Abstract
Purpose
To investigate the effects of laboratory-confirmed SARS-CoV-2 infection on thyroid function tests (TFTs) in pregnant women and to evaluate whether TFT changes are related to the severity and prognosis.
Methods
Consecutive pregnant women tested for SARS-CoV-2 by RT-PCR at Ankara City Hospital were recruited between January 2021 and September 2021. Thyroid-stimulating hormone (TSH), free thyroxine (FT4) and free triiodothyronine (FT3), thyroid peroxidase antibody (anti-TPO), and thyroglobulin antibody (anti-TG) were measured on admission.
Results
Among 747 eligible pregnant women with the same baseline characteristics, 369 RT-PCR-positive women in the patient group and 378 RT-PCR-negative women in the control group were included in the analyses. Pregnant women in the patient group had significantly lower TSH, FT4, FT3, Anti TPO, and Anti TG concentrations compared with those in the control group (p < 0.001). The proportion of patient groups with mild, moderate, severe, and critical diseases were 297 (80.4%), 40 (10.8%), 17 (4.6%), and 15 (4.2%), respectively, among which with the moderate, severe, and critical disease had significantly lower FT3 values (2.5 vs 2.19 pg/mL, p < 0.001) and higher nonthyroidal illness syndrome (NTIS) (29.2 vs. 8.4%, p < 0.001) than those with mild disease. Lower FT3 values increased the risk of ICU admission, NICU admission, and severe disease (p < 0.001). FT3 and TSH correlated positively with lymphocytes (p < 0.001) and negatively correlated with C-reactive protein (CRP) (p < 0.001, p = 0.005).
Conclusion
The SARS-CoV-2 infection seems to have an impact on the TFTs of pregnant women, and particularly FT3 level seems to be correlated with disease severity.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19), was declared a global pandemic by the World Health Organization (WHO) in March 2020 [1]. By July 18, 2022, more than 565 million confirmed cases and more than 6 million deaths have been reported worldwide [2].
COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which uses angiotensin-converting enzyme 2 (ACE2) as a host cell receptor to infect humans [3, 4]. ACE2 is not only an enzyme as it is known but also a receptor on tissue cells through which SARS-CoV-2 enters the host cells. According to recent studies, it is highly expressed in many organs such as the lung, heart, kidney, liver, and endocrine organs (e.g., thyroid and pituitary), making the hypothalamic-pituitary-thyroid (HPT) axis a susceptible target of SARS-CoV-2 for both direct (due to ACE2 expression) and indirect damage (due to abnormal immune-inflammatory responses to the virus) [5,6,7,8,9]. Based on this pathophysiology of the virus, previous studies have shown that COVID-19 could induce reversible thyroid dysfunction and could be associated with the severity of the disease [10, 11].
Pregnancy has a considerable impact on the thyroid gland and its function. Depending on the need for maternal thyroid hormone production, the importance of thyroid hormones increases significantly during pregnancy. Two sources supply thyroid hormones to fetal tissues: the developing fetal thyroid gland and the maternal thyroid gland. Although the fetal thyroid gland begins to develop by the 5th or 6th week of gestation and begins to produce thyroid hormones by about the 12th week of gestation, it is not functionally mature until the 18th to 20th week of gestation, and nearly 30% of the free thyroxine (FT4) in the umbilical cord blood serum at delivery is of maternal origin. This means that maternal FT4 is transferred to the fetus throughout pregnancy and is critical for normal fetal brain development, especially in the first half of pregnancy [12,13,14,15]. In addition, thyroid disorders in pregnancy have been associated with serious maternal, fetal, and neonatal complications in numerous previous studies: spontaneous abortions, preterm delivery, preeclampsia, gestational diabetes mellitus, admission to the neonatal intensive care unit (NICU), placental abruption, and breech presentation [16,17,18,19]. Thus, timely detection and treatment of pregnant women with thyroid dysfunction are clinically important because even mild thyroid dysfunction can lead to adverse pregnancy outcomes. Almost all data in the literature on pregnant women are limited by the absence of FT3 measurement as the fetus majorly relies on transplacental delivery of maternal T4.
There are many studies investigating the association between thyroid functions and COVID -19, but similar studies on pregnant women are limited and restricted to comparing the pandemic period with the pre-pandemic period [20, 21]. To our knowledge, there has been no study comparing SARS-CoV-2 positive pregnant women with negative pregnant women during the pandemic period with respect to the analysis of thyroid function.
Therefore, the objectives of the present study were to investigate the effects of laboratory-confirmed SARS-CoV-2 infection on thyroid function tests (TFT) in pregnant women and to determine whether it leads to thyroid dysfunction. We also evaluated whether HPT axis and autoantibody changes are related to the severity and prognosis of COVID-19 in pregnancy and whether there is a correlation between TFT and inflammatory disease markers in patient pregnant women.
