DELC grade and age. Deceased persons with a DELC grade above 2b were significantly older, had a higher heart weight, a higher grade of CAD severity, and atherosclerosis; frequently, they had a preexisting cardiac disease and a cardiac-related cause of death. In comparison, deceased persons older than 63 years of age showed statistically significant differences in the abovementioned variables. Furthermore, the DELC and age showed predominantly medium and large effect sizes, respectively (Table 3).
In 50 of the 165 cases, death was directly or at least partially related to a cardiac event. Regarding those 50 cases, 11 decedents (22%) had no or only low-grade DELC, whereas 39 (78%) had high-grade DELC (grade 2b or 3). In comparison, 14 of the decedents (28%) were younger than 63 years, whereas 36 (72%) were older. The diagnostic values for DELCs and age regarding preexisting cardiac disease and cardiac-related causes of death are displayed in Table 4. The DELC showed a higher sensitivity but a lower specificity for the diagnosis of a preexisting cardiac disease and cardiac-related cause of death compared to age. The DELC and age differed slightly only for the PPV and NPV for these two variables. The binomial logistic regression model was statistically significant for presence of higher-grade DELC (χ2(3) = 42.02, p < 0.001) and CAD (χ2(3) = 49.84, p < 0.001), resulting in an acceptable amount of explained variance (Nagelkerke’s R2 = 0.0309 and 0.351, respectively). Age contributed significantly in predicting the presence of higher-grade DELC as well as CAD (p < 0.001, each). The summary of odds ratios for different age groups is shown in Table 5.
Discussion
The result of this study confirms the association between the occurrence of a DELC and the presence of CAD and general atherosclerosis, as well as a correlation between the respective grades of severity. The DELC was present with a frequency similar to that observed in the autopsy study by Kirkham et al. (72% vs. 84%), yet a cardiovascular cause of death was significantly more frequent in that study (64% vs. 30%) [24]. On the one hand, this may be because the collective age of the study cohort was 10 years older, on average. On the other hand, a substantial proportion of the retrospectively examined collective included cases of deaths due to hanging and strangulation. Cumberland et al. included 800 consecutive autopsies with an average age of 34.8 years. The youngest patient to be identified with an earlobe crease was 27 years of age. It was postulated that there was a statistically significant correlation between the DELC presence and severe stenotic coronary atherosclerosis [21]. In contrast with our study, Cumberland et al. did not grade the DELC, so it was unclear at what severity the DELC presence was affirmed.
In both higher-grade DELC and CAD, age had a significant effect on its presence. However, it was striking that the association between the presence of higher-grade CAD was more than two times higher in the different age groups than in higher-grade DELC. This suggests that although the presence of DELC, like CAD, is age-dependent, age itself has a comparatively significantly higher influence in the presence of CAD.
The sensitivity, specificity, PPV, and NPV for DELCs with a CAD diagnosis were 75.2%, 53.8%, 67.1%, and 63.3%, according to a study of 449 in-hospital cases by Wu et al. [8]. Based on 520 forensic autopsy cases, Edston calculated a sensitivity of 75% and a PPV of 68% for DELC with a CAD diagnosis. The highest PPV was observed in the group of persons aged younger than 40 years [22]. The results of those studies are similar to our calculated DELC values with the diagnosis of a preexisting cardiac disease. Cumberland et al. [21] calculated a sensitivity of 55%, specificity of 83%, PPV of 42%, and NPV of 90% for the DELC and concomitant significant atherosclerosis, and, consequently, a much lower sensitivity as well as a much higher specificity and NPV than those of our findings.
.An autopsy study by Stoyanov et al. which was one of the rare studies that included histological investigations, showed a significant association between the DELC and histopathological changes in the myocardium [25]. In accordance with our results, they observed a significant association between increased heart weight and the presence of a DELC. Furthermore, and in accordance with the results of studies by Patel et al. [2] and Ishii et al. [23], a more severe degree of CAD can be expected in cases of high-grade DELCs. A compilation of these and previously performed autopsy studies is summarized in Table 6.
