Abstract
Background
Osteocalcin, a protein secreted mainly by mature osteoblasts, has been shown to be involved in glucose metabolism through various pathways. However, few studies has explored the association between osteocalcin and Time in range (TIR). Continuous glucose monitoring (CGM) -derived metrics, such as TIR and other indexes have been gradually and widely used in clinical practice to assess glucose fluctuations. The main purpose of this study was to investigate the correlation between osteocalcin and indexes from CGM in patients with type 2 diabetes mellitus (T2DM).
Method
The total number of 376 patients with T2D were enrolled, all of them performed three consecutive days of monitoring. They were divided into four groups on account of the quartile of osteocalcin. Time in range, Time below range (TBR), Time above range(TAR) and measures of glycemic variability (GV) were assessed for analysing. After a 100 g standard steamed bread meal, blood glucose (Glu0h Glu0.5 h, Glu1h, Glu2h, GLu3h), C-peptide (Cp0h, Cp0.5 h, Cp1h, Cp2h, Cp3h), serum insulin (INS0h, INS0.5 h, INS1h, INS2h, INS3h) concentrations at different time points were obtained. HOMA-IS, HOMA-βwas calculated to evaluate insulin sensitivity and insulin secreting of the participants.
Results
Patients with higher osteocalcin level had higher TIR (P < 0.05). Spearman correlation analysis showed that osteocalcin was positively correlated with TBR (although the P value for TBR was greater than 0.05) (r = 0.227, P < 0.001 r = 0.068, P = 0.189) and negatively correlated with TAR (− 0.229, P < 0.001). Similarly, there was a negative correlation between osteocalcin and glycemic variability (GV) indicators, including SD, MBG, MODD, ADDR, and MAGE (P value of MAGE > 0.05). Multiple stepwise regression showed that osteocalcin was an independent contributor to TIR, TAR and HOMA-IS.
Conclusion
Circulating osteocalcin is positively correlated with TIR and negatively correlated with MODD, ADDR, and MAGE. Osteocalcin may have a beneficial impact on glucose homeostasis in T2DM patients.
Similar content being viewed by others
Background
In the last few decades, the number of people with diabetes has increased from 151 to 463 million by 2020 [1], and diabetes has become the ninth leading cause of death worldwide [2]. Recent diabetes treatment guidelines emphasize individualized treatment in the management of diabetes patients. As a plausible and common biomarker, HBA1c is a gold standard for assessing long-term glycemic control over the past 2 to 3 months [3, 4]. A series of studies have demonstrated that HBA1c plays a prominent role in the management of diabetes [5, 6]. However, the accuracy of HbA1C measurements can be affected by various clinical conditions [7, 8]. Moreover, HbA1C does not reflect blood glucose fluctuations, and thus fail to prevent potential harmful hyperglycemic or hypoglycemic events [9, 10]. In contrast, continuous glucose monitoring (CGM) provides a more accurate picture of glycemic variability by measuring glucose concentrations in the interstitium continuously for several days. A standardized CGM report was recommended internationally in 2017 [7]. The parameters derived from CGM, including TIR, TBR, TAR, SD, MBG, MODD, and ADDR [11], are widely used to assess glycemic variability in clinical. Furthermore, TIR was recommended as one of the target indicators for glycemic control assessment by the ADA recently [12].
Osteocalcin, a bone γ-carboxyglutamate (GLA) protein encoded by the human osteocalcin gene BGLAP, is mainly produced by osteoblasts [13, 14]. Osteocalcin was originally considered to act only in skeletal cells when it was first discovered in the 1976s [15]. Lee identified a novel function of osteocalcin in Ocn-/- mice in 2007, indicating that osteocalcin may be involved in regulating energy metabolism [16]. Although numerous studies have explored the relationship between osteocalcin and glucose metabolism since then, the results remains are still controversial. A cohort study found that osteocalcin levels in the HbA1c ≥ 9% group were significantly lower than those in the HbA1c < 7% group [17]. In contrast, another study showed that osteocalcin levels decreased after daily calcium supplements for one year in older community-dwelling women, whereas HbA1c did not change [18]. On the other hand, few studies have explored the correlation between osteocalcin and glucose variability, the effects of osteocalcin on glucose fluctuations remain unclear. The purpose of this study is to investigate the correlation between steocalcin and TIR and other parameters of glycemic variability from CGM in T2DM patients.