Materials and methods
This single-center case-control study was performed at Ankara City Hospital, a tertiary pandemic referral hospital with approximately 20,000 deliveries per year, accounting for the vast majority of SARS-CoV-2 infected pregnant women antenatal examinations and deliveries in Ankara, Turkey. Ethics approval was obtained from the institutional review board (No. E2-21-269). All participants provided written informed consent. The study was conducted in accordance with the Declaration of Helsinki [22].
Pregnant women from all trimesters were enrolled, who underwent thyroid function analysis at our hospital between January 01, 2021, and September 30, 2021, and were simultaneously tested for SARS-COV2 by reverse transcriptase-polymerase chain reaction (RT-PCR) and divided into 2 groups. RT-PCR-positive pregnant women considered as the study group was compared to an RT-PCR-negative gestational age-matched control group of pregnant women at the same period. According to the national guideline for COVID-19 management, the study group was divided into subgroups; mild, moderate, severe, and critical [23]. In all pregnant women, SARS-Cov-2 infection was confirmed by quantitative RT-PCR from nasal-oropharyngeal swab and blood samples were drawn from participants from antecubital vein between 07:00 a.m. and 09:00 a.m. along with RT-PCR test upon their first admission to the hospital or first overnight fasting after RT-PCR testing before initiation of any treatment and medication.
The following information, including sociodemographic and clinical data, was recorded by the researchers in the electronic medical record: Maternal age, gravidity, parity, previous miscarriage, living child, pre-pregnancy body mass index (BMI), the gestational week at the time of testing, gestational trimester at the time of diagnosis, the severity of COVID-19, maternal mortality, ICU admission rate, neonatal ICU admission rate, thyroid function tests (TFT); thyrotropin (TSH), free thyroxine (FT4), free triiodothyronine (FT3), antithyroid peroxidase antibody (anti-TPO), and anti-thyroglobulin antibody (anti-TG) concentrations.
Pregnant women were excluded from the analysis if they were obese (BMI before pregnancy >40 kg/m2), underwent in vitro fertilization (IVF), had multiple pregnancies, had a history of thyroid disease or thyroid autoantibody positivity, were taking thyroid medication, or were using steroids and heparin for any reason. We did not include the cases if there were any missing values of TSH, FT3, FT4, and thyroid autoantibodies. We also wanted to exclude vaccinated pregnant women, based on a systematic review that analyzed data from 51 patients who developed thyroid problems after the COVID-19 vaccination [24]. Indeed, one study reported low acceptance of COVID -19 vaccination among pregnant women in Turkey [25], none of the participants were vaccinated in the present study. in the present study, none of the participants were vaccinated. A total of 747 pregnant women-study groups (n = 369), and control group (n = 378)-were included in the final analysis (Fig. 1).
The lower limits of detection of thyroid function tests in our laboratory were 28 and 0.1 IU/ml for Anti TPO and Anti TG, respectively; 0.01 mU/L for TSH; 1.36 ng/L for FT3; 0.63 ng/dl for FT4. Anti TPO≥60 IU/ml was considered positive. Anti TG ≥1.3 IU/ml was considered positive. The trimester-specific reference intervals in our hospital were set according to the 2017 guidelines of the American Thyroid Association and the Turkey Endocrinology and Metabolism Society [26, 27]. For the first trimester, the reference intervals were 0.1–2.5 mU/L for TSH and 0.8–1.53 ng/dL for FT4, and 2.46–3.89 ng/L for FT3. For the second trimester, they were 0.2–3 mU/L for TSH and 0.7–1.2 ng/dl for FT4, and 2.09–3.55 ng/L for FT3, and in the third trimester, they were 0.3–3 mU/L for TSH and 0.7–1.2 ng/dl for FT4 and 2.01–3.27 ng/L for FT3. TSH, FT4, FT3, anti-TPO, and anti-TG were measured by electrochemiluminescence immunoassay (ECLIA) on a Roche Cobas 6000 e 601 analyzer (Roche Diagnostics).
The study group was divided into four categories of thyroid dysfunction (subclinical hypothyroidism, subclinical hyperthyroidism, isolated hypothyroxinemia, and nonthyroidal illness syndrome). We defined subclinical hypothyroidism as high TSH with normal FT4 and FT3; subclinical hyperthyroidism as low TSH with normal FT4 and FT3; isolated hypothyroxinemia as low FT4 with normal TSH and FT3; nonthyroidal illness syndrome (NTIS) as low FT3 with normal TSH and FT4. Finally, correlation analysis was performed in the study group to evaluate basic inflammatory biomarkers such as C-reactive protein (CRP), interleukin-6 (IL -6), and lymphocyte levels with TFT analysis. IL Interleukin-6 levels were measured using commercially available ELISA kits according to the kit data sheet (eBioscience, Thermo Fisher Scientific USA).
