Abstract
Introduction
In recent decades, the dramatic rise of obesity among youth in the US has been accompanied by a rise in the prevalence of type 2 diabetes (T2D) in this population. This alarming trend underscores the importance of conducting trials to evaluate new therapies in children with T2D.
Methods
A targeted review of peer-reviewed literature and trials registered on www.clinicaltrials.gov was conducted in January 2021 to identify pharmaceutical interventional studies in youth with T2D. Information regarding enrollment data, study design elements, subjects’ baseline characteristics, and key treatment outcomes was documented.
Results
Among the 16 clinical studies included in this review, only five appeared to meet projected enrollment targets in < 4 years. Although three other studies met recruitment targets, two took approximately 5 years to complete and the third took nearly 10 years.
Conclusions
Despite legislation requiring evaluation of pharmaceutical treatments in pediatric populations, surprisingly few interventional studies have been conducted in children with T2D. This review highlights that recruitment challenges may be impeding the conduct and completion of interventional studies. Consequently, few pharmaceutical treatments have been proven to be effective and approved for children with T2D. Metformin and liraglutide remain the only non-insulin treatments formally approved in the US for use in this population. More clinical research is needed to support regulatory decision-making as well as treatment decisions for children with T2D in clinical settings. Sponsors and investigators will need to implement strategies for improving trial enrollment as well as work with regulatory agencies to develop novel study designs that may require fewer patients.
Similar content being viewed by others
Why carry out this study? |
There has been a dramatic rise of obesity among youth in the US, accompanied by a rise in the prevalence of youth-onset type 2 diabetes (T2D). |
Unlike adults with T2D, treatment options are limited in youth with T2D, underscoring the need to conduct clinical trials evaluating new therapies in children and adolescents with T2D. |
The purpose of the current literature review was to gather updated information on completed interventional phase 3 and 4 studies in youth with T2D and to identify factors that may be limiting research in this area. |
What was learned from the study? |
Relatively few pediatric trials evaluating products for T2D have been completed in the past 20 years, with recruitment challenges likely impeding the conduct and completion of these studies. |
Strategies for improving trial enrollment and potentially leveraging data from outside the traditional trial context could help address the lack of efficacy data in this population. |
Introduction
In recent decades, the increasing prevalence of obesity among youth in the US has been accompanied by a corresponding rise in the prevalence of youth-onset type 2 diabetes (T2D) [1, 2]. The SEARCH for Diabetes in Youth study, a population-based epidemiology and surveillance registry, found an increase of approximately 30% in T2D from 2001 to 2009, with minority youth particularly affected [1, 3]. Though still considered a rare disease among youth, the rising trends point to the growing need for high-quality trials evaluating T2D therapies in children to inform regulatory and clinical decision-making.
The number of pediatric trials has increased over the past 20 years partly due to the passage of US legislation that requires and incentivizes evaluation of medical products in children [4, 5]. These include the Best Pharmaceuticals for Children Act (BPCA) of 2002 and the Pediatric Research Equity Act (PREA) of 2003. While BPCA incentivizes sponsors to voluntarily conduct pediatric research in therapeutic areas beyond the approved adult indication, PREA provides legislative authority to the FDA to require studies in children whenever the use of a new treatment approved in adults is relevant to a pediatric population. Despite these legislative efforts, relatively few trials focusing on treatment for T2D in children have been successfully completed. Consequently, only three (i.e., metformin, insulin, and liraglutide) of the many treatments approved for the treatment of T2D in adults are currently approved for use in children.
The purpose of the current literature review was to gather updated information on completed interventional phase 3 and 4 studies in youth with T2D and to identify factors that may be limiting research in this area.
Methods
Literature Review
A targeted literature search was performed to identify peer-reviewed publications of interventional phase 3 or 4 clinical trials involving the use of one or more pharmaceutical agents for the treatment of T2D in children and adolescents. The search was conducted using Medline and Embase and was restricted to articles written in English and published in 2000 or later. The search was also limited to trials enrolled fully or in part in the US. Key search terms included: (1) diabetes, mellitus, type 2, non-insulin dependent; (2) child, adolescent, pediatric; (3) clinical trial. Adult-only trials, phase 1 and 2 trials, trials with no US patients, case reports, animal trials, and subgroup analyses were excluded. The literature search was conducted on 19 January 2021.
Resulting abstracts identified through the search were reviewed for relevancy. Abstracts were selected for full-text review if they met the pre-determined inclusion criteria. Abstracted information from the peer-reviewed papers included: basic trial information (i.e., sponsor, objective, duration, inclusion/exclusion criteria, etc.), study sample information, key efficacy and safety results, and any information identified regarding recruitment challenges or difficulties.