Study design and methodology
Research Subjects
A total of 376 participants were recruited from the Department of Endocrinology in Jinling Hospital of Southern Medical University according to the diagnostic criteria published by the WHO in 1999 [19]. Inclusion criteria were age ≥ 18 years and having a stable glucose- lowering treatment within the last three months. Individuals who met one of the following criteria were excluded: hyperglycemic hyperosmolar state or severe hypoglycemic events within the past 3 months; diabetic ketoacidosis; history of cancer and psychiatric disease; severe hepatic or renal dysfunction; comorbid thyroid or parathyroid disease; diagnosis of osteoporosis; and treatment with medications that can affect bone and calcium metabolism, such as vitamin D, calcitonin, bisphosphonates, or estrogens. The local ethics committee approved the study in accordance with the Declaration of Helsinki.
Anthropometric and biochemical assessment
Basic characteristics including age composition, gender, duration of diabetes mellitus, height and weight were collected. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured with an accurate sphygmomanometer, and BMI was obtained according to an international formula. After an all-night fast, venous blood samples were drawn from participants by a professional the day before the CGM was performed. HbA1c was measured by high performance liquid chromatography (HLC-723G8 automated glycated hemoglobin analyzer, TOSOH, Japan). Biochemical indicators were measured by an automated biochemical analyzer (7600 series automated analyzer, Hitachi, Japan). Circulating osteocalcin levels, insulin and C-peptide concentrations were obtained by chemiluminescent immunoassay (IMMULITE 2000 XPi, Siemens, Germany). HOMA-IS and HOMA-β were calculated according to the standard formula {HOMA-β = 20 × fasting insulin (FINS mIU/L)/[fasting serum glucose (FPG mmol/L)- 3.5], HOMA-IS = 22.5/[FPG (mmol/L) × FINS (mIU/L)]}.
CGM parameters
Patients were tested by CGM (Meiqi) for three consecutive days (all participants were informed about the system and its safety by a regular professional before participating in the experiment). Raw blood glucose data were detected every three minutes and were not visible to the patients. Oxford's EasyGV version 9.0R2 was used to assess glycemic control metrics. Each individual was taught to avoid any strenuous activity that could affect blood glucose. TIR was defined as the percentage of time that blood glucose level remained between 3.9 and 10 mmol/L throughout the day, TBR represented the percentage of time that blood glucose was < 3.9 mmol/L in a 24-h period, and TAR was the proportion of time that exceeded 10.0 mmol/L during the day [7]. Glycemic control indicators such as standard deviation (SD), coefficient of variation of glucose (CV), low glycemic index (LBGI), high glycemic index (HBGI), mean amplitude of glucose excursion (MAGE), mean daily risk range (ADDR), and mean daily difference (MODD) were calculated and analyzed.
Statistical analysis
Patients were classified as G1 (osteocalcin < 10.68 ng/ml), G2 (10.68 ng/ml≦osteocalcin < 13.72 ng/ml), G3 (13.72 ng/ml≦osteocalcin < 17.30 ng/ml) and G4 (osteocalcin ≧17.30 ng/ml) according to the quartiles of osteocalcin levels. Data are expressed as mean ± SD, median [25% 75%]. Categorical variables were tested by chi-square test. Regarding continuous and normally distributed variables, one-way ANOVA was used to assess trends in each group, while Kruskal–Wallis H-test was used for abnormalities. We performed Spearman rank correlation to assess the association between osteocalcin and other variables. After adjusting for age, duration of diabetes, gender, BMI, SBP, DBP, TG, TC and other indicators, multivariate linear regression analysis was used to examine the independent association of osteocalcin with CGM parameters. We considered P < 0.05 as statistically significant. SPSS 25.0 software was used for analysis.
Results
Comparison of clinical characteristics between groups
In our study, 376 patients with T2DM (235 males and 141 females) were divided into four groups according to the quartiles of osteocalcin (Table 1). The osteocalcin concentrations in groups 1 to 4 were 8.73 (7.50 9.82) ng/ml, 12.38 (11.43 13.19) ng/ml, 15.10 (14.51 16.00) ng/ml, and 21.20 (18.70 26.27) ng/ml, respectively. The TIR of each group is shown in Fig. 1. There were no statistically significant differences between the groups in terms of gender composition, age, weight, BMI, duration of diabetes or blood pressure (P > 0.05, respectively). Similarly, there were no differences between groups in biochemical measurements, such as TC, TG, serum K + , serum Ca + , creatinine and total vitamin D (Table 1).
