Abstract
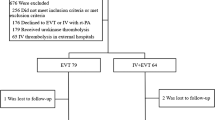
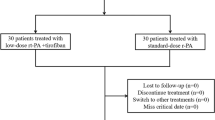
The objective of this study was to evaluate the efficacy and safety of intra-arterial thrombolysis in treating acute cerebral infarction and further discuss the indications of acute cerebral infarction treatment, in order to enhance the therapeutic effects of arterial thrombolysis. The data of 164 patients with acute cerebral infarction who accepted intra-arterial thrombolysis treatment by using rt-PA or reteplase between 2009 and 2014 at the Department of Neurology of our hospital, were collected, including patients’ medical history, characteristics of the onset procedure, intervals between onset and intra-arterial thrombolysis, bleeding or death, and the changing process of patient’s main neurologic function after the treatment. The neurological functions including muscle strength, speech, and level of consciousness were chosen for evaluation. Through a review of cerebral angiography, we collected the digital subtraction angiography (DSA) morphological changes of blood vessels before and after arterial thrombolysis to evaluate whether those blood vessels had been reperfused. Thereafter, we analyzed and statistically processed above-mentioned data. The mean time of arterial thrombolysis was 5.7 h. DSA results were as follows: 22 patients had complete internal carotid artery (ICA) occlusion; 49 patients middle cerebral artery’s (MCA’s) Ml or M2 segment occlusion; 6 patients anterior cerebral artery (ACA) occlusion; 58 patients reperfusion after thrombolysis, and the recanalization rate was 76 %. Based on vertebral–basilar artery (VBA) system, 18 patients had complete occlusion, 11 patients had reperfusion after thrombolysis, and the recanalization rate was 61 %. A total of 63 patients had severe stenosis, and they had significantly improved after thrombolysis. The clinical symptoms of patients were improved: 79 out of 164 patients with paralysis had partially recovered their limb muscle strength after operation, while 33 patients had completely recovered, and there was no recovery at all of the muscle strength in 4 patients after operation. In total, 59 out of 63 patients with aphasia had improved their language function, while 19 patients with disturbance of consciousness turned for the better after arterial thrombolysis. Only one patient experienced the cerebral hemorrhage, and 14 cases had gingival bleeding, oral mucosa bleeding, and urethrorrhagia. The overall effective rates of intra-arterial thrombolysis in treating the acute cerebral infarction by reteplase had no significant differences compared to those by rt-PA, and there were no hemorrhagic complications. It is safe and effective if the arterial thrombolysis using reteplase is performed within a few hours after acute cerebral infarction onset because reteplase has a higher clinical efficacy and lower hemorrhagic transformation, which suggests that it may become a new feasible option for clinical arterial thrombolysis.




Similar content being viewed by others
References
Smith, W. S., Sung, G., Saver, J., Budzik, R., Duckwiler, G., Liebeskind, D. S., et al. (2008). Mechanical thrombectomy for acute ischemic stroke: Final results of the multi merci trial. Stroke, 39, 1205–1212.
Tissue plasminogen activator for acute ischemic stroke. (1995). The national institute of neurological disorders and stroke rt-pa stroke study group. The New England journal of medicine., 333, 1581–1587.
Hacke, W., Brott, T., Caplan, L., Meier, D., Fieschi, C., von Kummer, R., et al. (1999). Thrombolysis in acute ischemic stroke: Controlled trials and clinical experience. Neurology, 53, S3–S14.
Hacke, W., Kaste, M., Fieschi, C., von Kummer, R., Davalos, A., Meier, D., et al. (1998). Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second european-australasian acute stroke study investigators. Lancet, 352, 1245–1251.
Mattle, H. P., Arnold, M., Georgiadis, D., Baumann, C., Nedeltchev, K., Benninger, D., et al. (2008). Comparison of intraarterial and intravenous thrombolysis for ischemic stroke with hyperdense middle cerebral artery sign. Stroke, 39, 379–383.
Rha, J. H., & Saver, J. L. (2007). The impact of recanalization on ischemic stroke outcome: A meta-analysis. Stroke, 38, 967–973.
Lindsberg, P. J., & Mattle, H. P. (2006). Therapy of basilar artery occlusion: A systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke, 37, 922–928.
Misra, V., El Khoury, R., Arora, R., Chen, P. R., Suzuki, S., Harun, N., et al. (2011). Safety of high doses of urokinase and reteplase for acute ischemic stroke. American Journal of Neuroradiology, 32, 998–1001.
Ciccone, A., Valvassori, L., & Nichelatti, M. (2011). Synthesis expansion: Design of a nonprofit, pragmatic, randomized, controlled trial on the best fast-track endovascular treatment vs. Standard intravenous alteplase for acute ischemic stroke. International journal of stroke, 6, 259–265.
Ciccone, A. (2003). Consent to thrombolysis in acute ischaemic stroke: From trial to practice. Lancet Neurology, 2, 375–378.
Furlan, A., Higashida, R., Wechsler, L., Gent, M., Rowley, H., Kase, C., et al. (1999). Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: A randomized controlled trial. Prolyse in acute cerebral thromboembolism. The Journal of the American Medical Association, 282, 2003–2011.
Mori, E., Tabuchi, M., Yoshida, T., & Yamadori, A. (1988). Intracarotid urokinase with thromboembolic occlusion of the middle cerebral artery. Stroke, 19, 802–812.
del Zoppo, G. J., Higashida, R. T., Furlan, A. J., Pessin, M. S., Rowley, H. A., & Gent, M. (1998). Proact: A phase ii randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. Proact investigators. Prolyse in acute cerebral thromboembolism. Stroke, 29, 4–11.
Lisboa, R. C., Jovanovic, B. D., & Alberts, M. J. (2002). Analysis of the safety and efficacy of intra-arterial thrombolytic therapy in ischemic stroke. Stroke, 33, 2866–2871.
Qureshi, A. I., Siddiqui, A. M., Suri, M. F., Kim, S. H., Ali, Z., Yahia, A. M., et al. (2002). Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: A prospective study. Neurosurgery, 51, 1319–1327. discussion 1327–1319.
Soares, B. P., Chien, J. D., & Wintermark, M. (2009). Mr and ct monitoring of recanalization, reperfusion, and penumbra salvage: Everything that recanalizes does not necessarily reperfuse! Stroke, 40, S24–S27.
Deitcher, S. R., & Jaff, M. R. (2002). Pharmacologic and clinical characteristics of thrombolytic agents. Reviews in cardiovascular medicine, 3(Suppl 2), S25–S33.
Qureshi, A. I., Ali, Z., Suri, M. F., Kim, S. H., Shatla, A. A., Ringer, A. J., et al. (2001). Intra-arterial third-generation recombinant tissue plasminogen activator (reteplase) for acute ischemic stroke. Neurosurgery, 49, 41–48. discussion 48–50.
Sugg, R. M., Noser, E. A., Shaltoni, H. M., Gonzales, N. R., Campbell, M. S., Weir, R., et al. (2006). Intra-arterial reteplase compared to urokinase for thrombolytic recanalization in acute ischemic stroke. American Journal of Neuroradiology, 27, 769–773.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shen, B., Liu, Q., Gu, Y. et al. Efficacy and Safety Evaluation on Arterial Thrombolysis in Treating Acute Cerebral Infarction. Cell Biochem Biophys 73, 297–304 (2015). https://doi.org/10.1007/s12013-015-0577-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0577-9