Abstract
Purpose
Headache is a common presenting feature of patients with pituitary adenomas and other tumors of the sellar region. However, at present, it still is unclear whether the headache is actually caused by the tumor. To explore whether there is a relation, we examined in detail the headache types, their relationship to the underlying pathology, and if the headache responded to neurosurgery in a prospective study design.
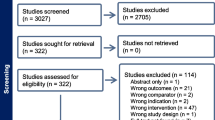
Methods
One hundred twelve patients with tumors of the sellar region scheduled for neurosurgery in a single center were analyzed for presence and quality of headache before surgery and at least 3 months after surgery. Patients received headache and depression self-rating inventories, presented on a handheld computer (PainDetect®). Clinical variables thought to impact on headache were analyzed in conjunction with the inventories.
Results
Fifty-nine (53%) patients reported headache in the 3 months prior to neurosurgery, 49 (44%) had headache at the time of filling in the questionnaires. The four patients with pituitary apoplexy described thunderclap headache. In the other patients diverse headache types were encountered, most frequently migraine. Untreated gonadotroph deficiency was significantly associated with absence of headache, while none of the other clinical and morphological variables related to headache. Presence of headache and disability due to headache were not significantly reduced after surgery.
Conclusion
Apart from pituitary apoplexy we detected no specific headache type in our patient group and no significant improvement of headache after neurosurgery. Headache alone constitutes neither a valid diagnostic marker for the presence of tumors of the sellar region nor a sufficient indication for tumor removal.



Similar content being viewed by others
References
A. Jahangiri, J.R. Wagner, A.T. Chin, S.W. Han, M.T. Tran, L.M. Miller, M.W. Tom, R. Chen, S. Kunwar, L. Blevins, M.K. Aghi, Incidence of headache as a presenting complaint in over 1000 patients with sellar lesions and factors predicting postoperative improvement. Clin. Neurol. Neurosurg. 132, 16–20 (2015). doi:10.1016/j.clineuro.2015.02.006
M.J. Levy, M.S. Matharu, K. Meeran, M. Powell, P.J. Goadsby, The clinical characteristics of headache in patients with pituitary tumours. Brain 128(Pt 8), 1921–1930 (2005). doi:10.1093/brain/awh525
B. Stoffel-Wagner, P. Stoger, D. Klingmuller, Initial symptoms and anamnestic time in 517 patients with pituitary adenoma. Dtsch. Med. Wochenschr. 122(8), 213–219 (1997). doi:10.1055/s-2008-1047599
B.M. Arafah, D. Prunty, J. Ybarra, M.L. Hlavin, W.R. Selman, The dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas. J. Clin. Endocrinol. Metab. 85(5), 1789–1793 (2000). doi:10.1210/jcem.85.5.6611
J.A. Gondim, J.P. de Almeida, L.A. de Albuquerque, M. Schops, E. Gomes, T. Ferraz, Headache associated with pituitary tumors. J. Headache Pain 10(1), 15–20 (2009). doi:10.1007/s10194-008-0084-0
M.J. Levy, The association of pituitary tumors and headache. Curr. Neurol. Neurosci. Rep. 11(2), 164–170 (2011). doi:10.1007/s11910-010-0166-7
A. Pereira-Neto, A.M. Borba, P.A. Mello, L.A. Naves, A.S. Araujo Jr, L.A. Casulari, Mean intrasellar pressure, visual field, headache intensity and quality of life of patients with pituitary adenoma. Arq. Neuropsiquiatr. 68(3), 350–354 (2010)
N. Suwanwela, K. Phanthumchinda, S. Kaoropthum, Headache in brain tumor: a cross-sectional study. Headache 34(7), 435–438 (1994)
The International Classification of Headache Disorders: 2nd edition, Headache Classification Subcommittee of the International Headache Society. Cephalalgia 24(Suppl 1), 9–160 (2004)
S. Nelson, L.P. Taylor, Headaches in brain tumor patients: primary or secondary? Headache 54(4), 776–785 (2014). doi:10.1111/head.12326
Z. Morris, W.N. Whiteley, W.T. Longstreth Jr., F. Weber, Y.C. Lee, Y. Tsushima, H. Alphs, S.C. Ladd, C. Warlow, J.M. Wardlaw, R. Al-Shahi Salman, Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. Br. Med. J. 339, b3016 (2009). doi:10.1136/bmj.b3016
C.J. Schankin, A.K. Reifferscheid, M. Krumbholz, J. Linn, W. Rachinger, S. Langer, P. Sostak, T. Arzberger, H. Kretzschmar, A. Straube, Headache in patients with pituitary adenoma: clinical and paraclinical findings. Cephalalgia 32(16), 1198–1207 (2012). doi:10.1177/0333102412462639
Department of Health and Human Services, F.D.A., in International Conference on Harmonisation; Good Clinical Practice: Consolidated Guideline, Vol. 62, pp. 1–53. Federal Register, Brussels, Belgium (1997)
World Medical Association, World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. J. Am. Med. Assoc. 310(20), 2191–2194 (2013). doi:10.1001/jama.2013.281053
