Abstract
Purpose
Since the dramatic rise of obesity prevalence in childhood and adolescence has contributed to increased rates of type 2 diabetes (T2D) in youth, we sought to explore current evidence-based management options for pediatric T2D patients.
Methods
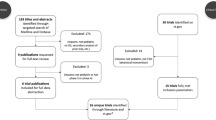
A comprehensive literature search was performed for studies of T2D in childhood and adolescence until September 2021.
Results
Special pathophysiological and diagnostic characteristics of T2D in this age are presented, while the main focus of the article is on management. Lifestyle interventions with healthy diet and exercise are of great importance for the treatment of T2D in children and adolescents. Metformin and insulin remain the traditional therapeutical means, while liraglutide recently gained indication for children older than 10 years both in USA and Europe. Data on the use, efficacy, safety and therapeutic considerations of other pharmacological treatments in children and adolescents with T2D are critically discussed.
Conclusion
Although many new and promising therapeutic strategies have been introduced during recent years for the management of T2D in adults, available therapeutic options for the management of pediatric T2D remain limited.

Similar content being viewed by others
References
S. Fazeli Farsani, A.A.M.P. Van der et al. Global trends in the incidence and prevalence of type 2 diabetes in children and adolescents: a systematic review and evaluation of methodological approaches. Diabetologia 56, 1471–88 (2013)
C.L. Ogden, M.D. Carroll, H.G. Lawman, C.D. Fryar, D. Kruszon-Moran, B.K. Kit et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 315, 2292–9 (2016)
S.H. Kwak, K.S. Park, Genetics of type 2 diabetes and potential clinical implications. Arch. Pharm. Res. 36, 167–177 (2013)
S.A. Arslanian, Metabolic differences between Caucasian and African-American children and the relationship to type 2 diabetes mellitus. J. Pediatr. Endocrinol. Metab. 15(Suppl 1), 509–517 (2002)
S. Arslanian, F. Bacha, M. Grey, M.D. Marcus, N.H. White, P. Zeitler, Evaluation and management of youth-onset type 2 diabetes: A position statement by the American Diabetes Association. Diabetes Care 41, 2648–2668 (2018)
Effects of Metformin, Metformin plus Roziglitazone and Metformin plus lifestyle on insulin sensitivity and b-cell function in TODAY. Diabetes Care 36, 1749–57 (2013)
P. Zeitler, S. Arslanian, J. Fu, O. Pinhas-Hamiel, T. Reinehr, N. Tandon, T. Urakami, J. Wong, D.M. Maahs, ISPAD Clinical Practice Consensus Guidelines 2018: Type 2 diabetes mellitus in youth. Pediatr. Diabetes 19(Suppl 27), 28–46 (2018). https://doi.org/10.1111/pedi.12719
E.S. Onge, S.A. Miller, C. Motycha, A. DeBerry, A review of the treatment of type 2 diabetes in children. J. Pediatr. Pharm. Ther. 20(1), 4–16 (2015)
R. Unnikrishnan, V.N. Shah, M. Viswanathan, Challenges in diagnosis and management of diabetes in the young. Clin. Diabetes Endocrinol. 2, 18–27 (2016)
M. Safavi, A. Foumadi, M. Abdollahi, The imprortance of synthetic drugs for type 2 diabetes drug discovery. Exp. Opin. Drug Discov. 8, 1339–83 (2013)
A.D. Liese, R.B. D’Agostino Jr, R.F. Hamman, P.D. Kilgo, J.M. Lawrence, L.L. Liu, B. Loots, B. Linder, S. Marcovina, B. Rodriguez, D. Standiford, D.E. Williams, The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics 118, 1510–1518 (2006)
T. Reinehr, Clinical presentation of type 2 diabetes mellitus in children and adolescents. Int J. Obes. (Lond.) 29(Suppl2), S105–S110 (2005)