Statistical analyzes were performed using the SPSS package program (IBM SPSS Statistics 24). Frequency tables and descriptive statistics were used to interpret the results. Parametric methods were used for the measured values suitable for normal distribution. In accordance with the parametric methods, the “independent sample t”-test (t-table value) was used to compare the measured values of two independent groups. Nonparametric methods were used for the measured values that did not conform to the normal distribution. “Mann–Whitney U”-test (Z-table value) to compare the measured values of two independent groups by nonparametric methods; “Kruskal–Wallis H” method (χ2-table value) to compare the measured values of three or more independent groups. “Spearman” correlation coefficient was used to study the relationships between two quantitative variables that do not have a normal distribution. “Pearson-χ2” cross-tabulations were used to analyze the relationships between two qualitative variables. Binary logistic regression: the backward model LR was used to determine the factors affecting the risk situations.
Results
Baseline characteristics and TFT analysis between groups
There was no statistically significant difference between groups (p > 0.05) in baseline characteristics. Pregnant women in the study group had significantly lower TSH, FT4, FT3, Anti TPO, and Anti TG concentrations than those in the control group (p < 0.001) (Table 1).
TFT analysis between groups according to gestational-specific reference intervals
Then, we classified the TFT level as low/normal/high and thyroid autoantibodies as positive/negative according to trimester-specific references (Table 2). We found that the patient group was significantly more likely to have low TSH and low FT3 levels, while the control group had a predominance of high levels (p = 0.034 and p < 0.001). We also found that Anti TPO positivity was significantly higher in the control group (p < 0.001), while Anti TG positivity was significantly higher in the patient group (p < 0.001).
TFT analysis between groups according to Covid-19 severity
The study population was divided into two groups based on the severity of COVID-19: a mild group and a moderate/severe/critical group. Table 3 compares the thyroid function tests of each group. Patients with moderate/severe/critical disease had significantly lower FT3 values than patients with mild disease (p < 0.001), while there was no significant difference in FT4, TSH values, and thyroid autoantibody positivity (p > 0.05). To investigate the risk of developing a non-mild disease, logistic regression was performed with the parameters that were significant in the univariate analysis. FT3 level was found to be an important parameter inversely affecting disease severity (p < 0.001) (OR = 0.913; 1- OR = 0.087) (95% CI: 0.857–0.944).
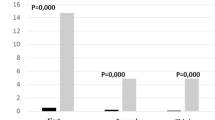
FT3 levels according to COVID-19 severity (including the control group) were (2.87 ± 0.42 ng/dl) for control; (2.50 ± 0.46 ng/dl) for mild; (2.24 ± 0.37 ng/dl) for moderate; (2.17 ± 0.35 ng/dl) for severe; (2.11 ± 0.35 ng/dl) for critical patients and those levels show that the degree of FT3 reduction was related to confirmed disease and disease severity.
Thyroid disease and the severity of COVID-19
In Table 4, we analyzed the severity of COVID-19 and thyroid disease. While no statistically significant association was found between disease severity and subclinical hypothyroidism, subclinical hyperthyroidism, and isolated hypothyroxinemia (p > 0.05), the NTIS rate was significantly higher (29.2–8.4%) in the moderate/severe/critical group (p < 0.001).
Comparison of TFT analysis with COVID-19 according to ICU and NICU admissions and risk analysis
The study population was divided into two groups based on maternal ICU admission. As shown in Table 5, FT3 levels of ICU-admitted patients were significantly lower than those of non-ICU-admitted patients (p < 0.001), while there was no statistically significant difference between groups for TSH, FT4, anti-TPO, and anti-TG (p > 0.05). Logistic regression analysis was performed with the parameters that were significant in the univariate analysis to investigate the association between FT3 and ICU admission. It was found that FT3 level was a significant parameter inversely affecting ICU admission (p < 0.001, OR = 0.912; 1- OR = 0.088) (95% CI: 0.811–0.969).
Subsequently, the study population was divided into two groups based on fetal NICU admission. As shown in Table 6, not only were the FT3 scores of the NICU-admitted infants significantly lower than those of the non-NICU-admitted infants (p < 0.001), but the FT4 scores were also significantly lower in the NICU-admitted group (p = 0.013). Logistic regression analysis with the parameters that were significant in univariate analysis was used to investigate the relationship between FT3, FT4, and NICU admission. It was found that the FT3 value was an important parameter that inversely affected NICU admission (p < 0.001, OR = 0.909; 1- OR = 0.091) (95% CI: 0.824–0.961).
Correlation analysis of laboratory biomarkers and TFTs
Finally, we examined the correlation of lymphocyte count, IL -6, CRP level, and TFT analysis in pregnant women with COVID -19, as shown in Table 7. We observed a significant positive correlation between lymphocytes with FT3 and TSH levels (p < 0.001) and a significant negative relationship between CRP with FT3 and TSH levels (p < 0.001, p = 0.005).