U. Junker, R. Freynhagen, K. Langler, U. Gockel, U. Schmidt, T.R. Tolle, R. Baron, T. Kohlmann, Paper versus electronic rating scales for pain assessment: a prospective, randomised, cross-over validation study with 200 chronic pain patients. Curr. Med. Res. Opin. 24(6), 1797–1806 (2008). doi:10.1185/03007990802121059
M. Pompili, D. Di Cosimo, M. Innamorati, D. Lester, R. Tatarelli, P. Martelletti, Psychiatric comorbidity in patients with chronic daily headache and migraine: a selective overview including personality traits and suicide risk. J. Headache Pain 10(4), 283–290 (2009). doi:10.1007/s10194-009-0134-2
G. Fritsche, M. Hueppe, M. Kukava, A. Dzagnidze, M. Schuerks, M.S. Yoon, H.C. Diener, Z. Katsarava, Validation of a German language questionnaire for screening for migraine, tension-type headache, and trigeminal autonomic cephalgias. Headache 47(4), 546–551 (2007). doi:10.1111/j.1526-4610.2007.00758.x
W.F. Stewart, R.B. Lipton, A.J. Dowson, J. Sawyer, Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology 56(6 Suppl 1), S20–S28 (2001)
K. Kroenke, R.L. Spitzer, J.B. Williams, The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16(9), 606–613 (2001)
A. Victor, A. Elsasser, G. Hommel, M. Blettner, Judging a plethora of p-values: how to contend with the problem of multiple testing—part 10 of a series on evaluation of scientific publications. Dtsch. Arztebl. Int. 107(4), 50–56 (2010). doi:10.3238/arztebl.2009.0050
B. Yu, N. Ji, Y. Ma, B. Yang, P. Kang, F. Luo: Clinical characteristics and risk factors for headache associated with non-functioning pituitary adenomas. Cephalalgia (2016). doi:10.1177/0333102416648347
M.J. Levy, H.R. Jager, M. Powell, M.S. Matharu, K. Meeran, P.J. Goadsby, Pituitary volume and headache: size is not everything. Arch. Neurol. 61(5), 721–725 (2004). doi:10.1001/archneur.61.5.721
C. Dimopoulou, A.P. Athanasoulia, E. Hanisch, S. Held, T. Sprenger, T.R. Toelle, J. Roemmler-Zehrer, J. Schopohl, G.K. Stalla, C. Sievers, Clinical characteristics of pain in patients with pituitary adenomas. Eur. J. Endocrinol. 171(5), 581–591 (2014). doi:10.1530/eje-14-0375
B. Harbeck, C.S. Haas, S. Suefke, P. Kropp, H. Moenig, Headache and depression in patients with hypothalamic-pituitary disorders-etiology and risk factors. Exp. Clin. Endocrinol. Diabetes 123(9), 571–574 (2015). doi:10.1055/s-0035-1559630
N.C. Chai, B.L. Peterlin, A.H. Calhoun, Migraine and estrogen. Curr. Opin. Neurol. 27(3), 315–324 (2014). doi:10.1097/wco.0000000000000091
T. Abe, K. Matsumoto, J. Kuwazawa, I. Toyoda, K. Sasaki, Headache associated with pituitary adenomas. Headache 38(10), 782–786 (1998)
M.H. Almalki, A.D. Chesover, M.D. Johnson, G.E. Wilkins, J.A. Maguire, E. Ur, Characterization of management and outcomes of patients with acromegaly in Vancouver over 30 years. Clin. Invest. Med. 35(1), E27–E33 (2012)
M. Mercado, A.L. Espinosa de los Monteros, E. Sosa, S. Cheng, V. Mendoza, I. Hernandez, C. Sandoval, G. Guinto, M. Molina, Clinical-biochemical correlations in acromegaly at diagnosis and the real prevalence of biochemically discordant disease. Horm. Res. 62(6), 293–299 (2004). doi:10.1159/000082032
D. Borsook, N. Erpelding, A. Lebel, C. Linnman, R. Veggeberg, P.E. Grant, C. Buettner, L. Becerra, R. Burstein, Sex and the migraine brain. Neurobiol. Dis. 68, 200–214 (2014). doi:10.1016/j.nbd.2014.03.008
A. May, L.H. Schulte, Chronic migraine: risk factors, mechanisms and treatment. Nat. Rev. Neurol. 12(8), 455–464 (2016). doi:10.1038/nrneurol.2016.93
M.T. Minen, O. Begasse De Dhaem, A. Kroon Van Diest, S. Powers, T.J. Schwedt, R. Lipton, D. Silbersweig, Migraine and its psychiatric comorbidities. J. Neurol. Neurosurg. Psychiatry 87(7), 741–749 (2016). doi:10.1136/jnnp-2015-312233
R.W. Evans, M.J. Levy, Expert opinion: headache and pituitary tumors. Headache 48(2), 280–283 (2008). doi:10.1111/j.1526-4610.2007.01020.x
Acknowledgements
Part of the data was collected for the doctoral theses of Renata Weber Carneiro and Sonja Siegel. The study was performed when the first, second, fifth, and last author worked full-time at the Department of Neurosurgery, Erlangen. The study was partially funded by an independent investigator-initiated grant from Pfizer Pharma GmbH.
Author contributions
S.S., R.W.C., M.B., G.B., and I. K.-A. designed the study. R.W.C., S.S., and A.G. collected the data. S.S., B.K., and I. K.-A. conducted the statistical data analysis. All authors critically discussed the results of the study and participated in the drafting of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
With respect to the performed research, the authors report no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Siegel, S., Weber Carneiro, R., Buchfelder, M. et al. Presence of headache and headache types in patients with tumors of the sellar region—can surgery solve the problem? Results of a prospective single center study. Endocrine 56, 325–335 (2017). https://doi.org/10.1007/s12020-017-1266-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1266-9