Abstract
Purpose
To investigate the association between circulating osteocalcin and incident cardiovascular diseases in a community-based cohort, and further assess whether the association differs by different glycemic stages.
Methods
This cohort study included 1428 participants (626 men and 802 women) aged 50–80 years, without baseline cardiovascular diseases, and with osteocalcin data available. Circulating total osteocalcin levels were measured by electrochemiluminescence immunoassay. Multivariate Cox proportional hazards models were used to assess the relationship between osteocalcin levels and different glycemic stages with cardiovascular events.
Results
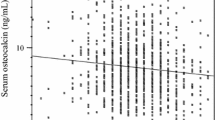
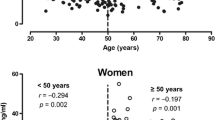
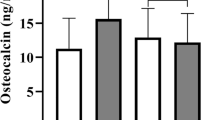
At baseline, 437 participants were normoglycaemia and 991 participants were hyperglycaemia. Median circulating osteocalcin levels were 16.43 (13.34–20.19) and 21.66 (17.95–26.11) ng/mL in men and women, respectively. During a mean follow-up of 7.6 years, 144 cases of cardiovascular diseases occurred (10.1%). The risk of incident cardiovascular diseases linearly increased with a decrease in baseline osteocalcin quartiles (quartile 1 versus quartile 4: hazard ratio 2.44, 95% confidence interval 1.07–5.55) in women, while not in men (Pinteraction on sex = 0.028). Subgroup analyses showed that the association was more predominant in participants with baseline hyperglycaemia. Besides, the joint effect of baseline decreased osteocalcin levels and hyperglycaemia resulted in higher risks of future cardiovascular diseases.
Conclusions
Low baseline osteocalcin levels were associated with high risks of cardiovascular diseases in middle-aged and elderly women, which were more predominant among those with baseline hyperglycaemia.




Similar content being viewed by others
Data availability
The dataset analyzed during the current study is available from the corresponding author upon reasonable request.
References
G. Hu, Gender difference in all-cause and cardiovascular mortality related to hyperglycaemia and newly-diagnosed diabetes. Diabetologia. 46(5), 608–617 (2003)
X. Cai, Y. Zhang, M. Li, J.H. Wu, L. Mai, J. Li, Y. Yang, Y. Hu, Y. Huang, Association between prediabetes and risk of all-cause mortality and cardiovascular disease: updated meta-analysis. BMJ. 370, m2297 (2020)
T. Wang, J. Lu, Q. Su, Y. Chen, Y. Bi, Y. Mu, L. Chen, R. Hu, X. Tang, X. Yu, M. Li, M. Xu, Y. Xu, Z. Zhao, L. Yan, G. Qin, Q. Wan, G. Chen, M. Dai, D. Zhang, Z. Gao, G. Wang, F. Shen, Z. Luo, Y. Qin, L. Chen, Y. Huo, Q. Li, Z. Ye, Y. Zhang, C. Liu, Y. Wang, S. Wu, T. Yang, H. Deng, D. Li, S. Lai, Z.T. Bloomgarden, L. Shi, G. Ning, J. Zhao, W. Wang, 4C Study Group: ideal cardiovascular health metrics and major cardiovascular events in patients with prediabetes and diabetes. JAMA. Cardiol. 4(9), 874–883 (2019)
G. Liu, Y. Li, Y. Hu, G. Zong, S. Li, E.B. Rimm, F.B. Hu, J.E. Manson, K.M. Rexrode, H.J. Shin, Q. Sun, Influence of lifestyle on incident cardiovascular disease and mortality in patients with diabetes mellitus. J. Am. Coll. Cardiol. 71(25), 2867–2876 (2018)
Y. Takashi, D. Kawanami, The role of bone-derived hormones in glucose metabolism, diabetic kidney disease, and cardiovascular disorders. Int. J. Mol. Sci. 23(4), 2367 (2022)
M. Zhou, X. Ma, H. Li, X. Pan, J. Tang, Y. Gao, X. Hou, H. Lu, Y. Bao, W. Jia, Serum osteocalcin concentrations in relation to glucose and lipid metabolism in Chinese individuals. Eur. J. Endocrinol. 161(5), 723–729 (2009)
J. Liu, Y. Wei, P. Zang, W. Wang, Z. Feng, Y. Yuan, H. Zhou, Z. Zhang, H. Lei, X. Yang, J. Liu, B. Lu, J. Shao, Circulating osteocalcin is associated with time in range and other metrics assessed by continuous glucose monitoring in type 2 diabetes. Diabetol. Metab. Syndr. 14(1), 109 (2022)
I. Kanazawa, T. Yamaguchi, M. Yamamoto, M. Yamauchi, S. Kurioka, S. Yano, T. Sugimoto, Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 94(1), 45–49 (2009)
J. Dou, H. Li, X. Ma, M. Zhang, Q. Fang, M. Nie, Y. Bao, W. Jia, Osteocalcin attenuates high fat diet-induced impairment of endothelium-dependent relaxation through Akt/eNOS-dependent pathway. Cardiovasc. Diabetol. 13, 74 (2014)