Discussion
Data on the relationship between COVID-19 and pregnancy have been published since March 2020 [28,29,30]. However, to the best of our knowledge, the current study is the first on the analysis of thyroid function during the COVID-19 outbreak, comparing confirmed SARS-CoV-2 positive pregnant women with confirmed negative pregnant women and establishing an association with disease severity in pregnancy.
As mentioned earlier, most data in the literature on pregnant women are limited by the absence of FT3 measurement and thyroid autoantibody status, so further studies with these measurements were needed to determine the full effects of COVID -19 on the HPT axis. Therefore, one of the greatest strengths of our study was the inclusion of all TFTs. Here, we report the effect of COVID -19 on the HPT axis in pregnancy.
In the first part of the present study, we performed an analysis of positive and negative pregnant cases. The comprehensive analysis of our study showed that pregnant women infected with COVID -19 had significantly lower levels of FT3, FT4, TSH, anti-TPO, and anti-TG compared to the confirmed negative pregnant cases with the same baseline characteristics. Although all TFTs were suppressed in the study group, there was no difference in low FT4, while low FT3 and low TSH were significantly higher in the patient group. Wang et al. reported that TT3 and TSH levels were lower in COVID -19 patients than in the healthy group [31], which is consistent with our results, while no significant difference was found in TT4, in contrast to our results, which showed significantly lower FT4 levels. The contrast in FT4 may be due to the difference between the control groups in both studies because healthy individuals who underwent a routine annual physical examination before the onset of COVID -19 served as controls in their study. Indeed, Lin et. al. found that exposure to the COVID -19 outbreak was independently associated with lower FT4 levels in pregnant women [20]. Based on this study, it can be interpreted that anxiety triggered by COVID -19 during pregnancy [32] significantly affects maternal thyroid function. Of note, the overall decrease in all TSH, FT4, and FT3 levels in SARS-CoV-2 infected pregnant women are indicative of an indirect nonthyroidal clinical picture rather than a direct thyroid effect.
Anti TPO and Anti TG positivity are known to be present in 15.2 and 8.9% of unselected pregnant women, respectively [33], and a recent meta-analysis found isolated positivity of 4.1 and 4.8%, respectively [34]. Data suggest that thyroid autoantibody positivity is associated with poor fetal outcomes [35], and, in particular, with an increased risk of preterm birth [36, 37]. Previous studies in nonpregnant women have shown an increase in antithyroid antibody levels 3 months after COVID-19 [22] and following COVID-19 vaccination [38]. However, data on the impact of SARS-CoV-2 infection on thyroid autoantibodies during acute disease are still limited. In our analysis of unvaccinated pregnant women, we found that anti-TPO positivity was significantly higher in the control group (24.9–6.2%) and, paradoxically, anti-TG positivity was significantly higher in the patient group (17.1–6.6%), although both had significantly lower concentrations in the patient group. However, we found that none of the autoantibodies were related to disease severity, ICU, and NICU admission, both in terms of concentration and positivity.
In the second part of our study, we performed a subgroup analysis in the positive pregnant cases according to disease severity, thyroid dysfunction, ICU admission, and NICU admission. We found that TSH and FT4 levels were suppressed with disease severity, but this was not statistically significant. On the other hand, moderately severe, severe, and critical cases were found to have significantly lower FT3 levels and a higher rate of NTIS than mild cases, which is confirmed by the literature in recent studies on the nonpregnant population [39,40,41]. Consequently, thyroid function testing in pregnant patients seems reasonable, although WHO does not recommend systematic thyroid function testing in hospitalized COVID -19 patients [42].
In addition, FT4 and FT3 levels of positive pregnant women with NICU admission were significantly lower than those without NICU admission, but in logistic regression analysis, we found an increased risk for NICU admission only with decreased FT3 levels. Although maternal FT4 level is very important for the intrauterine life of fetuses, it does not increase the risk for NICU admission in newborns, even if it was significantly suppressed in the mother.
According to recent guidelines from ATA [26], subclinical hyperthyroidism during pregnancy is not associated with adverse outcomes and only needs to be monitored, whereas subclinical hypothyroidism is associated with adverse obstetric and fetal outcomes, and treatment with thyroxine is recommended in selected cases. Data regarding the association between isolated hypothyroxinemia and adverse maternal and fetal outcomes are controversial. Some studies suggest that isolated maternal hypothyroxinemia (IMH) is associated with an increased risk of preterm birth and hence admission to the neonatal intensive care unit [43, 44], whereas others have found no association [45, 46].