TIR of each group by quartile of osteocalcin levels (G1:osteocalcin < 10.68 ng/ml, G2:10.68 ng/ml≦osteocalcin < 13.72 ng/ml, G3:13.72 ng/ml≦osteocalcin < 17.30 ng/ml, G4:osteocalcin≧17.30 ng/ml). Kruskal–Wallis H test was applied to show statistical significance of comparison between groups (n = 94 per group) *p = 0.001
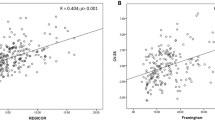
Correlation of serum osteocalcin and glucose indexes
Patients with G3 and G4 tended to have lower TAR and HbA1C levels, as well as MBG, SD, CV, HBGI, ADDR and MODD compared to G1 (P < 0.05). In contrast, the TIR and LBGI were lower in G1. Positive correlations were found between osteocalcin and TIR and HOMA-IS (r = 0.227, 0.192 P < 0.001), negative correlations were found between osteocalcin and TAR and HbA1C, while the relationship between osteocalcin and HOMA-βwas not significant (P = 0.801). Similarly, blood glucose at INS0h, INS0.5 h and all time points were inversely correlated with circulating osteocalcin (Table 2). As for the glycemic variability indices, HBGI, SD, CV, MBG, MODD, MAGE and ADDR all decreased with increasing serum osteocalcin levels.
Multiple stepwise regression analysis of the factors influencing TIR, TAR, HOMA-β, and HOMA-IS
Multiple stepwise regression analysis was used to study the influencing factors of TIR, TBR and TAR, and the results showed that age, disease duration, TG, ALT, eGFR, osteocalcin, GluOh, Cp3h, and HbA1C were independent influencing factors of TIR (Table 3). The influencing factors of TAR and TBR were shown in Tables 4 and 5, respectively. Osteocalcin was found to be one of the influencing factors for HOMA-IS (ß = 0.188, P < 0.001) (Table 6), but not in HOMA-β (Table 7).
Discussion
Osteocalcin, a secreted protein consisting of 49 amino acid residues, plays a crucial role in the regulation of bone metabolism. However, recent studies cast new light on osteocalcin and suggest that bone can act as an endocrine organ involved in energy metabolism by secreting osteocalcin [20, 21]. Studies found osteocalcin levels were significantly lower in diabetic patients than in non-diabetic patients [22]. Hu found serum osteocalcin was also negatively associated with fasting plasma glucose in 2032 healthy Chinese women [23]. Higher OC levels were linearly associated with a decreased risk of diabetes in the non-diabetes subcohort [24]. Further research found that osteocalcin was negatively correlated with glucose concentrations in patients with different levels of glycemic tolerance, including normal glucose tolerance, impaired glucose tolerance and T2DM [25]. In the Swedish MrOS study, serum osteocalcin was considered as an independent negative predictor of plasma glucose [26]. Similarly, we found serum osteocalcin level was negatively associated with fasting and postprandial glucose concentrations at all time points and MBG.
High blood glucose variability is detrimental to the control and treatment of diabetes, an increase in dawn glucose level and glycemic excursions were negatively correlated with bone turnover markers [27]. To assess the relationship between bone turnover markers such as osteocalcin and glucose variability, CGM was used in this study to monitor blood glucose fluctuations and provide detailed information of glycaemic status. As an emerging metric derived from CGM data, TIR is commonly used to analyze the quality of glycemic control [7, 28]. Studies have shown that TIR describes not only short-term but also long-term glucose variability [29, 30]. Since TIR is highly correlated with HbA1C, TIR may be used to determine the outcome of clinical studies, predict diabetic complications, and assess glycemic control in individual patients [31]. A study of 3,262 diabetic patients confirmed the association between TIR and the incidence of diabetic retinopathy at all stages [32]. Using the DCCT dataset, Beck proposed that the hazard rate of development of retinopathy progression was increased by 64%, and development of the micro- albuminuria outcome was increased by 40%, for each 10 percentage points lower TIR [33]. A growing number of international organizations and guidelines support the inclusion of TIR as one of the target indicators for glycemic control and recommended that most diabetic patients have a glycemic control targets of TIR > 70%, TBR < 4%, and TBR < 1% [28].