Y. Shen, L. Chen, J. Zhou, C. Wang, F. Gao, W. Zhu, G. Hu, X. Ma, H. Xia, Y. Bao, Low total osteocalcin levels are associated with all-cause and cardiovascular mortality among patients with type 2 diabetes: a real-world study. Cardiovasc. Diabetol. 21(1), 98 (2022)
X. Zhang, Y. Shen, Y. Xu, Q. Xiong, Z. Lu, X. Ma, Y. Bao, W. Jia, Association of serum osteocalcin levels with major adverse cardiovascular events: a 4.4-year retrospective cohort study. Clin. Exp. Pharmacol. Physiol. 45(1), 3–9 (2018)
B.B. Yeap, S.A. Chubb, L. Flicker, K.A. McCaul, P.R. Ebeling, G.J. Hankey, J.P. Beilby, P.E. Norman, Associations of total osteocalcin with all-cause and cardiovascular mortality in older men. The Health In Men Study. Osteoporos. Int. 23(2), 599–606 (2012)
T. Yamashita, K. Okano, Y. Tsuruta, T. Akiba, K. Nitta, Serum osteocalcin levels are useful as a predictor of cardiovascular events in maintenance hemodialysis patients. Int. Urol. Nephrol. 45(1), 207–214 (2013)
K. Holvik, N.M. van Schoor, E.M. Eekhoff, M. den Heijer, D.J. Deeg, P. Lips, R. de Jongh, Plasma osteocalcin levels as a predictor of cardiovascular disease in older men and women: a population-based cohort study. Eur. J. Endocrinol. 171(2), 161–170 (2014)
T. Hu, Y. Shen, W. Cao, Y. Xu, Y. Wang, Y. Bao, X. Ma, The association and joint effect of adipocyte fatty acid-binding protein and obesity phenotype with cardiovascular events. J. Clin. Endocrinol. Metab. dgad110 (2023). Epub ahead of print
G. Yang, L. Fan, J. Tan, G. Qi, Y. Zhang, J.M. Samet, C.E. Taylor, K. Becker, J. Xu, Smoking in China: findings of the 1996 National Prevalence Survey. JAMA. 282(13), 1247–1253 (1999)
V.D. Tran, V.V. Do, N.M. Pham, C.T. Nguyen, N.T. Xuong, J. Jancey, A.H. Lee, Validity of the International Physical Activity Questionnaire-Short Form for Application in Asian Countries: a study in Vietnam. Eval. Health. Prof. 43(2), 105–109 (2020)
T. Wang, J. Lu, L. Shi, G. Chen, M. Xu, Y. Xu, Q. Su, Y. Mu, L. Chen, R. Hu, X. Tang, X. Yu, M. Li, Z. Zhao, Y. Chen, L. Yan, G. Qin, Q. Wan, M. Dai, D. Zhang, Z. Gao, G. Wang, F. Shen, Z. Luo, Y. Qin, L. Chen, Y. Huo, Q. Li, Z. Ye, Y. Zhang, C. Liu, Y. Wang, S. Wu, T. Yang, H. Deng, J. Zhao, S. Lai, Y. Bi, R.A. DeFronzo, W. Wang, G. Ning; China Cardiometabolic Disease and Cancer Cohort Study Group, Association of insulin resistance and β-cell dysfunction with incident diabetes among adults in China: a nationwide, population-based, prospective cohort study. Lancet. Diabetes. Endocrinol. 8(2), 115–124 (2020)
D.R. Matthews, J.P. Hosker, A.S. Rudenski, B.A. Naylor, D.F. Treacher, R.C. Turner, Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 28(7), 412–419 (1985)
A.S. Levey, L.A. Stevens, C.H. Schmid, Y.L. Zhang, A.F. Castro III, H.I. Feldman, J.W. Kusek, P. Eggers, F. Van Lente, T. Greene, J. Coresh; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration), A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150(9), 604–612 (2009)
T. Hu, Y. Shen, W. Cao, Y. Xu, Y. Wang, X. Ma, Y. Bao, Neck circumference for predicting the occurrence of future cardiovascular events: a 7.6-year longitudinal study. Nutr. Metab. Cardiovasc. Dis. 32(12), 2830–2838 (2022)
N.A. ElSayed, G. Aleppo, V.R. Aroda, R.R. Bannuru, F.M. Brown, D. Bruemmer, B.S. Collins, M.E. Hilliard, D. Isaacs, E.L. Johnson, S. Kahan, K. Khunti, J. Leon, S.K. Lyons, M.L. Perry, P. Prahalad, R.E. Pratley, J.J. Seley, R.C. Stanton, R.A. Gabbay; on behalf of the American Diabetes Association, 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes. Care. 46(Suppl 1), S19–S40 (2023)
T. Unger, C. Borghi, F. Charchar, N.A. Khan, N.R. Poulter, D. Prabhakaran, A. Ramirez, M. Schlaich, G.S. Stergiou, M. Tomaszewski, R.D. Wainford, B. Williams, A.E. Schutte, 2020 International Society of Hypertension Global Hypertension Practice Guidelines. J. Hypertens. 75(6), 1334–1357 (2020)
Joint Committee for Guideline Revision, 2016 Chinese guidelines for the management of dyslipidemia in adults. J. Geriatr. Cardiol. 15(1), 1–29 (2018)
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World. Health. Organ. Tech. Rep. Ser. 894, i–253 (2000).