S.N. Assuncao, N.C. Boa Sorte, C.A. Alves, P.S. Mendes, C.R. Alvves, L.R. Silva, Glucose alteration and insulin resistance in asymptomatic obese children and adolescents. J. Pediatr. (Rio J.) 94, 268–272 (2018)
K.J. Nudeau, B.J. Anderson, E.G. Berg, J.L. Chiang, H. Chou, K.C. Copeland, T.S. Hannon, T.T. Haung, J.L. Lynch, J. Powell, E. Sellers, W.V. Tamborlane, P. Zeitler, Youth onsent type 2 diabetes consensus report: current status, challenges and priorities. Diabetes Care 39, 1635–1642 (2016)
M.T. Barbato, P.R. Criado, A.K. Silva, E. Averbeck, M.B. Guerine, N.B. Sa, Association of acanthosis nigricans and skin tags with insulin resistance. Bras. Dermatol. 87, 97–104 (2012)
R.A. Schwartz, Akanthosis nigricans. J. Am. Acad. Dermatol. 31, 1–19 (1994)
E. Diamanti-Kandarakis, A. Dunaif, Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr. Rev. 33(6 Dec), 981–1030 (2012). https://doi.org/10.1210/er.2011-1034. Epub 2012 Oct 12
A. Dunaif, M. Graf, J. Mandeli, V. Laumas, A. Dobrjansky, Characterization of groups of hyperandrogenic women with acanthosis nigricans, impaired glucose tolerance, and/or hyperinsulinemia. J. Clin. Endocrinol. Metab. 65, 499–507 (1987)
K. Dileepan, M.M. Feldt, Type 2 diabetes mellitus in children and adolescents. Pediatrics Rev. 34, 541–548 (2013)
E. Schober, R.W. Holl, M. Grabert, A. Thon, B. Rami, T. Kapellen, O. Seewi, T. Reinehr, Diabetes mellitus type 2 in childhood and adolescence in Germany and parts of Austria. Eur. J. Pediatr. 164, 705–707 (2005)
T. Reinehr, W. Kiess, T. Kapellen, S. Wiegand, R.W. Holl, Children with diabetes mellitus type 2 in Europe: an underserved population. Arch. Dis. Child 95, 954 (2010)
S. Amed, H.J. Dean, C. Panagiotopoulos, E.A. Sellers, S. Hadjiyannakis, T.A. Laubscher et al. Type 2 diabetes, medication-induced diabetes and monogenic diabetes in Canadian children: a prospective national surveillance study. Diabetes Care 33(4), 786–791 (2010)
S. Spurr, J. Bally, C. Bullin, D. Allan, E. McNair, The prevalence of undiagnosed prediabetes/type 2 diabetes, prehypertension/hypertension and obesity among ethnic groups of adolescents in Western Canada. BMC Pedaitr. 20, 31–39 (2020)
E. Zeggini, A new era for Type 2 diabetes genetics. Diabet. Med. 24, 1181–86 (2007)
R.A. Defronzo, Banting Lecture. From the triumvirate to the ominous octet: a newparadigm for the treatment of type 2 diabetes mellitus. Diabetes 58(4), 773–795 (2009)
N. Gungor, F. Bacha, R. Saad, J. Janosky, S. Arslanian, Youth type 2 diabetes: insulin resistance, beta cell failure, or both? Diabetes Care 28, 638–644 (2005)
J. Un Ju, C. Myung-Sook, Obesity and Its Metabolic Complications: The Role of Adipokines and the Relationship between Obesity, Inflammation, Insulin Resistance, Dyslipidemia and Nonalcoholic Fatty Liver Disease. Int J. Mol. Sci. 15(4), 6184–6223 (2014)
J.C. Mbanya, A.A. Motala, E. Sobngwi, F.K. Assah, S.T. Enoru, Diabetes in sub-Saharan Africa. Lancet 375, 2254–66 (2010)
C.S. Yajnik, The lifecycle effects of nutrition and body size on adult adiposity, diabetes and cardiovascular disease. J. Clin. Endocrinol. Metab. 2002. https://doi.org/10.1046/j.1467-789X.2002.00072.x
F. Bacha, N. Gungor, S. Lee, S.A. Arslanian, Progressive deterioration of β-cell function in obese youth with type 2 diabetes. Pediatr. Diabetes 14(2), 106–111 (2013)