In the present study, we found a positive correlation between serum osteocalcin and LBGI, while the relationship between osteocalcin and TBR had no significant correlation. TIR was significantly higher in the group with higher osteocalcin, while TAR decreased with increasing osteocalcin concentrations. In addition, various indicators of glycemic stability, such as SD, MODD, and ADDR were inversely correlated with osteocalcin, suggesting that osteocalcin may be a protective factor for TIR. Previous studies have shown that osteocalcin is positively correlated with HOMA-β [34] and negatively correlated with HOMA -IR [35]. We found that higher osteocalcin was a protective factor for HOMA -IS, whereas the relationship between osteocalcin and HOMA -β was not significant. Increasing insulin sensitivity and improving insulin resistance are crucial to maintain glucose homeostasis in diabetic patients [36]. Osteocalcin is able to increase insulin secretion or insulin sensitivity by stimulating the release of adiponectin [37,38,39], which is helpful to reduce blood glucose fluctuations. Osteocalcin could increase β-cell proliferation, energy expenditure, and adiponectin expression [40]. In vivo, administration of recombinant osteocalcin using subcutaneous mini-pump improved glucose tolerance and insulin sensitivity in mice [41]. Oral administration of osteocalcin exhibited similar effects [42].
On the other hand, constant high glucose could result in intestinal epithelial cell inflammation and apoptosis, which may be worsened due to drastic glucose fluctuation [43]. Anti-inflammatory medications may improve diabetes patient outcomes by reducing inflammatory activities and enhancing anti-inflammatory responses [44]. Recombinant LZ-8 dose-dependently reduced blood glucose, and haemoglobin A1c (HbA1c) by inhibiting inflammation and enhancing Tregs generation in diabetic rat model [45]. Likewise, osteocalcin can significantly reduce the secretion of pro-inflammatory cytokines and relieve inflammatory effects induced by hyperglycemic, through the PI3K/Akt/NF -kB signaling pathway [46, 47]. Futhermore, osteocalcin can stabilize blood sugar by interacting with muscle, fat and other tissues, but the exact mechanism remains obscure [48]. Further studies are needed to validate these issues.
There are some limitations in our study. Firstly, the patients in this study underwent CGM for 3 days instead of the 10–14 days which was recommended internationally [7, 49]. Secondly, osteocalcin exists in two forms, carboxylated and undercarboxylated osteocalcin [50]. However, we only assessed total serum osteocalcin due to technical reasonsin. Thirdly, we did not perform cell- or animal- based experiments to explore the possible mechanisms. Last but not least, this was a retrospective observational study, with a relatively small sample size. A larger multicenter, prospective study is needed to validate our findings in the future.
In conclusion, circulating osteocalcin is positively correlated with TIR and negatively correlated with MODD, ADDR, and MAGE. Osteocalcin may have a beneficial impact on glucose homeostasis in T2DM patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- T2D:
-
Type 2 diabetes
- CGM:
-
Continuous glucose monitoring
- BMI:
-
Body mass index
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- HbA1c:
-
Hemoglobin A1c
- TIR:
-
Time in range
- TBR:
-
Time below range
- TAR:
-
Time above range
- CV:
-
Coefficient variation
- SD:
-
Standard deviation
- LBGI:
-
Low blood glucose index
- HBGI:
-
High blood glucose index
- MAGE:
-
Mean amplitude of glucose excursions
- ADDR:
-
Average daily danger range
- MODD:
-
Mean of daily differences
References
Saeedi P, Petersohn I, Salpea P, et al. IDF Diabetes Atlas Committee Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157: 107843.
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–71.
Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. Diabetes Control and Complications Trial Research Group. J Pediatr. 1994;125(2):177–88.
Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. 2014;383:69–82.
Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther. 2019;21:81–5.
Schade DS, Lorenzi GM, Braffett BH, et al. DCCT/EDIC Research Group. Hearing impairment and type 1 diabetes in the diabetes control and complications trial/ epidemiology of diabetes interventions and complications (DCCT/EDIC) cohort. Diabetes Care. 2018;41:2495–501.
Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care. 2017;40:1631–40.
Wolffenbuttel BH, Herman WH, Gross JL, et al. Ethnic differences in glycemic markers in patients with type 2 diabetes. Diabetes Care. 2013;36(10):2931–6.
Beyond A1C Writing Group. Need for regulatory change to incorporate beyond A1C glycemic metrics. Diabetes Care. 2018;41:92–4.