Y.C. Hwang, M. Kang, I.J. Cho, I.K. Jeong, K.J. Ahn, H.Y. Chung, M.K. Lee, Association between the circulating total osteocalcin level and the development of cardiovascular disease in middle-aged men: a mean 8.7-year longitudinal follow-up study. J. Atheroscler. Thromb. 22(2), 136–143 (2015)
B.B. Yeap, H. Alfonso, S.A. Chubb, E. Byrnes, J.P. Beilby, P.R. Ebeling, C.A. Allan, C. Schultz, G.J. Hankey, J. Golledge, L. Flicker, P.E. Norman, Proportion of undercarboxylated osteocalcin and serum P1NP predict incidence of myocardial infarction in older men. J. Clin. Endocrinol. Metab. 100(10), 3934–3942 (2015)
Q. Gong, P. Zhang, J. Wang, J. Ma, Y. An, Y. Chen, B. Zhang, X. Feng, H. Li, X. Chen, Y.J. Cheng, E.W. Gregg, Y. Hu, P.H. Bennett, G. Li; Da Qing Diabetes Prevention Study Group, Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet. Diabetes. Endocrinol. 7(6), 452–461 (2019)
M. Ferron, J. Wei, T. Yoshizawa, A. Del Fattore, R.A. DePinho, A. Teti, P. Ducy, G. Karsenty, Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell. 142(2), 296–308 (2010)
K. Fulzele, R.C. Riddle, D.J. DiGirolamo, X. Cao, C. Wan, D. Chen, M.C. Faugere, S. Aja, M.A. Hussain, J.C. Brüning, T.L. Clemens, Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell. 185(4), 746 (2022)
J. Wei, M. Ferron, C.J. Clarke, Y.A. Hannun, H. Jiang, W.S. Blaner, G. Karsenty, Bone-specific insulin resistance disrupts whole-body glucose homeostasis via decreased osteocalcin activation. J. Clin. Invest. 124(4), 1–13 (2014)
Funding
This work was partly funded by the Shanghai Research Center for Endocrine and Metabolic Diseases (2022ZZ01002), Shanghai Municipal Science and Technology Commission Medical Guide Project (19411964300), Shanghai Pujiang Program (21PJ1411800), and Shanghai Municipal Key Clinical Specialty. The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.Q.B. and X.J.M. conceived the study. T.T.H. and Y.S. analyzed the data and wrote the manuscript. Y.T.X. and Y.F.W. collected the data. Y.S. and Y.Q.B. obtained funding. All authors contributed to the conception and design of the work, interpretation of the data, reviewed and provided edits and comments on the manuscript, approved the final version of the manuscript, and agree to be accountable for all aspects of the work. Y.Q.B. and X.J.M. are the guarantors of this work and, as such, had full access to all the data in the study.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The current study was carried out in accordance with the principles of the Declaration of Helsinki and approved by the institutional review board at the Ethics Committee of Shanghai Sixth People’s Hospital Affiliated with Shanghai Jiao Tong University School of Medicine, approved number 2019-067.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, T., Shen, Y., Xu, Y. et al. Low total osteocalcin levels are associated with the risk of cardiovascular events among women with hyperglycaemia: a 7.6-year prospective study. Endocrine 82, 47–56 (2023). https://doi.org/10.1007/s12020-023-03428-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03428-1