This review is based on previously conducted studies. No new studies of human or animal subjects were performed by any of the authors for the purpose of conducting this review.
Review of Completed Trials
A search of www.clinicaltrials.gov was conducted to identify any trials that may have been completed but not published. Clinical trials were required to meet the same criteria as noted above. A “completed” study, as defined on the www.clinicaltrials.gov website, is a study that has ended ‘normally’ and whose participants are no longer being examined or treated. After searching for studies listed with a “completed” status, a second search was conducted to identify any studies that had completed enrollment and posted primary data results but were not yet categorized as “completed.” These studies were listed as “active—not recruiting” rather than “completed” because of their ongoing data collection efforts to inform secondary endpoints (e.g., open-label extensions). The clinical trials search was performed on 23 January 2021. Data were abstracted and categorized utilizing the same variables abstracted for the scientific publications noted above.
When information on www.clinicaltrials.gov or in publications was limited, additional internet searches were conducted to identify regulatory review documents or other publicly available sources of information that could provide additional details.
Results
Summary of Completed Pediatric T2D Studies
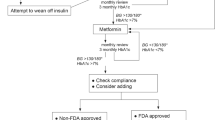
A total of 16 completed interventional studies (phase 3 and 4) among children and adolescents with T2D were identified and included in this review (Fig. 1, Table 1). Thirteen of these studies were funded by a pharmaceutical company; three were funded by a mix of government and academic institutions.
The 16 studies spanned > 2 decades with the earliest study (A) [6] launching in 1998 and the latest completed study having concluded in April 2020 (N) [7] (Table 2). Two studies (O and P) [8, 9] completed data collection in April and May (respectively) 2020 to inform their primary endpoints, but are still ongoing to inform their secondary endpoints. Study duration or enrollment period for the studies varied, ranging from 1–2 years (five trials) to 3–5 years (eight trials) to 6–11 years (four trials). Note study K [10] was a pooled analysis of two clinical trials (NCT01760447 and NCT01472367); the enrollment period for NCT01760447 lasted 5 years and over 6 years for NCT01472367. Ten trials included metformin in at least one treatment arm. Other study drugs (either alone or in combination) included: sulfonylureas, thiazolidinediones, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) agonists, bile acid sequestrants, amylin analogs, sodium-glucose co-transporter-2 (SGLT2) inhibitors, and insulin.
Each study with a peer-reviewed publication (n = 6) is included in all data tables. One study (B) [11] had minimal information posted on www.clinicaltrials.gov and had no publication. However, details of this trial were found in regulatory review documents available online [12, 13], so this study was also included in all tables. Six studies (K, L, M, N, O, and P) [7,8,9,10, 14, 15] with no associated publications had sufficient information posted on www.clinicaltrials.gov to be included in all tables. Three studies (E, F, G) [16,17,18] had sufficient enrollment and study design information posted on the trial registry site to be included in Tables 2 and 3 but were excluded from Table 4 due to lack of available information on study results.
Enrollment and Enrollment Challenges
Most of the 16 studies appeared to have difficulty recruiting patients. Enrollment for eight studies (A, B, C, E, H, J, O, and P) [6, 8, 9, 11, 18,19,20,21,22,23,24] was conducted within a relatively short period of approximately 1–3 years; however, only five of these eight shorter studies (A, C, E, J, and O) [6, 9, 18, 19, 21,22,23] met their projected enrollment numbers. Significant recruitment challenges were reported in the publications associated with studies A and H [6, 20, 24]. Although study A [6] surpassed projected enrollment by ten subjects, the authors described recruitment difficulties related to the study inclusion criteria. In this study, 481 subjects were screened and only 82 were randomized. This high screen failure rate may be in part related to the fact that investigators were screening subjects who had not yet been diagnosed with T2D. The authors also noted that many potential study subjects failed screening based on the required fasting plasma glucose (FPG) levels. For the second of these eight shorter studies (B) [11], projected enrollment information for the trial could not be found but 167 subjects were randomized in the study. For the third shorter study (C) [19, 22], investigators met projected enrollment within approximately 18 months, and recruitment challenges were not mentioned in the publication. Study E [18] achieved its projected enrollment target within 2 years, although the target was only 16 subjects for this government-funded, single-center phase 4 trial. Study J (RISE) [21, 23] investigators were successful in meeting projected enrollment goals within a slightly longer period of time (3 years). Study H [20, 24] ceased enrollment due to unreasonably slow recruitment after 17 months, which resulted in a total of 42 subjects despite an enrollment goal of 358 subjects. The authors did not speculate or provide reasons for the trial’s slow recruitment [24]. Study O [9] slightly exceeded its enrollment target after 3 years of recruitment, but the projected enrollment was relatively modest at only 54 subjects. Study P [8] began recruitment in August 2014; however, recruitment efforts were suspended for approximately a year and a half for unknown reasons. Following re-initiation of recruitment in early 2016, the trial was still unable to meet its projected enrollment of 100 subjects.
