Abstract
Purpose
Acromegaly is a rare disease due to growth hormone (GH)-secreting pituitary adenoma. GH and IGF-1 levels are usually congruent, indicating either remission or active disease; however, a discrepancy between GH and IGF-1 may occur. We aimed to evaluate the outcome of diabetes mellitus (DM) and hypertension (HT) in acromegalic patients with congruent GH and/or IGF-1 levels vs. discordant biochemical parameters.
Methods
Retrospective analysis of the data of 3173 patients from the Liege Acromegaly Survey (LAS) allowed us to include 190 patients from 8 tertiary referral centers across Europe, treated by surgery, with available data concerning DM and HT both at diagnosis and at the last follow-up (LFU). We recorded the number of anti-HT and anti-DM drugs used at the first evaluation and at LFU for every patient.
Results
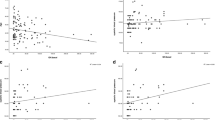
Ninety-nine patients belonged to the REM group (concordant parameters), 65 patients were considered as GHdis (high random GH/controlled IGF-1), and 26 patients were considered as IGF-1dis (high IGF-1/controlled random GH). At diagnosis, 72 patients (37.8%) had HT and 54 patients had DM (28.4%). There was no statistically significant difference in terms of the number of anti-HT and anti-DM drugs at diagnosis versus LFU (mean duration: 7.3 ± 4.5 years) between all three groups.
Conclusion
The long-term outcome of DM and HT in acromegaly does not tend to be more severe in patients with biochemical discordance in comparison with patients considered as in remission on the basis of concordant biological parameters, suggesting that patients with biochemical discordance do not require a closer follow-up.


Similar content being viewed by others
References
A. Colao, L.F.S. Grasso, A. Giustina, S. Melmed, P. Chanson, A.M. Pereira, R. Pivonello, Acromegaly. Nat. Rev. Dis. Prim. 5, 20 (2019)
M.R. Gadelha, L. Kasuki, D.S.T. Lim, M. Fleseriu, Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr. Rev. 40, 268 (2019)
A. Giustina, A. Barkan, A. Beckers, N. Biermasz, B.M.K. Biller, C. Boguszewski, M. Bolanowski, V. Bonert, M.D. Bronstein, F.F. Casanueva, D. Clemmons, A. Colao, D. Ferone, M. Fleseriu, S. Frara, M.R. Gadelha, E. Ghigo, M. Gurnell, A.P. Heaney, K. Ho, A. Ioachimescu, L. Katznelson, F. Kelestimur, J. Kopchick, M. Krsek, S. Lamberts, M. Losa, A. Luger, P. Maffei, M. Marazuela, G. Mazziotti, M. Mercado, P. Mortini, S. Neggers, A.M. Pereira, S. Petersenn, M. Puig-Domingo, R. Salvatori, I. Shimon, C. Strasburger, S. Tsagarakis, A.J. van der Lely, J. Wass, M.C. Zatelli, S. Melmed, A consensus on the diagnosis and treatment of acromegaly comorbidities: an update. J. Clin. Endocrinol. Metab. 105, e937 (2020)
P. Kamenický, G. Mazziotti, M. Lombès, A. Giustina, P. Chanson, Growth hormone, insulin-like growth Factor-1, and the kidney: pathophysiological and clinical implications. Endocr. Rev. 35, 234 (2014)
S. Puglisi, M. Terzolo, Hypertension and acromegaly. Endocrinol. Metab. Clin. N. Am. 48, 779 (2019)
S. Frara, F. Maffezzoni, G. Mazziotti, A. Giustina, Current and emerging aspects of diabetes mellitus in acromegaly. Trends Endocrinol. Metab. 27, 470 (2016)
D. Niculescu, M. Purice, M. Coculescu, Insulin-like growth factor-I correlates more closely than growth hormone with insulin resistance and glucose intolerance in patients with acromegaly. Pituitary 16, 168 (2013)
O.M. Dekkers, N.R. Biermasz, A.M. Pereira, J.A. Romijn, J.P. Vandenbroucke, Mortality in acromegaly: a metaanalysis. J. Clin. Endocrinol. Metab. 93, 61 (2008)
L. Katznelson, E.R. Laws, S. Melmed, M.E. Molitch, M.H. Murad, A. Utz, J.A.H. Wass, Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99(11), 3933–3951 (2014)