Because the severity of COVID-19 is known to increase the risk of perinatal complications, we found no association between disease severity and subclinical hyperthyroidism and IMH in the present study. On the other hand, COVID-19 severity was significantly associated with NTIS and insignificantly associated with subclinical hypothyroidism in our study, as described in previous studies [47, 48]. In view of analyzes using the logistic regression model to evaluate the predictive potential of low FT3 for the risk of non-mild COVID-19, ICU admission, and NICU admission, it has ensured that non-mild cases of COVID-19 may lead to NTIS in pregnant women as well.
Finally, we investigated the correlation between TFTs and some laboratory immune parameters at admission, which are commonly used in COVID-19 diagnosis and follow-up, because the thyroid gland is a neuroendocrine organ effective in immune regulation. We found that FT3 and TSH had a significant inverse correlation with CRP and a direct correlation with lymphocytes, whereas there was no correlation with IL-6. However, most data have shown that IL -6 is also inversely related to FT3 levels, in contrast to our results [49]. In the absence of a study on pregnant women, similar studies in nonpregnant patients are consistent with our results in CRP and lymphocytes [50,51,52]. Of note, FT4 levels showed no correlation with these parameters, which may be due to the fact that FT3 is the active form of FT4. Consequently, all these results support the potential interactions between the HPT axis and the immune system in COVID-19.
The main strengths of the present study were a large number of cases despite the monocentric design, the inclusion of all TFTs in all groups, and the fact that all pregnant women were not vaccinated and were not taking any medication that could affect TFT levels. Another strength is the presence of a control group and a group of patients with different clinical scenarios classified as mild, moderate, severe, and critical. On the other hand, we have some limitations. We matched the study groups based on a molecular test (RT-PCR), which is highly specific and the probability of false positive results is low, but false negative results are possible [53]. In addition, thyroid imaging was not performed in the patient group to assess the potential effects of COVID -19 on the thyroid beyond TFTs and antithyroid antibodies, particularly with regard to subacute thyroiditis (also called de Quervain’s thyroiditis or viral thyroiditis), which is an inflammatory disease of the thyroid gland that usually follows or coexists with a viral infection, especially in women, and in a recent review of case reports and case series linking subacute thyroiditis to a viral complication of COVID-19 [54].
In conclusion, SARS-CoV-2 infection appears to affect thyroid function analysis in pregnant women, and TFT levels, particularly FT3 levels, appear to be correlated with disease severity. It is well established in the literature that NTIS may be an early marker of poor outcomes of COVID-19, and the current study shows that a suppressed FT3 level has prognostic significance not only for disease severity and ICU admission but also for neonatal ICU admission. Considering the results of the present study as inferential, our study justifies the inclusion of FT3 in routine investigations alongside TSH and FT4 in pregnancies complicated with COVID-19. Given the ongoing COVID-19 pandemic, further studies in pregnancy are certainly needed to determine the full impacts of COVID -19 on the HPT axis, whereas similar data in pregnancy are still limited.
References
Organization W.H. WHO Director-General’s opening remarks at the media briefing on COVID-19 March 2020, https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
World Health Organization WHO Coronavirus (COVID-19) dashboard July 2022, https://covid19.who.int
M. Hoffmann, H. Kleine-Weber, S. Schroeder, N. Krüger, T. Herrler, S. Erichsen et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(2), 271–80.e8 (2020). https://doi.org/10.1016/j.cell.2020.02.052
C.G.K. Ziegler, S.J. Allon, S.K. Nyquist, I.M. Mbano, V.N. Miao, C.N. Tzouanas et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell 181(5), 1016–1035.e19 (2020). https://doi.org/10.1016/j.cell.2020.04.035
M.Y. Li, L. Li, Y. Zhang, X.S. Wang, Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect. Dis. Poverty 9(1), 45 (2020). https://doi.org/10.1186/s40249-020-00662-x
L. Scappaticcio, F. Pitoia, K. Esposito, A. Piccardo, P. Trimboli, Impact of COVID-19 on the thyroid gland: an update. Rev. Endocr. Metab. Disord. 22(4), 803–815 (2021). https://doi.org/10.1007/s11154-020-09615-z