C. Dutil, J.P. Chaput, Inadequate sleep as a contributor to type 2 diabetes in children and adolescents. Nutr. Diabetes 8(7), e266 (2017). https://doi.org/10.1038/nutd.2017.19
B. Valaiyapathi, B. Gower, A.P. Ashraf, Pathophysiology of Type 2 Diabetes in Children and Adolescents. Curr. Diabetes Rev. 16(3), 220–229 (2020)
W.-K. Chan, P. Sthaneshwar, N.R. Nik Mustapha, S. Mahadeva, Limited utility of plasma M30 in discriminating non-alcoholic steatohepatitis from steatosis comparison with routine biochemical markers. PLoS ONE 9, e105903 (2014)
R.A. Defronzo, Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58, 773–795 (2009)
M. Franzago, F. Fraticelli, L. Stuppia, E. Vitacolonna, Nutrigenetics, epigenetics and gestational diabetes: consequences in mother and child. Epigenetics 14(3), 215–235 (2019). https://doi.org/10.1080/15592294.2019.1582277. Epub 2019 Mar 22
K. Hidayat, S.Y. Zou, B.M. Shi, The influence of maternal body mass index, maternal diabetes mellitus, and maternal smoking during pregnancy on the risk of childhood-onset type 1 diabetes mellitus in the offspring: systematic review and meta-analysis of observational studies. Obes. Rev. 20(8), 1106–1120 (2019). https://doi.org/10.1111/obr.12858. Epub 2019 May 15
T. Holder, C. Giannini, N. Santoro et al. A low disposition index in adolescent offspring of mothers with gestational diabetes: a risk marker for the development of impaired glucose tolerance in youth. Diabetologia 57(11), 2413–20 (2014)
C. Wang, H. Yatsuya, K. Tamakoshi, H. Toyoshima, K. Wada, Y. Li, E.H. Hilawe, M. Uemura, C. Chiang, Y. Zhang, R. Otsuka, A. Ota, Y. Hirakawa, A. Aoyama, Association between parental history of diabetes and the incidence of type 2 diabetes mellitus differs according to the sex of the parent and offspring’s body weight: a finding from a Japanese worksite-based cohort study. Prev. Med. 81, 49–53 (2015). https://doi.org/10.1016/j.ypmed.2015.07.021
B.L. Rodriguez, W.Y. Fujimoto, E.J. Mayer-Davis, G. Imperatore, D.E. Williams, R.A. Bell, R.P. Wadwa, S.L. Palla, L.L. Liu, A. Kershnar, S.R. Daniels, B. Linder, Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for diabetes in youth study. Diabetes Care 29, 1891–1896 (2006). https://doi.org/10.2337/dc06-0310
T. Reinehr, Type 2 diabetets mellitus in children and adolescents. World J. Diabetes 4(6), 270–281 (2013)
T.A. Hillier, K.L. Pedula, Complications in young adults with early-onset type 2 diabetes: losing the relative protection of youth. Diabetes Care 26(11), 2999–3005 (2003)
American Diabetes Associations, Classification and Diagnosis of Diabetes. Diabetes Care 38(Suppl. 1), S8–S16 (2015)
ISPAD, Clinical Practice Consensus Guidelines 2006–2007 Type 2 diabetes mellitus in the child and adolescent. Pediatr. Diabetes 9, 65–77 (2008)
A.L. Rosenbloom, J.H. Silverstein, S. Amemiya, P. Zeitler, G.J. Klingensmith, ISPAD Clinical Practice Consensus Guidelines 2006-2007. Type 2 diabetes mellitus in the child and adolescent. Pediatr. Diabetes 9, 512–526 (2008)
E.J. Mayer-Davis, A.R. Kahkoska, C. Jefferies, D. Dabelea, Balde N,5 Gong CX et al., ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr. Diabetes 19(Suppl 27), 7–19 (2018)
K.R. Owen, Monogenic diabetes in adults: what are the new developments? Curr. Opin. Genet. Dev. 50, 103–110 (2018). https://doi.org/10.1016/j.gde.2018.04.006
