Abstract
Purpose
There are multiple risk factors have different influence on the disorder. However, the risk of hyperuricemia and gout in different socioeconomic status (SES) remains unclear. Recent studies provided results that contradicted to former studies. We aimed to perform a systematic review and meta-analysis of evidence to date and to assess the associations between SES and hyperuricemia or gout worldwide.
Methods
We searched MEDLINE, EMBASE, and Web of Science databases to identify studies that investigated the association between SES and hyperuricemia or gout. Studies that presented risk estimates were included. We conducted meta-analyses using random effects to combine unadjusted and adjusted effect estimates.
Results
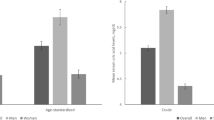
Data from 14 studies were included, 9 provided data about hyperuricemia and 5 provided gout. Overall, there was an association between higher educational level and a higher risk of hyperuricemia (POR = 1.38, 95% CI 1.04–1.73) but lower risk of gout (POR = 0.59, 95% CI 0.47–0.71). Subgroup meta-analysis showed no association between all SES measures and hyperuricemia or gout in males or females.
Conclusions
Our study suggested that the associations between SES and hyperuricemia gout are different. Higher educational level was related to a higher risk of hyperuricemia but lower risk of gout. Given the limitations of our study, future studies are needed to investigate specific mechanisms underlying the relationship among SES differences in hyperuricemia and gout. Strategies to prevent and control SES inequalities in hyperuricemia and gout should be explored and adopted.



Similar content being viewed by others
Data availability
This is a systematic review of the literature, all the data presented are available and cited in the references section.
References
N. Dalbeth, T.R. Merriman, L.K. Stamp, Gout. Lancet 388, 2039 (2016)
C.-F. Kuo, M.J. Grainge, W. Zhang, M. Doherty, Global epidemiology of gout: prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 11, 649 (2015)
T. Bardin, P. Richette, Impact of comorbidities on gout and hyperuricaemia: an update on prevalence and treatment options. BMC Med. 15, 123 2017)
A.E. Hak, G.C. Curhan, F. Grodstein, H.K. Choi, Menopause, postmenopausal hormone use and risk of incident gout. Ann. Rheum. Dis. 69, 1305–1309 (2010). https://doi.org/10.1136/ard.2009.109884
P.C. Robinson, Gout—an update of aetiology, genetics, co-morbidities and management. Maturitas 118, 67 (2018)
C.J. Smyth, C.W. Cotterman, R.H. Freyberg, The genetics of gout and hyperuricemie—an analysis of nineteen familes. J. Clin. Investig. 27, 749–759 (1948). https://doi.org/10.1172/JCI102025
S.W. Lai, C.K. Tan, K.C. Ng, Epidemiology of hyperuricemia in the elderly. Yale J. Biol. Med. 74, 151–157 (2001)
R. Villegas, Y.-B. Xiang, Q. Cai, S. Fazio, M. Linton, H. Li, T. Elasy, W. Zheng, X.O. Shu, Prevalence and determinants of hyperuricemia in middle-aged, Urban Chinese men. Metab. Syndr. Relat. Disord. 8, 263–270 (2010). https://doi.org/10.1089/met.2009.0084
M.A. McAdams-Demarco, A. Law, J.W. Maynard, J. Coresh, A.N. Baer, Risk factors for incident hyperuricemia during mid-adulthood in African American and White men and women enrolled in the ARIC cohort study. BMC Musculoskelet. Disord. 14 (2013). https://doi.org/10.1186/1471-2474-14-347
Y.L. Qu, L. Yu, Z.M. Li, L.H. Kong, T.C. Xiao, M. Li, N.N. Luo, X.F. Deng, K.Y. Qu, Epidemiological status and risk factors of hyperuricemia in rural area of the Three Gorges. Chin. J. Cardiol. 41, 427–431 (2013). https://doi.org/10.3760/cma.j.issn.0253-3758.2013.05.015
L. Liu, S. Lou, K. Xu, Z. Meng, Q. Zhang, K. Song, Relationship between lifestyle choices and hyperuricemia in Chinese men and women. Clin. Rheumatol. 32, 233–239 (2013). https://doi.org/10.1007/s10067-012-2108-z
P. Song, H. Wang, W. Xia, X. Chang, M. Wang, L. An, Prevalence and correlates of hyperuricemia in the middle-aged and older adults in China. Sci. Rep. 8, 4314 2018). https://doi.org/10.1038/s41598-018-22570-9
Y. Kim, J. Kang, G.T. Kim, Prevalence of hyperuricemia and its associated factors in the general Korean population: an analysis of a population-based nationally representative sample. Clin. Rheumatol. 37, 2529–2538 (2018). https://doi.org/10.1007/s10067-018-4130-2
Y. Shen, Y. Wang, C. Chang, S. Li, W. Li, B. Ni, Prevalence and risk factors associated with hyperuricemia among working population at high altitudes: a cross-sectional study in Western China. Clin. Rheumatol. 38, 1375–1384 (2019). https://doi.org/10.1007/s10067-018-4391-9