Six studies (D, I, K, L, M, and N) [7, 10, 14, 15, 25,26,27,28] appear to have encountered significant recruitment difficulties, with each taking approximately ≥ 5 years to complete and many not meeting enrollment goals. Projected enrollment numbers were not met for studies D, I, K, L, or N [7, 10, 15, 25,26,27,28]. Despite pooling data from two trials, study K [10] still failed to meet the projected enrollment numbers for either of the original studies. Study M [14] met projected enrollment numbers; however, given its lengthy duration (beginning in late 2010 and concluding its recruitment in 2019), it likely experienced enrollment challenges as well.
Finally, two studies (F and G) [16, 17], both examining the safety and efficacy of saxagliptin and conducted by the same study sponsor, appear to have failed because of recruitment challenges. Their final sample sizes were recorded as N = 8 and N = 6, respectively, while projected enrollment for each of these studies was greater than 200 subjects. Based on publicly available regulatory review documents, it appears that the sponsor discontinued enrollment for these trials based on a recommendation from their independent Data Monitoring Committee (DMC) [29]. The DMC noted that the continued slow accrual of subjects was preventing the studies from achieving their objectives. It appears that the sponsor proposed replacing these two terminated studies with a different study (NCT03199053), which is still actively recruiting subjects according to www.clinicaltrials.gov and thus not included in this review.
Study Characteristics and Key Results
The number of enrolling sites varied widely ranging from a single center for 1 of the phase 4 studies (E) [18] to as many as 185 sites (I) [26, 27] (Table 2). Inclusion and exclusion criteria varied across studies; however, there were some similarities (Table 3). Ten studies targeted the age group of 10–17 years, while three studies targeted a slightly younger range (8–16 [A], 9–16 [B], and 8–17 [C]) [6, 11, 19, 22] and three recruited an older group (12–21 years [E], 10–19 years [J], and 10–24 years [O]) [9, 18, 21, 23]. The three studies with younger age ranges were older studies, conducted before regulatory expectations for interventional studies in youth-onset T2D were established, and two of the three studies with older age ranges were academic studies, which would not be subject to these regulatory expectations. The required HbA1c for study enrollment varied slightly across trials and even varied within some trials depending on a subject’s treatment history. The most common required HbA1c range was ≥ 7.0% and ≤ 10.5%. Most studies stipulated a body mass index (BMI) of ≥ 85% (adjusted for age and gender) and/or a weight of ≥ 30 kg. Exclusion criteria also varied across studies; however, some common exclusion criteria included diabetic ketoacidosis, previous use of antidiabetic agents other than metformin, use of corticosteroids, use of weight loss agents, and diabetes of monogenic or secondary etiology.
It is important to note that the largest studies included in this review (D and J) [21, 23, 25, 28], which were both academic- and government-sponsored trials, were not designed to assess effect of treatment on change from baseline in HbA1c or other parameters. Study D (TODAY) [25, 28] was designed to assess time to treatment failure in youth with T2D already under glycemic control treated with metformin, while study J (RISE) [21, 23] compared the effect of insulin followed by metformin with metformin alone in preserving or improving beta-cell function in youth with either impaired glucose tolerance (IGT) or recently diagnosed T2D.
Study E [18] has no posted results on the trial registry site; however, for the 15 trials with available results, there was a wide range of final sample sizes (N = 6 to N = 699) and outcome measures (Table 3). In studies F [17], G [16], and H [20, 24], no efficacy conclusions could be drawn because of their small sample sizes. For 9 of the 13 remaining studies, significant differences between treatment and placebo were found for at least one of the three efficacy measures; however, it is notable that four studies failed to meet their primary endpoints (L, M, N, and O) [7, 9, 14, 15]. Study L [15] (sitagliptin monotherapy), study O [9] (dapaglifloxin), study M [14] (colesevelam), and study N [7] (exenatide twice daily) failed to demonstrate a statistically significant reduction in HbA1c compared with placebo. Study P [8], which assessed the safety and efficacy of exenatide as a once weekly treatment, did meet its primary HbA1c endpoint; however, regulatory decisions regarding approval for its use in children are currently unknown. Finally, although statistically significant results were reported on www.clinicaltrials.gov for study K [10] (sitagliptin + metformin), collectively the results from this study and study L [15] (sitagliptin monotherapy) did not ultimately support pediatric approval in the US. Labelling for sitagliptin was updated in 2020 to note that efficacy in pediatrics was not established.