E. Kawasaki, T. Maruyama, A. Imagawa, H. Ikegami, Y. Uchigata, H. Osawa, Y. Kawabata, T. Kobayashi, A. Shimada, I. Shimizu, K. Takahashi, M. Nagata, H. Makino, T. Hanafusa, Diagnostic criteria for acute-onset type 1 diabetes mellitus (2012): Report of the Committee of Japan Diabetes Society on the research of fulminant and acute onset type 1 diabetes mellitus. J. Diabetes Investig. 5(1), 115–118 (2014)
A. Petersmann, D. Muller-Wieland, U.A. Muller, R. Landgraf, M. Nauck, G. Freckmann, L. Heinemann, E. Schleicher, Definition, classification and diagnosis of diabetes mellitus. Exp. Clin. Endocrinol. Diabetes 127(Suppl 1), S1–S7 (2019)
T.S. Hannon, The changing face of diabetes in youth: lessons learned from studies of type 2 diabetes.Arslanian SA. Ann. N. Y Acad. Sci. 1353, 113–37 (2015). https://doi.org/10.1111/nyas.12939. Epub 2015 Oct 8
A. Fagot-Campagna, K.M. Narayan, R.L. Hanson, G. Imperatore, B.V. Howard, R.G. Nelson, D.J. Pettitt, W.C. Knowler, Plasma lipoproteins and incidence of non-insulin-dependent diabetes mellitus in Pima Indians: protective effect of HDL cholesterol in women. Atherosclerosis 128, 113–119 (1997). https://doi.org/10.1016/S0021-9150(96)05978-3
SEARCH Study Group, SEARCH for diabetes in youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin. Trials 25, 458–471 (2004)
K.C. Copeland, P. Zeitler, M. Geffner, C. Guandalini, J. Higgins, K. Hirst, F.R. Kaufman, B. Linder et al, for the TODAY Study Group. J. Clin. Endocr. Metab. 96(1),159–167 (2011).
O. Pinhas-Hamiel, P. Zeitler, Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet 369, 1823–31 (2007)
E.W. Gregg, I. Hora, S.R. Benoit, Resurgence in diabetes-related complications. JAMA 321, 1867–1868 (2019)
T. Urakami, R. Kuwabara, M. Habu, A. Yoshida, M. Okuno, J. Suzuki, S. Takahashi, H. Mugishima, Pharmacologic treatment strategies in children with type 2 diabetes. Clin. Ped Endocrinol. 22(1), 1–8 (2013)
S. Weihrauch-Blüher, K. Kromeyer-Hauschild, K. Graf, K. Widhalm, U. Korsten-Reckf, B. Jödickeg et al. Current Guidelines for Obesity Prevention in Childhood and Adolescence. Obes. Facts 11, 263–276 (2018)
M.L. Gow, S.P. Garnett, L.A. Baur, N.B. Lister, The effectiveness of different diet strategies to reduce type 2 diabetes risk in youth. Nutrients 8(8), 486 (2016)
M.S. Tremblay, A.G. LeBlanc, V. Carson, L. Choquette, S.C. Gorber, C. Dillman et al. Canadian Physical Activity Guidelines for the Early Years (aged 0–4 years). Appl. Physiol. Nutr. Metab. 37, 345–356 (2012). https://doi.org/10.1139/H2012-018
J.N. Davis, A. Tung, S.S. Chak et al. Aerobic and strength training reduces adiposity in overweightLatina adolescents. Med Sci. Sports Exerc. 41(7), 1494–1503 (2009)
R.I. Berkowitz, M.D. Marcus, B.J. Anderson, L. Delahanty, N. Grover, A. Kriska et al. Adherence to a lifestyle program for youth with type 2 diabetes and its association with treatment outcome in the TODAY clinical trial. Pediatr. Diabetes 19(2), 191–198 (2018)
J.Y. Kim, J.Y. Jeon, Role of exercise on insulin sensitivity and beta-cell function: is exercise sufficient for the prevention of youth-onset type 2 diabetes? Ann. Pediatr. Endocrinol. Metab. 25, 208–216 (2020)
R.W. Beck, R.M. Bergenstal, T.D. Riddlesworth et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care 42, 400–405 (2019)
T. Battelino, T.H. Danne, R.M. Bergenstal, S.A. Amiel, R. Beck, T. Biester et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care 42, 1593–1603 (2019)
FDA News release, 2019: https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-pediatric-patients-type-2-diabetes
J.S.A. Pratt, A. Browne, N.T. Browne, M. Matias Bruzoni, M. Cohen, A. Desai et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg. Obes. Relat. Dis. 14, 882–901 (2018)
