Abstract
Introduction
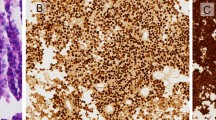
Data on silent corticotroph tumor (SCT) are still heterogeneous and controversial. In this study, we aimed to compare the demographic, clinicopathological manifestations, postoperative complications, and patient outcomes of SCTs with other non-functioning pituitary neuroendocrine tumor (NFT) and functioning corticotroph tumor (FCT) or so-called Cushing disease adenoma.
Methods
We searched PubMed and Web of Science for data of interest. Odds ratio (OR), mean difference (MD), hazard ratio (HR), and their 95% confidence intervals (CI) were pooled using the random-effect model.
Results
Twenty-nine studies with 985 SCTs were included in meta-analyses. In comparison to other NFTs, SCTs were more commonly associated with female gender, younger age, cavernous sinus invasion, apoplexy, and radiotherapy administration. Postoperatively, SCT patients were more likely to experience hypocortisolism, new-onset visual disturbances, and a higher risk for tumor progression than other NFTs. We did not find any significant differences between SCT type I and type II. Compared to FCTs, SCTs were more likely male, older age, and had larger tumor sizes. The prevalence of a USP8 mutation was significantly higher in FCT than in SCT.
Conclusion
SCT was demographically, clinicopathologically, and prognostically distinct from other NFTs and FCTs. These tumors should be considered high-risk; appropriate treatment decisions and more stringent follow-up should be tailored to improve patient outcomes.


Similar content being viewed by others
References
D.N. Louis, A. Perry, P. Wesseling et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 23(8), 1231–1251 (2021)
S.L. Asa, O. Mete, A. Perry, R.Y. Osamura, Overview of the 2022 WHO Classification of Pituitary Tumors. Endocr. Pathol. 33(1), 6–26 (2022)
O. Mete, M.B. Lopes, Overview of the 2017 WHO Classification of Pituitary Tumors. Endocr. Pathol. 28(3), 228–243 (2017)
H. Alahmadi, D. Lee, J.R. Wilson et al. Clinical features of silent corticotroph adenomas. Acta Neurochirurgica 154(8), 1493–1498 (2012)
K.J. Bradley, J.A.H. Wass, H.E. Turner, Non-functioning pituitary adenomas with positive immunoreactivity for ACTH behave more aggressively than ACTH immunonegative tumours but do not recur more frequently. Clin. Endocrinol. 58(1), 59–64 (2003)
H.Y. Cho, S.W. Cho, S.W. Kim, C.S. Shin, K.S. Park, S.Y. Kim, Silent corticotroph adenomas have unique recurrence characteristics compared with other nonfunctioning pituitary adenomas. Clin. Endocrinol. 72(5), 648–653 (2010)
O. Cohen-Inbar, Z.Y. Xu, C.C. Lee et al. Prognostic significance of corticotroph staining in radiosurgery for non-functioning pituitary adenomas: a multicenter study. J. Neuro-Oncol. 135(1), 67–74 (2017)
B.A. Strickland, S. Shahrestani, R.G. Briggs et al. Silent corticotroph pituitary adenomas: clinical characteristics, long-term outcomes, and management of disease recurrence. J. Neurosurg. 135(6), 1706–1713 (2021)
M.B.S. Lopes, The 2017 World Health Organization classification of tumors of the pituitary gland: a summary. Acta Neuropathol. 134(4), 521–535 (2017)
D. Moher, A. Liberati, J. Tetzlaff, D. Altman; PRISMA Group, Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7), e1000097 (2009)
J.F. Tierney, L.A. Stewart, D. Ghersi, S. Burdett, M.R. Sydes, Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8, 16 (2007)
J.P. Higgins, S.G. Thompson, Quantifying heterogeneity in a meta-analysis. Stat. Med. 21(11), 1539–1558 (2002)
G. Akkus, B. Karagun, N.E. Cetinalp et al. Clinical, hormonal, radiological and morphological comparison of patients with clinically evident Cushing’s disease and patients with silent corticotroph cell adenoma. Cukurova Med. J. 45(4), 1720–1732 (2020)
T. Amano, T. Masumoto, D. Watanabe, et al. Differentiation of silent corticotroph pituitary neuroendocrine tumors (PitNETs) from non-functioning PitNETs using kinetic analysis of dynamic MRI. Jpn J Radiol. 2023.
R.L. Batista, E.B. Trarbach, M.D. Marques et al. Nonfunctioning Pituitary Adenoma Recurrence and Its Relationship with Sex, Size, and Hormonal Immunohistochemical Profile. World Neurosurg. 120, E241–E246 (2018)
M. Bujko, P. Kober, J. Boresowicz et al. USP8 mutations in corticotroph adenomas determine a distinct gene expression profile irrespective of functional tumour status. Eur. J. Endocrinol. 181(6), 615–627 (2019)
S. Castellnou, A. Vasiljevic, V. Lapras et al. SST5 expression and USP8 mutation in functioning and silent corticotroph pituitary tumors. Endocr. Connect. 9(3), 243–253 (2020)
O. Cooper, A. Ben-Shlomo, V. Bonert, S. Bannykh, J. Mirocha, S. Melmed, Silent corticogonadotroph adenomas: clinical and cellular characteristics and long-term outcomes. Horm. Cancer 1(2), 80–92 (2010)
A. Garcia-Martinez, A.C. Fuentes-Fayos, C. Fajardo, et al. Differential Expression of MicroRNAs in Silent and Functioning Corticotroph Tumors. J. Clin. Med. 9(6); (2020)
A. Goyal-Honavar, S. Sarkar, H.S. Asha et al. A clinicoradiological analysis of silent corticotroph adenomas after the introduction of pituitary-specific transcription factors. Acta Neurochirurgica 163(11), 3143–3154 (2021)
I.H. Hewedi, W.M. Osman, M.M. El Mahdy, Differential expression of cyclin D1 in human pituitary tumors: relation to MIB-1 and p27/Kip1 labeling indices. J. Egypt Natl Canc Inst. 23(4), 171–179 (2011)
L. Huang, G. Fatterpekar, S. Charles, D. Golub, D. Zagzag, N. Agrawal, Clinical Course and Unique Features of Silent Corticotroph Adenomas. World Neurosurg. 161, E274–E281 (2022)
A.G. Ioachimescu, L. Eiland, V.S. Chhabra et al. Silent Corticotroph Adenomas: Emory University Cohort and Comparison With ACTH-Negative Nonfunctioning Pituitary Adenomas. Neurosurgery 71(2), 296–303 (2012)
A. Jahangiri, J.R. Wagner, M. Pekmezci et al. A comprehensive long-term retrospective analysis of silent corticotrophic adenomas vs hormone-negative adenomas. Neurosurgery 73(1), 8–17 (2013).