Safety information, reported for most trials, is shown in Table 3. While difficult to attribute to specific medications given the use of permitted background therapies such as metformin, the most commonly reported adverse events (AEs) across trials were gastrointestinal symptoms/pain, headache, and upper respiratory tract infection. In general, medication safety and tolerability findings in subjects with youth-onset T2D were consistent with those observed in adults.
Patient Baseline Characteristics
Mean age of study subjects ranged from about 13.7 to 16.1 years (Table 4). Excluding four studies (H, I, K, and L) [10, 15, 20, 24, 26, 27], Black subjects represented approximately 25% to 35% of the sample. In studies H [20, 24], I [26, 27], K [10], and L [15], a lower proportion of Black subjects were enrolled and represented only between 2.4% and 11.9% of the sample. Except for study C [19, 22] where White subjects represented < 20% of the sample, White patients represented anywhere from 20% to 65% of the sample in the other 12 studies included in Table 4. Hispanic and Latino subjects typically represented about 30% to 40% of the sample, although study B [11] had only 13% Hispanic/Latino representation and study N [7] had nearly 47% Hispanic/Latino representation. In line with the epidemiology of youth-onset T2D, there was a consistent female majority with about 60% to 70% of the sample being female across the 13 studies included in Table 4.
Mean baseline weight ranged from about 73 to 102 kg and BMI ranged from approximately 28 to nearly 37 kg/m2 depending on the study. Mean baseline HbA1c ranged from 5.7% (J) [21, 23] to approximately 9.0% (A and H) [6, 20, 24]. Only 40% of randomized patients in study J (RISE) [21, 23] had T2D; the rest had IGT, which is likely why this study had the lowest mean baseline HbA1c (5.7%).
Discussion
In spite of legislation designed to increase the number of pharmaceutical treatments evaluated in pediatric populations and good faith efforts by sponsors to conduct trials of new treatments, relatively few interventional phase 3 studies have been successfully enrolled and completed in children with T2D. Only 16 trials met criteria for inclusion in this review, and these studies varied widely in trial duration, number of enrolling sites, and sample size. For ten of these studies, available information was quite limited because results had not been published at the time of this review.
The relative lack of trial data to inform regulatory decisions coupled with the failure of a number of recently completed trials to demonstrate efficacy has led to a paucity of approved medications for children and limited the information available to clinicians caring for these patients. In contrast to the numerous therapies available to adults with T2D, metformin and liraglutide remain the only non-insulin treatments formally approved in the US for use in children with T2D. While most insulins are not specifically indicated for treatment of children with T2D, they are used for this purpose and are recommended in treatment guidelines for patients who present with ketosis or for whom metformin does not provide adequate glycemic control [30]. The approval of liraglutide in June 2019 was the first approval of a medication for treatment of T2D in children since 2000 when metformin was approved. Most of the studies with recently posted results on www.clinicaltrials.gov (other than study P [8], which assessed exenatide once weekly) failed to meet their primary HbA1c endpoint and, in the case of sitagliptin, did not support approval for a pediatric T2D indication. This reiterates the challenges of managing T2D in youth, given its more aggressive course as compared to T2D in adults, and suggests that metformin and liraglutide may, for now, remain the only approved non-insulin options for treating these patients.
The majority of studies included in this review appeared to encounter challenges when recruiting patients. Only five studies (A, C, E, J, and O) [6, 9, 18, 19, 21,22,23] achieved projected enrollment targets in < 4 years, while seven trials (F, G, H, K, L, N, and P) [7, 8, 10, 15,16,17, 20, 24] failed to meet their initial recruitment targets altogether. There was no clear relationship between trial success or recruitment speed and number of sites involved. For example, study I [26, 27] had 109 participants complete the trial after 5 years using 185 sites. However, study C [19, 22] had 210 participants complete after only 2 years using 96 sites, and study J [21, 23] had 86 participants complete after 3 years using four sites. This suggests that when conducting clinical trials in pediatric T2D, careful consideration must be given to the location and type of sites selected. For example, sites in areas that serve communities of color may be able to increase diversity in trials. Moreover, sites that have long-standing and trusted relationships with families (e.g., general practices) may recruit more successfully than sites that do not (e.g., designated research sites that do not regularly see patients or manage their care). There are several factors that may interfere with recruiting pediatric T2D samples. In general, regardless of the medical condition, pediatric samples tend to be more difficult to recruit and retain than adult samples [31, 32]. For diabetes in particular, the low prevalence of T2D in children (i.e., 0.46 per 1000 children aged 10–19 years in the US [1]) further limits the number of potential subjects for trials. Demographic characteristics associated with T2D may also play a role. T2D is particularly prevalent in non-white communities with socioeconomic challenges and poor access to healthcare [33,34,35]. These demographic groups are generally considered difficult to enroll in clinical trials [36]. To address this challenge, investigators or sponsors can select clinical sites that specialize in treatment of pediatric T2D and serve communities with higher proportions of demographic groups that may be difficult to recruit elsewhere.