Runge AS, Kennedy L, Brown AS, et al. Does time-in-range matter? Perspectives from people with diabetes on the success of current therapies and the drivers of improved outcomes. Clin Diabetes. 2018;36:112-9.51.
Bergenstal RM, Beck RW, Close KL, et al. Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes Care. 2018;41:2275–80.
American Diabetes Association. 6 Glycemic Targets: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66–76.
Hauschka PV, Lian JB, Cole DE, et al. Osteocalcin and matrix Gla protein: vitamin K-dependent proteins in bone. Physiol Rev. 1989;69(3):990–1047.
Puchacz E, Lian JB, Stein GS, et al. Chromosomal localization of the human osteocalcin gene. Endocrinology. 1989;124(5):2648–50.
Price PA, Poser JW, Raman N. Primary structure of the gamma- carboxyglutamic acid-containing protein from bovine bone. Proc Natl Acad Sci USA. 1976;73:3374–5.
Lee NK, Sowa H, Hinoi E, et al. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007;130(3):456–69.
Zhao H, Qi C, Zheng C, et al. Effects of glycated hemoglobin level on bone metabolism biomarkers in patients with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2020;22(13):1785–91.
Lewis JR, Brennan-Speranza TC, Levinger I, et al. Effects of calcium supplementation on circulating osteocalcin and glycated haemoglobin in older women. Osteoporos Int. 2019;30(10):2065–72.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53.
DiGirolamo DJ, Clemens TL, Kousteni S. The skeleton as an endocrine organ. Nat Rev Rheumatol. 2012;8(11):674–83.
Karsenty G, Oury F. Biology without walls: the novel endocrinology of bone. Annu Rev Physiol. 2012;74:87–105.
Zhou M, Ma X, Li H, et al. Serum osteocalcin concentrations in relation to glucose and lipid metabolism in Chinese individuals. Eur J Endocrinol. 2009;161:723–9.
Hu WW, Ke YH, He JW, et al. Serum osteocalcin levels are inversely associated with plasma glucose and body mass index in healthy Chinese women. Acta Pharmacol Sin. 2014;35(12):1521–6. https://doi.org/10.1038/aps.2014.92 (Epub 2014 Oct 20).
Ye X, Yu R, Jia W, et al. Osteocalcin and risks of incident diabetes and diabetic kidney disease: a 4.6-year prospective cohort study. Diabetes Care. 2022;45(4):830–6.
Chen X, Wu Y, Liu L, et al. Osteocalcin is inversely associated with glucose levels in middle-aged Tibetan men with different degrees of glucose tolerance. Diabetes Metab Res Rev. 2014;30:476–82.
Kindblom JM, Ohlsson C, Smith U, et al. Plasma osteocalcin is inversely related to fat mass and plasma glucose in elderly Swedish men. J Bone Miner Res Off J Am Soc Bone Miner Res. 2009;24:785–91.
Starup-Linde J, Lykkeboe S, Handberg A, et al. Glucose variability and low bone turnover in people with type 2 diabetes. Bone. 2021;153:116159.
The Official Journal of ATTD Advanced Technologies & Treatments for Diabetes Conference Madrid, Spain-February 19–22, 2020. Diabetes Technol Ther. 2020;22(S1): A1-A250.
Vigersky RA, ShinJ JB, et al. The comprehensive glucose pentagon: a glucose-centric composite metric for assessing glycemic control in persons with diabetes. J Diabetes Sci Technol. 2018;12:114–23.
Augstein P, Heinke P, et al. Q-Score: development of a new metric for continuous glucose monitoring that enables stratification of antihyperglycaemic therapies. BMC Endocr Disord. 2015;1(15):22.
Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time- in-range in patients with diabetes. Diabetes Technol Ther. 2019;21:81–5.
Lu J, Ma X, Zhu W, et al. Association of time in range, as assessed by continuous glucose monitoring, with diabetic retinopathy in type 2 diabetes. Diabetes Care. 2018;41:2370–6.
Beck RW, Bergenstal RM, Riddlesworth TD, et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019;42:400–5.
Bao YQ, Zhou M, Zhou J, et al. Relationship between serum osteocalcin and glycaemic variability in Type 2 diabetes. Clin Exp Pharmacol Physiol. 2011;38(1):50–4.