S.Z. Jiang, J.Y. Zhu, M. Feng et al. Clinical profiles of silent corticotroph adenomas compared with silent gonadotroph adenomas after adopting the 2017 WHO pituitary classification system. Pituitary 24(4), 564–573 (2021)
D. Kim, C.R. Ku, S.H. Park et al. Clinical Parameters to Distinguish Silent Corticotroph Adenomas from Other Nonfunctioning Pituitary Adenomas. World Neurosurg. 115, E464–E471 (2018)
F. Langlois, D.S.T. Lim, E. Varlamov et al. Clinical profile of silent growth hormone pituitary adenomas; higher recurrence rate compared to silent gonadotroph pituitary tumors, a large single center experience. Endocrine 58(3), 528–534 (2017)
H. Nishioka, N. Inoshita, O. Mete et al. The Complementary Role of Transcription Factors in the Accurate Diagnosis of Clinically Nonfunctioning Pituitary Adenomas. Endocr. Pathol. 26(4), 349–355 (2015)
M. Pawlikowski, J. Kunert-Radek, M. Radek, "Silent"corticotropinoma. Neuro Endocrinol. Lett. 29(3), 347–350 (2008)
L.G. Perez-Rivas, M. Theodoropoulou, F. Ferrau et al. The Gene of the Ubiquitin-Specific Protease 8 Is Frequently Mutated in Adenomas Causing Cushing’s Disease. J. Clin. Endocrinol. Metab. 100(7), E997–E1004 (2015)
R. Reddy, S. Cudlip, J.V. Byrne, N. Karavitaki, J.A. Wass, Can we ever stop imaging in surgically treated and radiotherapy-naive patients with non-functioning pituitary adenoma? Eur. J. Endocrinol. 165(5), 739–744 (2011)
T.R. Smith, M.M. Hulou, K.T. Huang et al. Complications after transsphenoidal surgery for patients with Cushing’s disease and silent corticotroph adenomas. Neurosurg. Focus. 38(2), E12 (2015)
T. Tateno, H. Izumiyama, M. Doi, T. Akashi, K. Ohno, Y. Hirata, Defective expression of prohormone convertase 1/3 in silent corticotroph adenoma. Endocr. J. 54(5), 777–782 (2007)
A.K. Watts, A. Easwaran, P. McNeill, Y.Y. Wang, W.J. Inder, C. Caputo, Younger age is a risk factor for regrowth and recurrence of nonfunctioning pituitary macroadenomas: Results from a single Australian centre. Clin. Endocrinol. (Oxf.) 87(3), 264–271 (2017)
Z.Y. Xu, S. Ellis, C.C. Lee et al. Silent Corticotroph Adenomas After Stereotactic Radiosurgery: A Case-Control Study. Int. J. Radiat. Oncol. Biol. Phys. 90(4), 903–910 (2014)
K.Y. Zhang, X.F. Shou, H. Chen et al. Clinical Parameters of Silent Corticotroph Adenomas With Positive and Negative Adrenocorticotropic Hormone Immunostaining: A Large Retrospective Single-Center Study of 105 Cases. Front. Endocrinol. (Lausanne) 11, 608691 (2021)
O. Cooper, Silent corticotroph adenomas. Pituitary 18(2), 225–231 (2015)
A. Fountas, A. Lavrentaki, A. Subramanian, K.A. Toulis, K. Nirantharakumar, N. Karavitaki, Recurrence in silent corticotroph adenomas after primary treatment: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 104(4), 1039–1048 (2018)
N.F. Lenders, A.C. Wilkinson, S.J. Wong et al. Transcription factor immunohistochemistry in the diagnosis of pituitary tumours. Eur. J. Endocrinol. 184(6), 891–901 (2021)
Acknowledgements
We thank Trang Le and Thoa Le (University of Medicine and Pharmacy at Ho Chi Minh City) for their assistance with the abstract screening.
Author contributions
H.G.V.: conceptualization, data curation, formal analysis, investigation, methodology, project administration, software, validation, writing original, review, and editing. I.F.D.: conceptualization, project administration, validation, review, editing, and supervisions. All authors have read and approved the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vuong, H.G., Dunn, I.F. The clinicopathological features and prognosis of silent corticotroph tumors: an updated systematic review and meta-analysis. Endocrine 82, 527–535 (2023). https://doi.org/10.1007/s12020-023-03449-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03449-w