In conclusion, the main results of previous autopsy studies and, thus, the prognostic value and clinical relevance of the DELC could have been confirmed. Compared to age, the DELC showed a higher sensitivity (79.5% vs. 69.6%) but lower specificity (51.2% vs. 73.2%) and lower PPV (62.3% vs. 72.5%) for preexisting cardiac disease. Its specificity (40.9% vs. 60.9%) and PPV (36.4% vs. 44.4%) were also lower for cardiac-related causes of death.
Conclusion
The DELC and age showed a statistically significant correlation between age, heart weight, CAD, general atherosclerosis, preexisting cardiac disease, and cardiac-related causes of death. Consequently, the occurrence of a DELC must be considered in the context of the individual’s age. In both DELC and CAD, age has a significant influence on the presence of higher-grade manifestation, but the influence of age in CAD appears to be even more significant than in DELC. Therefore, the presence of a DELC seems to be of prognostic value for younger patients especially, and it seems advisable that its presence should be inspected regularly during physical examination. As recently emphasized by Stoyanov et al. [26], a large-scale prospective cohort study is needed to clarify the correlation between DELC and cardiovascular morbidity and its role as a marker for related complications. Such a study, which should also include a sufficiently large number of young subjects, would certainly also be suitable to clarify the influence of age and the correlation between DELC and CAD.
Furthermore, descriptions of the nomenclature and classification of Frank’s sign were inconsistent throughout the different studies. As mentioned earlier, the DELC grade may be based on the bilateral occurrence and/or the degree of the earlobe crease, which can only be affirmed by its presence. A coherent definition of this sign, with respect to the requirements needed for diagnosis, would greatly increase the comparability of the studies conducted on this subject and would help to clarify its prognostic value for cardiovascular and other medical conditions.
Key points
-
1.
Frank’s sign refers to a diagonal earlobe crease (DELC).
-
2.
The presence of Frank’s sign has been associated with coronary artery disease.
-
3.
In cases related to a lethal cardiac event, the majority showed high-grade DELC.
-
4.
DELC grade correlated significantly with severity of CAD and general atherosclerosis.
-
5.
Age has a significant influence on the presence of higher-grade DELC and CAD.
References
Frank ST. Aural sign of coronary-artery disease. N Engl J Med. 1973;289(6):327–8.
Patel V, Champ C, Andrews PS, et al. Diagonal earlobe creases and atheromatous disease. A postmortem study. J R Coll Phys London. 1992;26(3):274–77.
Evrengül H, Dursunoğlu D, Kaftan A, et al. Bilateral diagonal earlobe crease and coronary artery disease. A significant association. Dermatology (Basel, Switzerland). 2004;209(4):271–75. https://doi.org/10.1159/000080847.
Isunado T, Ito I, Katabira Y, Takahashi G. Histological study on the ear-lobe crease (in Japanese) Hihu. 1982;24:352–60.
Lichtstein E, Chapman I, Gupta PK, et al. Letter. Diagonal ear-lobe crease and coronary artery sclerosis. Ann Intern Med. 1976;85(3):337–38. https://doi.org/10.7326/0003-4819-85-3-337.
Kadam Y, Shah Y, Kore P. Diagonal earlobe crease. Prevalence and association with medical ailments. J Clin Prev Cardiol. 2018;7(2):49. https://doi.org/10.4103/JCPC.JCPC_26_17.
Fabijanic D, Miric D, Radic M. The diagonal ear-lobe crease. As sign of some diseases. Saudi Med J. 2006;27(1):130.
Wu X-L, Yang D-Y, Zhao Y-S, et al. Diagonal earlobe crease and coronary artery disease in a Chinese population. BMC Cardiovasc Disord. 2014;14:43. https://doi.org/10.1186/1471-2261-14-43.
Ramos PM, Gumieiro JH, Miot HA. Association between ear creases and peripheral arterial disease. Clinics (Sao Paulo, Brazil). 2010;65(12):1325–7. https://doi.org/10.1590/S1807-59322010001200016.
