Abstract
Objectives
To investigate whether intravenous thrombolysis (IVT) with alteplase (a recombinant tissue plasminogen activator, rt-PA) before endovascular treatment (EVT) is beneficial for acute ischemic stroke (AIS) patients in different periods.
Methods
This study enrolled a total of 140 patients hospitalized between 2019 and 2022 with AIS from large vessel occlusion (LVO) in the anterior circulation. Those patients were divided into the EVT alone group and IVT + EVT group, in which EVT was preceded by intravenous rt-PA. According to the time from onset to femoral artery puncture, the above two groups were divided into the following subgroups: < 4.5 h, between 4.5 and 6 h, between 6 and 8 h, and between 8 and 10 h. There were 78 patients in the EVT alone group and 62 patients in the IVT + EVT group.
Results
There was no statistically significant difference in functional independence, recanalization rate, favorable outcome rate, or mortality between the EVT and IVT + EVT groups (P > 0.05). After adjusting for confounding factors, a lower incidence of intracerebral hemorrhage was observed in the EVT group (P < 0.05). A comparison of time-dependent efficacy between the two groups showed that within 6–8 h, there were statistically significant differences between admission and postoperation in the National Institutes of Health Stroke Scale scores at 24 h (P = 0.01) or 7 days (P = 0.02).
Conclusions
Although there was no difference in clinical efficacy and safety between the abovementioned two groups, treatment with IVT + EVT could increase the risk of bleeding compared to EVT. Moreover, in the 6–8 h subgroup, the efficacy of EVT alone was better than that of IVT + EVT.
Similar content being viewed by others
Introduction
Stroke is the leading cause of death and disability among adults in China, with high rates of incidence, disability, mortality, and recurrence. The incidence of cerebrovascular events in China is predicted to be approximately 50% higher in 2030 than in 2010 [1, 2]. AIS is the most common type of stroke, accounting for approximately 80% of all strokes [3]. The key to treating AIS is to unclog the obstructed arteries as early as possible [4]. Timely IVT with rt-PA can recanalize the occluded vessels, thereby salvaging the ischemic semidark zone area and ultimately reducing the rates of death and disability caused by ischemic stroke. However, the limited lysis effect of IVT on larger, proximally located thrombi has been reported; in particular, partial lysis may fragment the target thrombus or cause it to migrate distally [5, 6]. Therefore, IVT may also increase the risk of cerebral hemorrhage. To overcome the disadvantage of IVT, more attention has been paid to EVT within the same time frame, which has become the current mainstream treatment option for AIS.
Based on national and international guidelines [7, 8], IVT should be administered before endovascular intervention for treating AIS patients who are eligible for both IVT and EVT. In addition, several randomized clinical trials have consistently shown that patients with LVO in the anterior circulation may benefit from EVT after IVT treatment [9,10,11]. However, a comparison of clinical profiles, including procedural, clinical outcomes, and safety, between EVT alone and IVT+EVT has not shown a significant difference between those two therapies, even after adjusting for confounding factors [12]. Recently, a published randomized clinical trial (DIRECT-MT) of EVT with or without IVT in AIS patients revealed that EVT alone was not inferior to EVT after IVT [13]. In the DEVT trial, a similar effect was observed [14]. However, there was a wide range of noninferiority in that trial, which did not reach clinical consensus. In addition, all the enrolled subjects were endovascularly treated within 4.5 h; therefore, it is not possible to state the superiority or inferiority of the two treatment options beyond 4.5 h. Thus, it is still debatable whether EVT is beneficial for the prognosis of AIS patients with LVO compared with IVT+EVT in different periods.
To clarify whether IVT with an injection of rt-PA before bolus retrieval in different periods is beneficial to patient prognosis, a comparison of efficacy between the subgroups of EVT alone and IVT+EVT in different periods was performed. The results of this study may provide a basis for the preoperative evaluation and selection of treatment options in different periods.
Methods
Trial design and oversight
This was a multicenter retrospective study that mainly compared the effectiveness (clinical results, recanalization rate) and safety (intracranial hemorrhage, mortality) between EVT and IVT+EVT in the different periods of treatment time. The protocol was approved by the institutional review board.