Restrictive study eligibility requirements may also interfere with recruitment of children with T2D. For example, pediatric T2D trials often exclude children with either very high or near-normal HbA1c levels, which limits the potential pool of trial participants [37]. In addition, many potential patients may be excluded because of obesity-related comorbidities that are common in this population (e.g., hypertension, hyperlipidemia, obstructive sleep apnea) [38,39,40]. These restrictive eligibility requirements may be the reason for the high rate of screen failures in trials included in the current review. In most of the trials that eventually met enrollment targets (e.g., C, D, I, and J) [19, 21,22,23, 25,26,27,28], only 40% to 60% of potential subjects assessed for eligibility were randomized. Adult T2D trials generally report similarly high rates of screen failures [41,42,43,44]. However, because T2D is more common in adults than in children, there is a larger pool of adult patients, and it may be more feasible to meet recruitment targets despite high screen failure rates. To maximize the pool of potential patients and minimize screen failures, researchers designing clinical trials may want to consider less restrictive eligibility criteria and allow for more comorbidities, a wider HbA1c range, and increased variety of pre-trial medication treatments.
One approach for locating and retaining pediatric patients for trials may be to engage members of children’s social and medical support network. These individuals can act as advisors reviewing protocols, procedures, and consent forms during the study design process. For example, parents and pediatricians may be able to identify potential recruitment or retention problems that can be addressed prior to finalizing study materials. Unlike with type 1 diabetes, there is little organized advocacy activity specific to pediatric T2D. Advocacy groups that do exist seem to be mostly local rather than national in scale. As awareness of pediatric T2D grows, patient advocacy groups may emerge and play a facilitative role in trial recruitment for this population.
Finally, it may not always be necessary to design and conduct a traditional fully randomized controlled clinical trial to evaluate treatments in this population. It may be possible to use alternative study approaches and designs to assess treatment outcomes while limiting the number of patients needed for trials [45, 46]. For example, the use of master protocols and other collaborative approaches, while requiring extensive cooperation and engagement from investigators, regulatory agencies, and pharmaceutical companies, could potentially facilitate more efficient completion of trials or focus efforts on the most promising drugs to be tested [45, 46]. Augmenting the placebo arm of a clinical trial with historical controls from prior trials or from well-curated and matched real-world cohorts also holds the potential to decrease the overall size of trials and limit exposure to placebo in those trials while potentially increasing power to detect efficacy signals [47, 48]. In addition, should we find, as we come to better understand youth-onset T2D, that the response to therapies is sufficiently similar to that in adults, sponsors may be able to extrapolate from adult data based on pharmacokinetic and pharmacologic data from adolescents with T2D [49]. Future use of such innovative approaches will require careful consultation and coordination between industry sponsors and regulators.
Findings of this literature review should be interpreted in the context of several limitations. First, the level of detail in this review was limited by the information provided in the original sources. Second, even among the published studies, the sample characteristics, endpoints, and study designs varied. This heterogeneity makes it difficult to identify trends and draw conclusions across studies. Third, there were several instances where information on www.clinicaltrials.gov diverged from the published articles, leading to some uncertainty in the findings.
Conclusion
Overall, this review highlights limitations and challenges in research on treatment for T2D in pediatric populations. Compared to the body of clinical research in adult patients with T2D, few studies have been conducted in children. Furthermore, many pediatric T2D studies have failed to meet sample size targets, likely because of recruitment challenges. Several recently completed trials, including those that assessed the safety and efficacy of DPP-4 inhibitors and SGLT2 inhibitors, failed to meet their primary HbA1c endpoints. Consequently, few pharmaceutical treatments have been proven to be effective and approved for use in this population. With over 30 new T2D medications currently in the phase 2 development pipeline across sponsors, the number of phase 3 trials in pediatric patients with T2D is only expected to grow in the near future [50]. To address these challenges, sponsors and investigators will need to implement strategies for improving clinical trial enrollment and potentially leverage data from outside the traditional trial context.
References
Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–86.
Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr. 1996;128(5 Pt 1):608–15.
Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med. 2017;376(15):1419–29.
Vernon JA, Shortenhaus SH, Mayer MH, Allen AJ, Golec JH. Measuring the patient health, societal and economic benefits of US pediatric therapeutics legislation. Paediatr Drugs. 2012;14(5):283–94.
Yen E, Davis JM, Milne CP. Impact of Regulatory incentive programs on the future of pediatric drug development. Ther Innov Regul Sci. 2019;53(5):609–14.
Jones KL, Arslanian S, Peterokova VA, Park JS, Tomlinson MJ. Effect of metformin in pediatric patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2002;25(1):89–94.