W. Ni, X. Yang, D. Yang, J. Bao, R. Li, Y. Xiao, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 24, 422 (2020). https://doi.org/10.1186/s13054-020-03120-0
A. Java, A.J. Apicelli, M.K. Liszewski, A. Coler-Reilly, J.P. Atkinson, A.H. Kim et al. The complement system in COVID-19: friend and foe? JCI Insight. 5(15), e140711 (2020) . https://doi.org/10.1172/jci.insight.140711
S. Goncu Ayhan, D. Oluklu, S. Sinaci, A. Atalay, S.A. Erol, E. Ozden Tokalioglu et al. Fetal thymus size in pregnant women with COVID-19 infection. Gynecol. Obstet. Reprod. Med. 27(2), 84–88 (2021). https://doi.org/10.21613/GORM.2021.1222
G. Lisco, A. De Tullio, E. Jirillo, V.A. Giagulli, G. De Pergola, E. Guastamacchia et al. Thyroid and COVID-19: a review on pathophysiological, clinical and organizational aspects. J. Endocrinol. Invest 44(9), 1801–1814 (2021). https://doi.org/10.1007/s40618-021-01554-z
J. Zheng, Z. Cui, N. Shi, S. Tian, T. Chen, X. Zhong et al. Suppression of the hypothalamic-pituitary-thyroid axis is associated with the severity of prognosis in hospitalized patients with COVID-19. BMC Endocr. Disord. 21, 228 (2021). https://doi.org/10.1186/s12902-021-00896-2
J. Bernal, Thyroid hormone receptors in brain development and function. Nat. Clin. Pr. Endocrinol. Metab. 3(3), 249–259 (2007). https://doi.org/10.1038/ncpendmet0424
R.M. Calvo, E. Jauniaux, B. Gulbis, M. Asunción, C. Gervy, B. Contempré et al. Fetal tissues are exposed to biologically relevant free thyroxine concentrations during early phases of development. J. Clin. Endocrinol. Metab. 87(4), 1768–1777 (2002). https://doi.org/10.1210/jcem.87.4.8434
T.I. Korevaar, R. Muetzel, M. Medici, L. Chaker, V.W. Jaddoe, Y.B. de Rijke et al. Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: a population-based prospective cohort study. Lancet Diabetes Endocrinol. 4(1), 35–43 (2016). https://doi.org/10.1016/s2213-8587(15)00327-7
Thyroid disease in pregnancy: ACOG practice bulletin, number 223. Obstet Gynecol. 135(6), e261–e274 (2020). https://doi.org/10.1097/aog.0000000000003893
T. Männistö, P. Mendola, J. Grewal, Y. Xie, Z. Chen, S.K. Laughon, Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort. J. Clin. Endocrinol. Metab. 98(7), 2725–2733 (2013). https://doi.org/10.1210/jc.2012-4233
W.C. Allan, J.E. Haddow, G.E. Palomaki, J.R. Williams, M.L. Mitchell, R.J. Hermos et al. Maternal thyroid deficiency and pregnancy complications: implications for population screening. J. Med Screen 7(3), 127–130 (2000). https://doi.org/10.1136/jms.7.3.127
M. Abalovich, S. Gutierrez, G. Alcaraz, G. Maccallini, A. Garcia, O. Levalle, Overt and subclinical hypothyroidism complicating pregnancy. Thyroid 12(1), 63–68 (2002). https://doi.org/10.1089/105072502753451986
S. Singh, V.G. Nair, V.V. Singh, S. Tiwari, D. Arora, M. Dey et al. Pregnancy-specific concerns and psychological impact of COVID-19 on antenatal women. Gynecol. Obstet. Reprod. Med 28(2), 129–134 (2022). https://doi.org/10.21613/GORM.2021.1172
T.T. Lin, C. Zhang, H.Q. Zhang, Y. Wang, L. Chen, C.L. Dennis et al. Thyroid hormone changes in early pregnancy along with the COVID-19 pandemic. Front. Endocrinol. 11, 606723 (2020). https://doi.org/10.3389/fendo.2020.606723
J. Hua, J. Shen, J. Zhang, Y. Zhou, W. Du, G.J. Williams, The association between COVID-19 pandemic and maternal isolated hypothyroxinemia in first and second trimesters. Psychoneuroendocrinology 128, 105210 (2021). https://doi.org/10.1016/j.psyneuen.2021.105210
World Medical Association, World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 310(20), 2191–2194 (2013). https://doi.org/10.1001/jama.2013.281053
Turkish Ministry of Health. General Directorate of Public Health, COVİD‐19 (SARS‐CoV‐2 infection) Guideline, Scientific Committee Report, https://covid19.saglik.gov.tr/. Accessed May, 2020
S. Ippolito, D. Gallo, A. Rossini, B. Patera, N. Lanzo, G.F.M. Fazzino et al. SARS-CoV-2 vaccine-associated subacute thyroiditis: insights from a systematic review. J. Endocrinol. Invest 45, 1189–1200 (2022). https://doi.org/10.1007/s40618-022-01747-0
S. Goncu Ayhan, D. Oluklu, A. Atalay, D. Menekse Beser, A. Tanacan, O. Moraloglu Tekin et al. COVID-19 vaccine acceptance in pregnant women. Int J. Gynaecol. Obstet. 154(2), 291–296 (2021). https://doi.org/10.1002/ijgo.13713
E.K. Alexander, E.N. Pearce, G.A. Brent, R.S. Brown, H. Chen, C. Dosiou et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27(3), 315–389 (2017). https://doi.org/10.1089/thy.2016.0457
Türkiye Endokrinoloji ve Metabolizma Derneği (TEMD) Tiroid Hastalıkları Tanı ve Tedavi Kılavuzu 2020 [Available from: https://file.temd.org.tr/Uploads/publications/guides/documents/20200929134733-2020tbl_kilavuzf527c34496.pdf?a=1.