L. Maione, T. Brue, A. Beckers, B. Delemer, P. Petrossians, F. Borson-Chazot, O. Chabre, P. Fran‡ois, J. Bertherat, C. Cortet-Rudelli, P. Chanson, Changes in the management and comorbidities of acromegaly over three decades: The French acromegaly registry. Eur. J. Endocrinol. 176(5), 645–655 (2017)
S. Melmed, M.D. Bronstein, P. Chanson, A. Klibanski, F.F. Casanueva, J.A.H. Wass, C.J. Strasburger, A. Luger, D.R. Clemmons, A. Giustina, A consensus statement on acromegaly therapeutic outcomes. Nat. Rev. Endocrinol. 14, 552 (2018)
C.R. Ku, E.Y. Choe, J.W. Hong, E.H. Kim, S.H. Park, S.H. Kim, E.J. Lee, No differences in metabolic outcomes between nadir GH 0.4 and 1.0 ng/mL during OGTT in surgically cured acromegalic patients (observational study). Medicine 95, e3808 (2016)
F. Bolfi, A.F. Neves, C.L. Boguszewski, V.S. Nunes-Nogueira, Mortality in acromegaly decreased in the last decade: a systematic review and meta-analysis. Eur. J. Endocrinol. 179, 59 (2018)
A. Colao, L.F.S. Grasso, M. Di Cera, P. Thompson-Leduc, W.Y. Cheng, H.C. Cheung, M.S. Duh, M.P. Neary, A.M. Pedroncelli, R. Maamari, R. Pivonello, Association between biochemical control and comorbidities in patients with acromegaly: an Italian longitudinal retrospective chart review study. J. Endocrinol. Investig. 43(4), 529–538 (2020)
J.A. Brzana, C.G. Yedinak, J.B. Delashaw, H.S. Gultelkin, D. Cook, M. Fleseriu, Discordant growth hormone and IGF-1 levels post pituitary surgery in patients with acromegaly na‹ve to medical therapy and radiation: what to follow, GH or IGF-1 values? Pituitary 15(4), 562–570 (2012)
P. Petrossians, M.A. Tichomirowa, A. Stevenaert, D. Martin, A.F. Daly, A. Beckers, The Liege Acromegaly Survey (LAS): a new software tool for the study of acromegaly. Ann. Endocrinol. 73, 190 (2012)
P. Petrossians, A.F. Daly, E. Natchev, L. Maione, K. Blijdorp, M. Sahnoun-Fathallah, R. Auriemma, A.M. Diallo, A.-L. Hulting, D. Ferone, V. Hana, S. Filipponi, C. Sievers, C. Nogueira, C. Fajardo-Montañana, D. Carvalho, V. Hana, G.K. Stalla, M.-L. Jaffrain-Réa, B. Delemer, A. Colao, T. Brue, S.J.C.M.M. Neggers, S. Zacharieva, P. Chanson, A. Beckers, Acromegaly at diagnosis in 3173 patients from the Liège Acromegaly Survey (LAS) Database. Endocr. Relat. Cancer 24, 505 (2017)
E.O. Machado, G.F. Taboada, L.V. Neto, F.R. van Haute, L.L. Corrêa, G.A. Balarini, Y. Shrank, M. Goulart, M.R. Gadelha, Prevalence of discordant GH and IGF-I levels in acromegalics at diagnosis, after surgical treatment and during treatment with octreotide LAR®. Growth Horm. IGF Res. 18, 389 (2008)
F.Gatto, C. Campana, F. Cocchiara, G. Corica, M. Albertelli, M. Boschetti, G. Zona, D. Criminelli, M. Giusti, D. Ferone, Current perspectives on the impact of clinical disease and biochemical control on comorbidities and quality of life in acromegaly. Rev. Endocr. Metab. Disord. 20(3), 365–381 (2019)
I.M. Holdaway, R.C. Rajasoorya, G.D. Gamble, Factors influencing mortality in acromegaly. J. Clin. Endocrinol. Metab. 89, 667 (2004)
G.A. Kanakis, A. Chrisoulidou, A. Bargiota, Z.A. Efstathiadou, L. Papanastasiou, A. Theodoropoulou, S.K.Tigas, D.A. Vassiliadi, S. Tsagarakis, M. Alevizaki, The ongoing challenge of discrepant growth hormone and insulin-like growth factor I results in the evaluation of treated acromegalic patients: a systematic review and meta-analysis. Clin. Endocrinol. 85(5), 681–688 (2016)
J. D. Carmichael, V.S. Bonert, J.M. Mirocha, S. Melmed, The utility of oral glucose tolerance testing for diagnosis and assessment of treatment outcomes in 166 patients with acromegaly. J. Clin. Endocrinol. Metab. 94(2), 523–527 (2009)
A.N. Paisley, K. Hayden, A. Ellis, J. Anderson, G. Wieringa, P.J. Trainer, Pegvisomant interference in GH assays results in underestimation of GH levels. Eur. J. Endocrinol. 156, 315 (2007)