Pasternac A, Sami M. Predictive value of the ear-crease sign in coronary artery disease. Can Med Assoc J. 1982;126(6):645–9.
Elliott WJ. Ear lobe crease and coronary artery disease. Am J Med. 1983;75(6):1024–32. https://doi.org/10.1016/0002-9343(83)90883-5.
Guţiu I, el Rifai C, Mallozi M. Relation between diagonal ear lobe crease and ischemic chronic heart disease and the factors of coronary risk. Med Inter. 1986;24(2):111–6.
Elliott WJ, Karrison T. Increased all-cause and cardiac morbidity and mortality associated with the diagonal earlobe crease. A prospective cohort study. Am J Med. 1991;91(3):247–54. https://doi.org/10.1016/0002-9343(91)90123-f.
Elliott WJ, Powell LH. Diagonal earlobe creases and prognosis in patients with suspected coronary artery disease. Am J Med. 1996;100(2):205–11. https://doi.org/10.1016/s0002-9343(97)89460-0.
Lichstein E, Chadda KD, Naik D, et al. Diagonal ear-lobe crease. Prevalence and implications as a coronary risk factor. N Eng J Med. 1974;290(11): 615–16. https://doi.org/10.1056/NEJM197403142901109.
Kaukola S. The diagonal ear-lobe crease, a physical sign associated with coronary heart disease. Acta Med Scand Suppl. 1978;619:1–49.
Mehta J, Hamby RI. Letter. Diagonal ear-lobe crease as a coronary risk factor. New Engl J Med. 1974;291(5):260. https://doi.org/10.1056/NEJM197408012910519.
Davis TM, Balme M, Jackson D, et al. The diagonal ear lobe crease (Frank’s sign) is not associated with coronary artery disease or retinopathy in type 2 diabetes. The Fremantle Diabetes Study. Aust N Z J Med. 2000;30(5):573–77. https://doi.org/10.1111/j.1445-5994.2000.tb00858.x.
Kenny DJ, Gilligan D. Ear lobe crease and coronary artery disease in patients undergoing coronary arteriography. Cardiology. 1989;76(4):293–8. https://doi.org/10.1159/000174506.
Gral T, Thornburg M. Earlobe creases in a cohort of elderly veterans. J Am Geriatr Soc. 1983;31(3):134–6. https://doi.org/10.1111/j.1532-5415.1983.tb04851.
Cumberland GD, Riddick L, Vinson R. Earlobe creases and coronary atherosclerosis. The view from forensic pathology. Am J Forensic Med Pathol. 1987;8(1):9–11. https://doi.org/10.1097/00000433-198703000-00003.
Edston E. The earlobe crease, coronary artery disease, and sudden cardiac death. An autopsy study of 520 individuals. Am J Forensic Med Pathol. 2006;27(2):129–33. https://doi.org/10.1097/01.paf.0000221067.73173.d7.
Ishii T, Asuwa N, Masuda S, et al. Earlobe crease and atherosclerosis. An autopsy study. J Am Geriatr Soc. 1990;38(8):871–76. https://doi.org/10.1111/j.1532-5415.1990.tb05702.x.
Kirkham N, Murrells T, Melcher DH, et al. Diagonal earlobe creases and fatal cardiovascular disease. Necropsy Study Br Heart J. 1989;61(4):361–4. https://doi.org/10.1136/hrt.61.4.361.
Stoyanov GS, Dzhenkov D, Petkova L, et al. The histological basis of Frank’s Sign. Head Neck Pathol. 2021;15(2):402–7. https://doi.org/10.1007/s12105-020-01205-4.
Stoyanov GS, Dzhenkov D, Petkova L, et al. Frank’s sign and paired ear creases of the helix. Wien Klin Wochenschr. 2021. https://doi.org/10.1007/s00508-021-01969-x.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prangenberg, J., Doberentz, E., Johann, L. et al. The prognostic value of the Frank sign. Forensic Sci Med Pathol 18, 149–155 (2022). https://doi.org/10.1007/s12024-022-00463-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-022-00463-8