D.F. Stroup, J.A. Berlin, S.C. Morton, I. Olkin, G.D. Williamson, D. Rennie, D. Moher, B.J. Becker, T.A. Sipe, S.B. Thacker,and for the M.O.O.S. in E. Group, Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283, 2008 (2000). https://doi.org/10.1001/jama.283.15.2008
J.P. Vandenbroucke, E. von Elm, D.G. Altman, P.C. Gotzsche, C.D. Mulrow, S.J. Pocock, C. Poole, J.J. Schlesselman, M. Egger, Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 4, e297 (2007). https://doi.org/10.1371/journal.pmed.0040297
S. Sanderson, I.D. Tatt, J.P.T. Higgins, Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int. J. Epidemiol. 36, 666–676 (2007). https://doi.org/10.1093/ije/dym018
R. DerSimonian, N. Laird, Meta-analysis in clinical trials. Control. Clin. Trials 7, 177–188 (1986)
J.P. Higgins, Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration (2011). www.training.cochrane.org/handbook
J.A. Sterne, M. Egger, Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J. Clin. Epidemiol. 54, 1046–1055 (2001). https://doi.org/10.1016/s0895-4356(01)00377-8
G.Schwarzer, Meta: an R package for meta-analysis. R News 7, 40–45 (2007)
V. Bhole, M. de Vera, M.M. Rahman, E. Krishnan, H. Choi, Epidemiology of gout in women: fifty-two-year followup of a prospective cohort. Arthritis Rheum. 62, 1069–1076 (2010). https://doi.org/10.1002/art.27338
R.A. Hayward, T. Rathod, E. Roddy, S. Muller, S.L. Hider, C.D. Mallen, The association of gout with socioeconomic status in primary care: a cross-sectional observational study. Rheumatology 52, 2004–2008 (2013). https://doi.org/10.1093/rheumatology/ket262
H. Liu, X.M. Zhang, Y.L. Wang, B.C. Liu, Prevalence of hyperuricemia among Chinese adults: a national cross-sectional survey using multistage, stratified sampling. J. Nephrol. 27, 653–658 (2014). https://doi.org/10.1007/s40620-014-0082-z
P. Wandell, A.C. Carlsson, X. Li, D. Gasevic, J. Arnlov, M.J. Holzmann, J. Sundquist, K. Sundquist, Gout in immigrant groups: a cohort study in Sweden. Clin. Rheumatol. 36, 1091–1102 (2017). https://doi.org/10.1007/s10067-016-3525-1
W.G. Fang, X.M. Huang, Y. Wang, W.G. Zhu, Z.X. Bie, J.L. Chen, X.J. Zeng, A cross-sectional study of hyperuricemia in state-employees in Beijing: prevalence and risk factors.Natl Med. J. China 86, 1764–1768 (2006)
M. Uetani, Y. Suwazono, E. Kobayashi, T. Inaba, M. Oishi, K. Nogawa, A longitudinal study of the influence of shift work on serum uric acid levels in workers at a telecommunications company. Occup. Med. 56, 83–88 (2006). https://doi.org/10.1093/occmed/kqi178
L. Winters-Miner, Personalized Medicine. In: L. Winters-Miner, P.S. Bolding, et al. (eds), Practical Predictive Analytics and Decisioning Systems for Medicine, pp 176–204. Academic Press (2015)
M.M. Ibrahim, A. Damasceno, Hypertension in developing countries. Lancet 380, 611–619 (2012). https://doi.org/10.1016/S0140-6736(12)60861-7
J. Schmidhuber, P. Shetty, The nutrition transition to 2030. Why developing countries are likely to bear the major burden. Food Econ. Acta Agric. Scand. Sect. C 2, 150–166 (2005). https://doi.org/10.1080/16507540500534812
T. Bärnighausen, D.E. Bloom, S. Humair, 3—Global health governance and tropical diseases. Presented at the (2014)
S.C. Larsson, S. Burgess, K. Michaëlsson, Genetic association between adiposity and gout: a Mendelian randomization study. Rheumatology 57, 2145–2148 (2018). https://doi.org/10.1093/rheumatology/key229
S.C. Larsson, M. Carlström, Coffee consumption and gout: a Mendelian randomisation study. Ann. Rheum. Dis., 4–6 (2018). https://doi.org/10.1136/annrheumdis-2018-213055
T.J. Major, N. Dalbeth, E.A. Stahl, T.R. Merriman, An update on the genetics of hyperuricaemia and gout. Nat. Rev. Rheumatol. 14, 351–353 (2018). https://doi.org/10.1038/s41584-018-0004-x
G.D. Smith, M. Egger, Meta-analyses of observational data should be done with due care. BMJ 318, 56 (1999)
I. Shrier, J.-F. Boivin, R.J. Steele, R.W. Platt, A. Furlan, R. Kakuma, J. Brophy, M. Rossignol, Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? Acritical examination of underlying principles. Am. J. Epidemiol. 166, 1203–1209 (2007). https://doi.org/10.1093/aje/kwm189
B. Galobardes, M. Shaw, D.A. Lawlor, J.W. Lynch, G. Davey Smith, Indicators of socioeconomic position (part 1). J. Epidemiol. Community Health 60, 7–12 (2006). https://doi.org/10.1136/jech.2004.023531
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pan, Z., Huang, M., Fang, M. et al. Socioeconomic differences in hyperuricemia and gout: a systematic review and meta-analysis. Endocrine 69, 286–293 (2020). https://doi.org/10.1007/s12020-020-02281-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02281-w