P. Dubey, S.Y. Reddy, S. Manuel, A.K. Dwivedi, Maternal and neonatal characteristics and outcomes among COVID-19 infected women: an updated systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 252, 490–501 (2020). https://doi.org/10.1016/j.ejogrb.2020.07.034
M.J. Delahoy, M. Whitaker, A. O’Halloran, S.J. Chai, P.D. Kirley, N. Alden et al. Characteristics and maternal and birth outcomes of hospitalized pregnant women with laboratory-confirmed COVID-19 - COVID-NET, 13 States, March 1-August 22, 2020. MMWR Morb. Mortal. Wkly Rep. 69(38), 1347–1354 (2020). https://doi.org/10.15585/mmwr.mm6938e1
D. Sahin, A. Tanacan, A.T. Anuk, S. Sinaci, B. Besimoglu, D. Oluklu, et al. Comparison of clinical features and perinatal outcomes between pre-variant and post-variant periods in pregnant women with SARS-CoV-2: analysis of 1935 cases. Arch Gynecol Obstet. 306(6), 1939–1948 (2022). https://doi.org/10.1007/s00404-022-06493-5
W. Wang, X. Su, Y. Ding, W. Fan, W. Zhou, J. Su et al. Thyroid function abnormalities in COVID-19 patients. Front Endocrinol. 11, 623792 (2020). https://doi.org/10.3389/fendo.2020.623792
S. Sinaci, E. Ozden Tokalioglu, D. Ocal, A. Atalay, G. Yilmaz, H.L. Keskin et al. Does having a high-risk pregnancy influence anxiety level during the COVID-19 pandemic. Eur. J. Obstet. Gynecol. Reprod. Biol. 255, 190–196 (2020). https://doi.org/10.1016/j.ejogrb.2020.10.055
A. McELDUFF, J. Morris, Thyroid function tests and thyroid autoantibodies in an unselected population of women undergoing first trimester screening for aneuploidy. Aust. N.Z. J. Obstet. Gynaecol. 48(5), 478–480 (2008)
S. Bliddal, A. Derakhshan, Y. Xiao, L.M. Chen, T. Männistö, G. Ashoor et al. Association of thyroid peroxidase antibodies and thyroglobulin antibodies with thyroid function in pregnancy: an individual participant data meta-analysis. Thyroid 32(7), 828–840 (2022). https://doi.org/10.1089/thy.2022.0083
S. Athar, S.F. Beer, Z. Martis, M.I. Alloub, The prevalence of thyroid autoimmunity in pregnancy and adverse neonatal outcomes at a secondary care hospital in the Middle East. Cureus 14(5), e24814 (2022). https://doi.org/10.7759/cureus.24814
S. Thangaratinam, A. Tan, E. Knox, M.D. Kilby, J. Franklyn, A. Coomarasamy, Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence. Bmj 342, d2616 (2011). https://doi.org/10.1136/bmj.d2616
R. Negro, Thyroid autoimmunity and pre-term delivery: brief review and meta-analysis. J. Endocrinol. Invest 34(2), 155–158 (2011). https://doi.org/10.1007/bf03347047
D.T.W. Lui, C.H. Lee, C.Y.Y. Cheung, J.H. Cheung Mak, C.H.Y. Fong, B.W.C. Lui, et al. Impact of COVID-19 vaccines on thyroid function and autoimmunity and impact of thyroid autoimmunity on antibody response. J. Clin. Endocrinol. Metab. 107(9), e3781–e3789 (2022). https://doi.org/10.1210/clinem/dgac355
R. Zou, C. Wu, S. Zhang, G. Wang, Q. Zhang, B. Yu et al. Euthyroid sick syndrome in patients with COVID-19. Front. Endocrinol. 11, 566439 (2020). https://doi.org/10.3389/fendo.2020.566439
D.T.W. Lui, C.H. Lee, W.S. Chow, A.C.H. Lee, A.R. Tam, C.H.Y. Fong et al. Thyroid dysfunction in relation to immune profile, disease status, and outcome in 191 patients with COVID-19. J. Clin. Endocrinol. Metab. 106(2), e926–e935 (2021). https://doi.org/10.1210/clinem/dgaa813
F.E.L. Beltrão, D.C.A. Beltrão, G. Carvalhal, F.E.L. Beltrão, A.D.S. Brito, K. Capistrano et al. Thyroid hormone levels during hospital admission inform disease severity and mortality in COVID-19 patients. Thyroid 31(11), 1639–1649 (2021). https://doi.org/10.1089/thy.2021.0225
World Health O. COVID-19 clinical management: living guidance, 25 January 2021. Geneva: World Health Organization; 2021 2021. Contract No.: WHO/2019-nCoV/clinical/2021.1.