Hwang YC, Jeong IK, Ahn KJ, et al. The uncarboxylated form of osteocalcin is associated with improved glucose tolerance and enhanced beta-cell function in middle-aged male subjects. Diabetes Metab Res Rev. 2009;25:768–72.
Arai C, Arai N, Mizote A, et al. Trehalose prevents adipocyte hypertrophy and mitigates insulin resistance. Nutr Res. 2010;30(12):840–8.
Ferron M, McKee MD, Karsenty G. Intermittent injections of osteocalcin improve glucose metabolism and prevent type 2 diabetes in mice. Bone. 2011;50:568–75.
Yamauchi T, Kamon J, Kadowaki T. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med. 2001;7(8):941–6.
Kubota N, Terauchi Y, Noda T. Disruption of adiponectin causes insulin resistance and neointimal formation. J Biol Chem. 2002;277(29):25863–6.
Hussein AG, Mohamed RH, Shalaby SM, et al. Vitamin K2 alleviates type 2 diabetes in rats by induction of osteocalcin gene expression. Nutrition. 2018;47:33–8.
Ferron M, McKee MD, Levine RL, et al. Intermittent injections of osteocalcin improve glucose metabolism and prevent type 2 diabetes in mice. Bone. 2011;50:568–75.
Mizokami A, Yasutake Y, Higashi S, et al. Oral administration of osteocalcin improves glucose utilization by stimulating glucagon-like peptide-1 secretion. Bone. 2014;69C:68–79.
Chen B, Jia Y, Lu D, et al. Acute glucose fluctuation promotes in vitro intestinal epithelial cell apoptosis and inflammation via the NOX4/ROS/JAK/STAT3 signaling pathway. Exp Ther Med. 2021;22(1):688. https://doi.org/10.3892/etm.2021.10120.
Nwadiugwu MC. Inflammatory activities in type 2 diabetes patients with co-morbid angiopathies and exploring beneficial interventions: a systematic review. Front Public Health. 2021;25(8):600427. https://doi.org/10.3389/fpubh.2020.600427.
Xiao H, Fang Z, He X, Ding P, et al. Recombinant ling zhi-8 enhances Tregs function to restore glycemic control in streptozocin-induced diabetic rats. J Pharm Pharmacol. 2020;72(12):1946–55.
Hill HS, Grams J, Walton RG, et al. Carboxylated and uncarboxylated forms of osteocalcin directly modulate the glucose transport system and inflammation in adipocytes. Horm Metab Res. 2014;46(5):341–7.
Zhou B, Li H, Xu L, et al. Osteocalcin reverses endoplasmic reticulum stress and improves impaired insulin sensitivity secondary to diet-induced obesity through nuclear factor-κB signaling pathway. Endocrinology. 2013;154(3):1055–68.
Ferron M, Hinoi E, Karsenty G, et al. Osteocalcin differentially regulates beta cell and adipocyte gene expression and affects the development of metabolic diseases in wild-type mice. Proc Natl Acad Sci USA. 2008;105:5266–70.
Riddlesworth TD, Bergenstal RM, Lee S, et al. Optimal sampling duration for continuous glucose monitoring to determine long-term glycemic control. Diabetes Technol Ther. 2018;20:314–6.
Hill HS, Grams J, Walton RG, et al. Carboxylated and uncarboxylated forms of osteocalcin directly modulate the glucose transport system and inflammation in adipocytes. Horm Metab Res. 2014;46:341–7.
Acknowledgements
The authors are very thankful to forward their gratitude to the data collectors, supervisors, and study subjects for their cooperation.
Funding
This work was supported by the National Natural Science Foundation of China(81873174); Key Research and Development Plan Project of Jiangsu Province—Social Development Projects(BE2020701).
Author information
Authors and Affiliations
Contributions
JL, YW, PZ, WW, and ZF conceived and designed the research. JL, PZ, YY, HZ and ZZ collected the data. JL, YW, HL, XY, and JL analyzed and interpreted the data. JL wrote the manuscript. BL and JS critically revised the manuscript and contributed to the discussion. JL, YW, and PZ contributed equally to this work. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the ethics committee of Southern Medical University. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, J., Wei, Y., Zang, P. et al. Circulating osteocalcin is associated with time in range and other metrics assessed by continuous glucose monitoring in type 2 diabetes. Diabetol Metab Syndr 14, 109 (2022). https://doi.org/10.1186/s13098-022-00863-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00863-4