AstraZeneca, Quintiles I, ClinicalTrials.Gov. Safety and efficay of exenatide as monotherapy and adjunctive therapy to oral antidiabetic agents in adolescents with type 2 diabetes. ClinicalTrials.gov Identifier: NCT00658021. Last update posted: December 1, 2020 [updated Last update posted: December 1, 2020; cited January 23, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT00658021.
AstraZeneca, ClinicalTrials.Gov. Safety and efficacy study of exenatide once weekly in adolescents with type 2 diabetes. ClinicalTrials.gov Identifier: NCT01554618. Last update posted: January 7, 2021 [updated Last update posted: January 7, 2021; cited January 23, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01554618.
AstraZeneca, ClinicalTrials.Gov. Study to evaluate safety and efficacy of dapagliflozin in patients with type 2 diabetes mellitus aged 10-24 years. ClinicalTrials.gov Identifier: NCT02725593. Last update posted: December 2, 2020 [updated Last update posted: December 2, 2020; cited January 23, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT02725593.
Merck Sharp & Dohme Corp, ClinicalTrials.Gov. A pooled analysis of the safety and efficacy of MK-0431A and MK-0431A XR in pediatric participants with type 2 diabetes mellitus with inadequate glycemic control on metformin therapy (Alone or in Combination With Insulin) (MK-0431A-170/MK-0431A-289). ClinicalTrials.gov Identifier: NCT01760447. Last update posted: November 16, 2020 [updated Last update posted: November 16, 2020; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01760447.
Bristol-Myers Squibb (BMS), ClinicalTrials.Gov. A research study to determine the safety and efficacy of glucovance compared to metformin and glyburide in children and adolescents with type 2 diabetes. ClinicalTrials.gov Identifier: NCT00035542. Last update posted: April 15, 2011 [updated Last update posted: April 15, 2011; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT00035542.
Center for Drug Evaluation and Research (CDER). Statistical Review and Evaluation: Clinical Studies (NDA 21–178) - Glucovance (glyburide and metformin hydrochloride) tablets. Submission: July 21, 2003; PDUFA: January 21, 2004b. p. 13.
Center for Drug Evaluation and Research (CDER), Misbin RI. Application Type: Glyburide/Metformin tablets -- Use of Glucovance in pediatric patients with type 2 diabetes (NDA 21–178). Document date: July 21, 2003; Review date: January 12, 2004a.
Daiichi Sankyo Inc., ClinicalTrials.Gov. Colesevelam for children with type 2 diabetes (WELKid DM). ClinicalTrials.gov Identifier: NCT01258075. Last update posted: February 24, 2021 [updated Last update posted: February 24, 2021; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01258075.
Merck Sharp & Dohme Corp, ClinicalTrials.Gov. Study to Assess safety and efficacy of sitagliptin as initial oral therapy for treatment of type 2 diabetes mellitus in pediatric participants (MK-0431-083). ClinicalTrials.gov Identifier: NCT01485614. Last update posted: December 16, 2020 [updated Last update posted: December 16, 2020; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01485614.
AstraZeneca, Bristol-Myers Squibb (BMS), ClinicalTrials.Gov. A multicenter, randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of saxagliptin (BMS-477118) in combination with metformin ir or metformin XR in pediatric patients with type 2 diabetes who have inadequate glycemic control on metformin alone. ClinicalTrials.gov Identifier: NCT01434186. Last update posted: April 18, 2017 [updated Last update posted: April 18, 2017; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01434186.
AstraZeneca, ClinicalTrials.Gov. Study to evaluate the efficacy, safety, tolerability, and pharmacokinetics of saxagliptin as monotherapy in pediatric patients with type 2 diabetes. ClinicalTrials.gov Identifier: NCT01204775. Last update posted: April 18, 2017 [updated Last update posted: April 18, 2017; cited March 12, 2020]; Available from: https://clinicaltrials.gov/ct2/show/NCT01204775.
Baylor College of Medicine, National Institutes of Health (NIH), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), ClinicalTrials.Gov. The Effect of Byetta and Symlin on Post-meal Meal Blood Sugar Levels in Children With Type 2 Diabetes (T2DM). ClinicalTrials.gov Identifier: NCT00950677. Last update posted: April 24, 2017 [updated Last update posted: April 24, 2017; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT00950677.
Gottschalk M, Danne T, Vlajnic A, Cara JF. Glimepiride versus metformin as monotherapy in pediatric patients with type 2 diabetes: a randomized, single-blind comparative study. Diabetes Care. 2007;30(4):790–4.