X. Yang, Y. Yu, C. Zhang, Y. Zhang, Z. Chen, L. Dubois et al. The association between isolated maternal hypothyroxinemia in early pregnancy and preterm birth. Thyroid 30(12), 1724–1731 (2020). https://doi.org/10.1089/thy.2019.0818
T.I. Korevaar, S. Schalekamp-Timmermans, Y.B. de Rijke, W.E. Visser, W. Visser, S.M. de Muinck Keizer-Schrama et al. Hypothyroxinemia and TPO-antibody positivity are risk factors for premature delivery: the generation R study. J. Clin. Endocrinol. Metab. 98(11), 4382–4390 (2013). https://doi.org/10.1210/jc.2013-2855
G. León, M. Murcia, M. Rebagliato, M. Álvarez-Pedrerol, A.M. Castilla, M. Basterrechea et al. Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. the Infancia y Medio Ambiente Cohort, Spain. Paediatr. Perinat. Epidemiol. 29(2), 113–122 (2015). https://doi.org/10.1111/ppe.12172
M.P. Hamm, N.M. Cherry, J.W. Martin, F. Bamforth, I. Burstyn, The impact of isolated maternal hypothyroxinemia on perinatal morbidity. J. Obstet. Gynaecol. Can. 31(11), 1015–1021 (2009). https://doi.org/10.1016/s1701-2163(16)34345-6
M. Świstek, M. Broncel, P. Gorzelak-Pabiś, P. Morawski, M. Fabiś, E. Woźniak, Euthyroid sick syndrome as a prognostic indicator of COVID-19 pulmonary involvement, associated with poorer disease prognosis and increased mortality. Endocr. Pract. 28(5), 494–501 (2022). https://doi.org/10.1016/j.eprac.2022.02.006
M. Chen, W. Zhou, W. Xu, Thyroid function analysis in 50 patients with COVID-19: a retrospective study. Thyroid 31(1), 8–11 (2021). https://doi.org/10.1089/thy.2020.0363
C. Sparano, E. Zago, A. Morettini, C. Nozzoli, D. Yannas, V. Adornato et al. Euthyroid sick syndrome as an early surrogate marker of poor outcome in mild SARS-CoV-2 disease. J. Endocrinol. Invest 45, 837–847 (2022). https://doi.org/10.1007/s40618-021-01714-1
D.T.W. Lui, C.H. Lee, W.S. Chow, A.C.H. Lee, A.R. Tam, P. Pang et al. The independent association of TSH and Free triiodothyronine levels with lymphocyte counts among COVID-19 patients. Front Endocrinol. 12, 774346 (2021). https://doi.org/10.3389/fendo.2021.774346
V. Ilera, L.C. Delfino, A. Zunino, P. Glikman, M. Drnovsek, A. Reyes et al. Correlation between inflammatory parameters and pituitary-thyroid axis in patients with COVID-19. Endocrine 74, 455–460 (2021). https://doi.org/10.1007/s12020-021-02863-2
J. Deng, S. Zhang, F. Peng, Q. Zhang, Y. Li, Y. Zhong, The association between FT3 with the outcome and inflammation/coagulopathy/fibrinolysis of COVID-19. Front Endocrinol. 13, 877010 (2022). https://doi.org/10.3389/fendo.2022.877010
T. Ai, Z. Yang, H. Hou, C. Zhan, C. Chen, W. Lv et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 296(2), E32–e40 (2020). https://doi.org/10.1148/radiol.2020200642
M. Aemaz Ur Rehman, H. Farooq, M.M. Ali, M. Ebaad Ur Rehman, Q.A. Dar, A. Hussain, The association of subacute thyroiditis with COVID-19: a systematic review. SN Compr. Clin. Med. 3, 1515–1527 (2021). https://doi.org/10.1007/s42399-021-00912-5
Acknowledgements
Special thanks to all the healthcare professionals in our country who work devotedly during the pandemic period. We are also grateful to the authors of the studies cited in this article.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by A.A., B.B., S.S., E.K., and O.Ö. A.S.O.-E. and F.D.O. designed the study and critically revised the manuscript. The first draft of the manuscript was written by A.A. and D.S. commented on previous versions of the manuscript and study supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Approval was granted by the Ethics Committee of Ankara City Hospital (Approval, March 24, 2021 /Protocol No. E2-21-269).
Consent to participate
All participants signed informed written consent before being enrolled in the study. This study was performed in line with the principles of the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Atalay, A., Besimoglu, B., Sinaci, S. et al. The impact of covid-19 on thyroid function tests in pregnancy. Endocrine 79, 502–511 (2023). https://doi.org/10.1007/s12020-022-03248-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03248-9