Patient selection
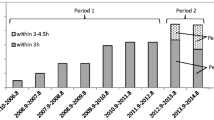
We collected 140 AIS patients with LVO in the anterior circulation from three local advanced stroke centers between March 2019 and March 2022 (Fig. 1). The inclusion criteria of this study were as follows: (1) confirmed diagnosis of AIS; (2) age ranging between 18 and 80; (3) baseline National Institutes of Health Stroke Scale (NIHSS) score ≥ 4 or with isolated aphasia or hemianopia; (4) Alberta Stroke Program Early CT Score (ASPECTS) ≥ 6; (5) pre-onset Modified Rankin Scale (MRS) score ≤ 1; (6) vascular occlusion associated with neurological deficit; and (7) duration of symptoms less than 10 h [15]. The exclusion criteria were as follows: (1) age > 80 years; (2) incomplete data; (3) lost cases; (4) posterior circulation occlusion; and (5) received outside hospital thrombolysis. All patients in this study had intracranial occlusion of the internal carotid artery (ICA), middle cerebral artery M1 or M2, or both, all of which were confirmed by digital subtraction angiography. The IVT procedure in our study was performed according to international and institutional guidelines [4, 16]. In the IVT+EVT group, patients received IVT at a dose of 0.9 mg/kg body weight, before which rt-PA was given within 4.5 h after the onset of symptoms, according to the patient’s condition and other factors. However, the final treatment decision was made by an interdisciplinary team of neurologists and neuroradiologists based on the basic situation of the case. Therefore, in some cases, especially in the case of LVO suspected to have a large thrombus burden, EVT directly could be the first choice of the team, rather than IVT+EVT. The EVT procedure included the following aspects: stent thrombectomy, thrombus extraction, stent forming, balloon forming, and mechanical removal of blood clots with or without local use of the thrombolytic agent. The corresponding scores of the cases were calculated by analyses of the computed tomography (CT) image data. In this study, we used Neusoft Brain Clinical Assistant Ration Evaluate (NeuBrainCARE, China) to avoid the large infarct area of the included cases. NeuBrainCARE is a brain disease analysis software that focuses on quickly providing evidence of thrombolysis and EVT via the detection of blockages in major brain blood vessels [17], which can automatically partition the brain and calculate the ASPECTS on the CT sequence, thereby finding the cases with ASPECTS ≥ 6 to ensure the reliability of our study results (Fig. 2). When patients were discharged, they were asked to conduct a follow-up (90 days) in the outpatient department of the hospital to re-check the MRS score. For patients who did not visit the outpatient department in time after 90 days, we evaluated their MRS score through telephone follow-up. Patients transferred after thrombolysis in external hospitals were not included in our study.
Study sites and interventionists
This study was performed at three advanced stroke centers in Shanxi Province. In those stroke centers, which are equipped with trained neurointerventional doctors, the number of hospitalized patients with AIS is more than 600 every year, and the number of cases with EVT and IVT+EVT is more than 200 each year.
Evaluation of patient outcomes
The primary outcome for evaluation was the MRS score at 90 days after surgery based on a 7-level global disability measurement scale with scores ranging from 0 (asymptomatic) to 6 (death), including categories of good results (0–2) and bad results (3–6), according to the analysis of data collected from telephone follow-up or outpatient reexamination. Secondary outcomes included functional independence 90 days after surgery (MRS score ≤ 2), such as changes in the NIHSS score 24 h and 7 days after surgery, as well as vascular recanalization, which is defined by the score of the modified thrombolysis in cerebral infarction (mTICI) ranging from 0 to 3; mTICI ≥ 2b is considered to be successful recanalization. The safety outcome was also considered, which included the 90-day postoperative mortality and intracranial hemorrhage rate evaluated using the European Cooperative Acute Stroke Study-II standard [18, 19], in which parenchymal hematoma PH-1 or PH-2 was defined as significant bleeding.
Statistical analyses
In this study, SPSS Statistics 22.0 software was used for data processing and data analysis. The chi-square test or Fisher’s exact probability method was used for comparisons among groups of categorical variables. The t test was used to compare the difference between groups for normally distributed measures, whereas the Mann–Whitney U test was used to compare between groups for non-normally distributed measures. At 90 days after treatment, the MRS scores in different subgroups were compared by ordered logistic regression analysis. The parameters in the multivariate model, including age, baseline NIHSS scores, ASPECTS, onset-to-revascularization time, and onset-to-puncture time, were also included for data analysis. We adjusted the results of the data analysis in this study according to theoretical knowledge, known relevant results, and empirical knowledge (baseline imbalance). Secondary outcomes were evaluated using logistic regression. P < 0.05 was considered statistically significant.