T.J. Reid, Z. Jin, W. Shen, C.M. Reyes-Vidal, J.C. Fernandez, J.N. Bruce, J. Kostadinov, K.D. Post, P.U. Freda, IGF-1 levels across the spectrum of normal to elevated in acromegaly: relationship to insulin sensitivity, markers of cardiovascular risk and body composition. Pituitary 18, 808 (2015)
C. Reyes-Vidal, J.C. Fernandez, J.N. Bruce, C. Crisman, I.M. Conwell, J. Kostadinov, E.B. Geer, K.D. Post, P.U. Freda, Prospective study of surgical treatment of acromegaly: effects on ghrelin, weight, adiposity, and markers of CV risk. J. Clin. Endocrinol. Metab. 99, 4124 (2014)
O. Alexopoulou, M. Bex, R. Abs, G. T’Sjoen, B. Velkeniers, D. Maiter, Divergence between growth hormone and insulin-like growth factor-I concentrations in the follow-up of acromegaly. J. Clin. Endocrinol. Metab. 93, 1324 (2008)
K.-C. Leung, G. Johannsson, G.M. Leong, K.K.Y. Ho, Estrogen regulation of growth hormone action. Endocr. Rev. 25, 693 (2004)
M. Matta, V. Bongard, S. Grunenwald, J.-C. Maiza, A. Bennet, P. Caron, Clinical and metabolic characteristics of acromegalic patients with high IGF1/normal GH levels during somatostatin analog treatment. Eur. J. Endocrinol. 164, 885 (2011)
M. Hage, P. Kamenicky, P. Chanson, Growth hormone response to oral glucose load: from normal to pathological conditions. Neuroendocrinology 108, 244 (2019)
A. Pokrajac, G. Wark, A.R. Ellis, J. Wear, G.E. Wieringa, P.J. Trainer, Variation in GH and IGF-I assays limits the applicability of international consensus criteria to local practice. Clin. Endocrinol. 67, 65 (2007)
A.M. Arafat, M. M”hlig, M.O. Weickert, F.H. Perschel, J. Purschwitz, J. Spranger, C.J. Strasburger, C. Sch”fl, A.F.H. Pfeiffer, Growth hormone response during oral glucose tolerance test: the impact of assay method on the estimation of reference values in patients with acromegaly and in healthy controls, and the role of gender, age, and body mass index. J. Clin. Endocrinol. Metab. 93(4), 1254–1262 (2008)
M. Bidlingmaier, P.U. Freda, Measurement of human growth hormone by immunoassays: Current status, unsolved problems and clinical consequences. Growth Horm. IGF Res. 20, 19 (2010)
J.O.L. Jørgensen, M. Krag, N. Jessen, H. Nørrelund, E.T. Vestergaard, N. Møller, J.S. Christiansen, Growth Hormone and Glucose Homeostasis. Horm. Res. Paediatr. 62, 51 (2004)
J. Dal, M. Klose, A. Heck, M. Andersen, C. Kistorp, E.H. Nielsen, J. Bollerslev, U. Feldt-Rasmussen, J.O.L. Jørgensen, Targeting either GH or IGF-I during somatostatin analogue treatment in patients with acromegaly: a randomized multicentre study. Eur. J. Endocrinol. 178, 65 (2018)
M. Christiansen Arlien-Søborg, C. Trolle, E. Alvarson, A. Bæk, J. Dal, J.O.L. Jørgensen, Biochemical assessment of disease control in acromegaly: reappraisal of the glucose suppression test in somatostatin analogue (SA) treated patients. Endocrine 56, 589 (2017)
L. Katznelson, J.L.D. Atkinson, D.M. Cook, S.Z. Ezzat, A.H. Hamrahian, K.K. Miller, American Association of Clinical Endocrinologists, American Association of Clinical Endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of acromegaly—2011 update. Endocr. Pract. 17(Supplement 4), 1–44 (2011)
L. Maione, P. Chanson, National acromegaly registries. Best Pract. Res. Clin. Endocrinol. Metab. 33, 101264 (2019)
Acknowledgements
This work was funded by an unrestricted grant from IPSEN to Albert Beckers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amodru, V., Petrossians, P., Colao, A. et al. Discordant biological parameters of remission in acromegaly do not increase the risk of hypertension or diabetes: a study with the Liege Acromegaly Survey database. Endocrine 70, 134–142 (2020). https://doi.org/10.1007/s12020-020-02387-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02387-1