D.M. Styne, S.A. Arslanian, E.L. Connor et al. Pediatric obesity assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 102, 709–757 (2017)
K.C. Copeland, J. Silverstein, K.P. Moore et al. Management of newly diagnosed type 2 DM in children and adolescents. Pediatrics 131, 364–82 (2013)
J. Ludvigsson, Prevention of adverse events in juvenile diabetes. Minerva Pediatr. 56(3), 277–290 (2004)
F. Bacha, P. Cheng, R.L. Gal, C. Kollman, W.V. Tamborlane, G.J. Klingensmith et al. Initial Presentation of Type 2 Diabetes in Adolescents Predicts Durability of Successful Treatment with Metformin Monotherapy: Insights from the Pediatric Diabetes Consortium T2D Registry. Horm. Res. Paediatr. 89(1), 47–55 (2018). https://doi.org/10.1159/000481687. for the Pediatric Diabetes ConsortiumEpub 2017 Oct 31
W.V. Tamborlane, G. Klinensmith, Crisis in care: limited treatment options for type 2 diabetes in adolescents and youth. Diabetes Care 36, 1777–8 (2013)
S. Narasimhan, R.S. Weinstock, Youth-onset type 2 diabetes mellitus: lessons learned from the TODAY study. Mayo Clin. Proc. 89(6 Jun), 806–16 (2014). https://doi.org/10.1016/j.mayocp.2014.01.009
O. Tabatabaei-Malazy, S. Nikfar, B. Larijani, M. Abdollahi. Drugs for the treatment of pediatric type 2 diabetes mellitus and related comorbidities. Exp. Op. Pharmacother. 2016; https://doi.org/10.1080/14656566.2016.1258057
M. Sanyura, L.H. Philipson, R. Naylor, Monogenic diabetes in children and adolescents: recognition and treatment options. Curr. Diab. Rep. 18(8), 58 (2019). https://doi.org/10.1007/s11892-018-1024-2
M. Gottschalk, T. Danne, A. Vlajnic, J.F. Cara, Glimepiride versus metformin as monotherapy in pediatric patients with type 2 diabetes: a randomized, single-blind comparative study. Diabetes Care 30(4 Apr), 790–4 (2007)
J.D. Smith, E. Mills, S.E. Carlisle. Treatment of pediatric type 2 diabetes. Ann. Pharmacother. 2016;1–10, https://doi.org/10.1177/1060028016655179
M. Boris, C.C. Kaiser, A. Goldblatt, M,W. Elice, S.M. Edelson, J.B. Adams et al. Effect of pyoglitazone treatment on behavioral symptoms in autistic children. J. Neuroinflamm. 2007; https://doi.org/10.1186/1742-2094-4-3
TODAY Study Group, A clinical trial to maintain glycaemic control in youth with type 2 diabetes. N. Engl. J. Med. 366(24), 2247–2256 (2012)
H.J. Teede, M.L. Misso, M.F. Costello, A. Dokras, J. Laven, L. Moran, T. Piltonen, R.J. Norman, Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil. Steril. 110(3), 364–379 (2018)
H. Tfayli, J.W. Ulnach, S. Lee, K. Sutton-Tyrrell, S. Arslanian, Drospirenone/Ethinyl Estradiol Versus Rosiglitazone Treatment in Overweight Adolescents with Polycystic Ovary Syndrome: Comparison of Metabolic, Hormonal, and Cardiovascular Risk Factors. J. Clin. Endocrinol. Metab. 96(5), 1311–1319 (2011)
J. Rodenburg, M.N. Vissers, A. Wiegman, A.S. van Trotsenburg, A. van der Graaf, E. de Groot et al. Statin treatment in children with familial hypercholesterolemia: the younger, the better. Circulation 116(6), 664–8 (2007)
M.V. Tamborlane, M. Barrientos-Perez, U. Fainberg, H. Frimer-Larsen, M. Hafez, P.M. Hale et al. Liraglutide in children and adolescents with type 2 diabetes. N. Engl. J. Med. 381, 637–46 (2019)
D.J. Klein, T. Battelino, D.J. Chatterjee, L.V. Jacobsen, P.M. Hale, S. Arslanian, Liraglutide’s Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics in Pediatric Type 2 Diabetes: A Randomized, Double-Blind, Placebo-Controlled Trial. Diabetes Technol. Ther. 16(10 Oct), 679–687 (2014). https://doi.org/10.1089/dia.2013.0366