Novo Nordisk A/S, ClinicalTrials.Gov. A trial investigating the efficacy and safety of insulin detemir versus insulin NPH in combination with metformin and diet/exercise in children and adolescents with type 2 diabetes insufficiently controlled on metformin with or without other oral antidiabetic Drug(s) With or without basal insulin (iDEAt2). ClinicalTrials.gov Identifier: NCT02131272. Last update posted: September 10, 2018 [updated Last update posted: September 10, 2018; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT02131272.
RISE Study Group, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), ClinicalTrials.Gov. RISE Pediatric Medication Study (RISE Peds). ClinicalTrials.gov Identifier: NCT01779375. Last update posted: December 10, 2019 [updated Last update posted: December 10, 2019; cited January 23, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01779375.
Sanofi, ClinicalTrials.Gov. Glimepiride vs metformin as monotherapy in pediatric subjects with type 2 diabetes mellitus. ClinicalTrials.gov Identifier: NCT00353691. Last update posted: January 11, 2011 [updated Last update posted: January 11, 2011; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT00353691.
The RISE Consortium. Impact of insulin and metformin versus metformin alone on β-cell function in youth with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care. 2018;41(8):1717–25.
Wheeler MD, Barrientos-Perez M, Lo FS, Liang B, Lunsford A, Thorisdottir O, et al. A 26-week, randomized trial of insulin detemir versus NPH insulin in children and adolescents with type 2 diabetes (iDEAt2). Eur J Pediatr. 2018;177(10):1497–503.
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), ClinicalTrials.Gov. Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY). ClinicalTrials.gov Identifier: NCT00081328. Last update posted: March 4, 2020 [updated Last update posted: March 4, 2020; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT00081328.
Novo Nordisk A/S, ClinicalTrials.Gov. Efficacy and safety of liraglutide in combination with metformin compared to metformin alone, in children and adolescents with type 2 diabetes (Ellipse™). ClinicalTrials.gov Identifier: NCT01541215. Last update posted: October 1, 2020 [updated Last update posted: October 1, 2020; cited March 2, 2021]; Available from: https://clinicaltrials.gov/ct2/show/NCT01541215.
Tamborlane WV, Barrientos-Perez M, Fainberg U, Frimer-Larsen H, Hafez M, Hale PM, et al. Liraglutide in children and adolescents with type 2 diabetes. N Engl J Med. 2019;381(7):637–46.
Zeitler P, Hirst K, Pyle L, Linder B, Copeland K, Today Study Group, et al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012;366(24):2247–56.
European Medicines Agency (EMA). Assessment report for paediatric studies submitted in accordance with article 46 of regulation (EC) No 1901/2006, as amended: Onglyza (saxagliptin). London, UK; 17 August 2017; p. 7.
Zeitler P, Arslanian S, Fu J, Pinhas-Hamiel O, Reinehr T, Tandon N, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Type 2 diabetes mellitus in youth. Pediatr Diabetes. 2018;19(Suppl 27):28–46.
Denhoff ER, Milliren CE, de Ferranti SD, Steltz SK, Osganian SK. Factors associated with clinical research recruitment in a pediatric academic medical center–a web-based survey. PLoS ONE. 2015;10(10):e0140768.
Nguyen TT, Jayadeva V, Cizza G, Brown RJ, Nandagopal R, Rodriguez LM, et al. Challenging recruitment of youth with type 2 diabetes into clinical trials. J Adolesc Health. 2014;54(3):247–54.
Clark ML, Utz SW. Social determinants of type 2 diabetes and health in the United States. World J Diabetes. 2014;5(3):296–304.
Grintsova O, Maier W, Mielck A. Inequalities in health care among patients with type 2 diabetes by individual socio-economic status (SES) and regional deprivation: a systematic literature review. Int J Equity Health. 2014;2(13):43.
Piccolo RS, Duncan DT, Pearce N, McKinlay JB. The role of neighborhood characteristics in racial/ethnic disparities in type 2 diabetes: results from the Boston Area Community Health (BACH) Survey. Soc Sci Med. 2015;130:79–90.
Mosenifar Z. Population issues in clinical trials. Proc Am Thorac Soc. 2007;4(2):185–7 (discussion 7-8).
Tamborlane WV, Chang P, Kollman C, Klingensmith GJ, Ruedy K, Gal RL, et al. Eligibility for clinical trials is limited for youth with type 2 diabetes: Insights from the Pediatric Diabetes Consortium T2D Clinic Registry. Pediatr Diabetes. 2018;19(8):1379–84.
Iglay K, Hannachi H, Joseph Howie P, Xu J, Li X, Engel SS, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243–52.
Luijks H, Schermer T, Bor H, van Weel C, Lagro-Janssen T, Biermans M, et al. Prevalence and incidence density rates of chronic comorbidity in type 2 diabetes patients: an exploratory cohort study. BMC Med. 2012;29(10):128.