I.S. Kochar, A. Sethi, Efficacy and safety of Liraglutide in Indian adolescents with obesity. Obes. Sci. Pract. 5(3), 251–257 (2019). https://doi.org/10.1002/osp4.328
T. Danne, T. Biester, K. Kapitzke, S.H. Jacobsen, L.V. Jacobsen, K.C.C. Petri et al. Liraglutide in an Adolescent Population with Obesity: A Randomized, Double-Blind, Placebo-Controlled 5-Week Trial to Assess Safety, Tolerability, and Pharmacokinetics of Liraglutide in Adolescents Aged 12-17 Years. J. Pediatr. 181, 146–153.e3 (2017). https://doi.org/10.1016/j.jpeds.2016.10.076. Epub 2016 Dec 13
L.D. Mastrandrea, L. Witten, K.C. Carlsson Petri, P.M. Hale, H.K. Hedman, R.A. Riesenberg, Liraglutide effects in a paediatric (7‐11 y) population with obesity: A randomized, double‐blind, placebo‐controlled, short‐term trial to assess safety, tolerability, pharmacokinetics, and pharmacodynamics. Pediatr. Obes. 14(5 May), e12495 (2019). https://doi.org/10.1111/ijpo.12495. Published online 2019 Jan 17
S.E. Kanoski, M.R. Hayes, K.P. Skibicka, GLP-1 and weight loss: unraveling the diverse neural circuitry. Am. J. Physiol. Regul. Integr. Comp. Physiol. 310(10), R885–95 (2016). https://doi.org/10.1152/ajpregu.00520.2015
I.P. Fraser, N.D. Neufeld, L.A. Fox, M.S. Kipnes, T.L. Miller, P.S. Zeitler et al. A randomized clinical trial to evaluate the single-dose pharmacokinetics, pharmacodynamics, and safety of sitagliptin in pediatric patients with type 2 diabetes. Pediatr. Diabetes 20(1), 48–56 (2019). https://doi.org/10.1111/pedi.12790. Epub 2018 Nov 13
L.M.B. Laffel, W.V. Tamborlane, A. Yver, G. Simons, J. Wu, V. Nock et al. Pharmacokinetic and pharmacodynamic profile of the sodium-glucose co-transporter-2 inhibitor empagliflozin in young people with Type 2 diabetes: a randomized trial. Diabet. Med. 35(8), 1096–1104 (2018). https://doi.org/10.1111/dme.13629
F. Fuyong Du, S.A. Hinke, C. Cavanaugh, D. Polidori, N. Wallace, T.H. Kirchner et al. Potent Sodium/Glucose Cotransporter SGLT1/2 Dual Inhibition Improves Glycemic Control Without Marked Gastrointestinal Adaptation or Colonic Microbiota Changes in Rodents. Pharmacol. Exp. Ther. 365(3), 676–687 (2018). https://doi.org/10.1124/jpet.118.248575
A.J. Scheen, Reduction in cardiovascular and all-cause mortality in the EMPA-REG OUTCOME trial: a critical analysis. Diabetes Metab. 42(2), 71–6 (2016). https://doi.org/10.1016/j.diabet.2015.12.005
D.K. McCulloch, D.M. Nathan, J.E. Mulder. Management of persistent hyperglycemia in type 2 diabetes mellitus. 2016 (updated 2016, June 10). www.UpToDate.com
American Diabetes Association, Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes 2021. Diabetes Care 44(Suppl. 1), S15–S33 (2021). https://doi.org/10.2337/dc21-S002
Author information
Authors and Affiliations
Contributions
K.K. has the idea for this review. K.K., S.P., N.T. and A.S. performed the literature search. All authors contributed in data analysis. K.K. and A.S. wrote the first draft. All authors critically revised the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karavanaki, K., Paschou, S.A., Tentolouris, N. et al. Type 2 diabetes in children and adolescents: distinct characteristics and evidence-based management. Endocrine 78, 280–295 (2022). https://doi.org/10.1007/s12020-022-03172-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03172-y