Okosun IS, Chandra KM, Choi S, Christman J, Dever GE, Prewitt TE. Hypertension and type 2 diabetes comorbidity in adults in the United States: risk of overall and regional adiposity. Obes Res. 2001;9(1):1–9.
Eckel RH, Henry RR, Yue P, Dhalla A, Wong P, Jochelson P, et al. Effect of ranolazine monotherapy on glycemic control in subjects with type 2 diabetes. Diabetes Care. 2015;38(7):1189–96.
Forst T, Koch C, Dworak M. Vildagliptin versus insulin in patients with type 2 diabetes mellitus inadequately controlled with sulfonylurea: results from a randomized, 24 week study. Curr Med Res Opin. 2015;31(6):1079–84.
Shestakova MV, Wilding JPH, Wilpshaar W, Tretter R, Orlova VL, Verbovoy AF. A phase 3 randomized placebo-controlled trial to assess the efficacy and safety of ipragliflozin as an add-on therapy to metformin in Russian patients with inadequately controlled type 2 diabetes mellitus. Diabetes Res Clin Pract. 2018;146:240–50.
Wang W, Ning G, Ma J, Liu X, Zheng S, Wu F, et al. A randomized clinical trial of the safety and efficacy of sitagliptin in patients with type 2 diabetes mellitus inadequately controlled by acarbose alone. Curr Med Res Opin. 2017;33(4):693–9.
Khan T, Stewart M, Blackman S, Rousseau R, Donoghue M, Cohen K, et al. Accelerating pediatric cancer drug development: challenges and opportunities for pediatric master protocols. Therap Innov Regul Sci. 2019;53(2):270–8.
Zeitler P, Chou HS, Copeland KC, Geffner M. Clinical trials in youth-onset type 2 diabetes: needs, barriers, and options. Curr Diab Rep. 2015;15(5):28.
Ghadessi M, Tang R, Zhou J, Liu R, Wang C, Toyoizumi K, et al. A roadmap to using historical controls in clinical trials - by Drug Information Association Adaptive Design Scientific Working Group (DIA-ADSWG). Orphanet J Rare Dis. 2020;15(1):69.
Viele K, Berry S, Neuenschwander B, Amzal B, Chen F, Enas N, et al. Use of historical control data for assessing treatment effects in clinical trials. Pharm Stat. 2014;13:41–54.
Barrett JS, Bucci-Rechtweg C, Amy Cheung SY, Gamalo-Siebers M, Haertter S, Karres J, et al. Pediatric extrapolation in type 2 diabetes: future implications of a workshop. Clin Pharmacol Therap. 2020.
PhRMA. 2019 Medicines in Development for Diabetes and Related Conditions. 2019 [updated 2019; cited April 15, 2020]. https://www.phrma.org/-/media/Project/PhRMA/PhRMA-Org/PhRMA-Org/PDF/M-O/MID-Diabetes-Drug-List-2019.pdf. Accessed 1 May 2021.
Copeland KC, Zeitler P, Geffner M, Guandalini C, Higgins J, Hirst K, et al. Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. J Clin Endocrinol Metab. 2011;96(1):159–67.
European Medicines Agency (EMA). Assessment report for paediatric studies submitted according to Article 46 of the Regulation (EC) No 1901/2006: Insulatard (insulin analogue human recombinant). Procedure no: EMEA/H/C/000441/P46/027. London, UK; 23 February 2017b.
Acknowledgements
The authors thank Stacy Holdsworth, Sarah Curtis, and David Ceryak for comments on an earlier draft of the manuscript.
Funding
Funding for this study was provided by Eli Lilly and Company, including the journal’s Rapid Service Fee and editorial support. The sponsor participated in the study design, review and interpretation of data, and manuscript preparation and review.
Editorial Assistance
The authors thank Amara Tiebout and Dawn Ri’chard of Evidera for editorial assistance. Payment for editorial assistance was included in the funding provided by Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
BMC, TAH, LSM, JAJ, and DAC collaborated on the study design, analysis and interpretation of data, and drafting of the manuscript. Additionally, BMC and TAH supported data collection and data management efforts. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Disclosures
Louis Matza and Timothy Howell are employees of Evidera, a company that received funding from Eli Lilly for time spent conducting this research. Brooke Currie was also an employee of Evidera at the time of writing. Joseph Johnston and David Cox are full-time employees and shareholders of Eli Lilly and Company.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human or animal participants performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Currie, B.M., Howell, T.A., Matza, L.S. et al. A Review of Interventional Trials in Youth-Onset Type 2 Diabetes: Challenges and Opportunities. Diabetes Ther 12, 2827–2856 (2021). https://doi.org/10.1007/s13300-021-01136-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01136-5