Results
A total of 140 patients were enrolled in our study, including 78 who received EVT alone and 62 who received IVT+EVT. As shown in Table 1, the baseline characteristics of the patients in those two groups were similar, such as age, hypertension, diabetes, atrial fibrillation, current smoking status, ischemic stroke or transient ischemic attack history, and the ASPECTS. The mean age of the patients in the EVT alone group was 64 years, of whom 37 patients (52.4%) were male, and their median ASPECTS was 8 points (interquartile range [IQR] 6–10). The mean age of patients in the IVT+EVT group was 65 years, and similarly, 45 patients (74.5%) were male, and their median ASPECTS was also 8 points (IQR 6–10). The median time from onset to femoral artery puncture was 396 min (IQR 24–600) and from stroke onset to revascularization was 469 min (IQR 67–1140) in the EVT group, whereas in the IVT+EVT group, it was 271 min (IQR 43–600) and 380 min (IQR 140–731), respectively.
Primary outcome
The evaluation of the primary outcome revealed that 49 cases (62.8%) in the EVT group had an MRS score of 0–2 at 90 days after the operation, whereas 35 cases (56.5%) in the IVT+EVT group had a similar MRS score (Fig. 3). Ninety days after the operation, the adjusted common odds ratio (OR) of the MRS score was 0.81 (95% confidence interval [CI] –0.86 to 0.43; P = 0.52) (Table 2). Therefore, there was no significant difference in MRS score between the EVT and IVT + EVT groups.
Scores on the MRS at 90 days in the intention-to-treat population. As shown in the picture, the percentages of patients in the endovascular therapy group and alteplase-only group with scores from 0 to 6, according to the MRS as follows: 0, no symptoms; 1. no clinically significant disability; 2. slight disability (able to handle own affairs without assistance but unable to carry out all previous activities); 3. moderate disability requiring some help (e.g., with shopping, cleaning, and finances but able to walk unassisted); 4. moderately severe disability (unable to attend to bodily needs without assistance and unable to walk unassisted); 5. severe disability (requiring constant nursing care and attention); and 6. death. Patients with a score of 0, 1, or 2 are considered to be independent in daily function
Secondary outcomes
The adjusted common OR for functional independence (MRS score ≤ 2) at 90 days after the operation was 1.72 (95% CI 0.78 to 3.78; P = 0.18). The NIHSS score was not significantly different between admission and postoperation at 24 h (P = 0.12) or 7 days (P = 0.15). The adjusted common OR of the postoperative recanalization rate was 0.59 (95% CI 0.23 to 1.55; P = 0.29). Successful revascularization was achieved in 83.3% of patients in the EVT alone group and in 79.0% of patients in the IVT+EVT group (Table 3). The abovementioned results revealed that there was no statistically significant difference in secondary outcomes between the two treatment groups. In the 6–8 h subgroup, the NIHSS score was significantly different between admission and postoperation at 24 h (P = 0.01) or 7 days (P = 0.02). The analyses of other subgroups are shown in Table 4.
Safety outcomes
During the 90-day follow-up, the adjusted common OR of postoperative mortality in the two treatment groups was 1.56 (95% CI 0.58 to 4.21; P = 0.38). The adjusted common OR of the postoperative intracranial hemorrhage rate in the two treatment groups was 8.21 (95% CI 1.28 to 52.82; P = 0.03), indicating that there was no significant difference in mortality between the two treatment groups. Moreover, IVT+EVT might increase the risk of intracranial hemorrhage. In the 6–8 h subgroup, the mortality (P = 0.02) was significantly different between groups. The analyses of other subgroups are shown in Table 4.
Discussion
In our study, the comparison of clinical outcomes showed that there was no difference in recanalization rate, mortality, or long-term functional outcomes in stroke patients who received rt-PA thrombolysis before EVT compared to those in patients who received EVT alone, except for the increased risk of intracranial hemorrhage. However, in the 6–8 h subgroup, the effect of EVT alone was not inferior to that of IVT+EVT, whereas the DEVT study showed no significant difference between the two groups regarding mortality and incidence of spontaneous cerebral hemorrhage [14], which may be due to the exclusion of patients with M2 segment occlusion in DEVT. Tsivgoulisg et al. [20] reported that the efficacy of EVT in acute LVO does not depend on IVT pretreatment, according to a systematic review and meta-analysis of all available randomized controlled trials. A meta-analysis by Chen et al. [21]. suggested that in patients with anterior circulation AIS within 4.5 h after onset, EVT was not inferior to IVT therapy in combination with intravascular EVT. Weber [22] and others believe that in patients with AIS treated with EVT, the use of IVT is not an independent predictor of a good prognosis, because there is no difference in the incidence of complications whether IVT is used. However, the study included cases with pre-stroke MRS ≥ 3 and with severe comorbidities, which may have impacted the reliability of the results. A retrospective study [23] showed that EVT combined with IVT within 4.5–9 h after onset might be safe in patients with anterior circulation artery occlusion due to the lack of a significantly increased risk of intracranial hemorrhage. Our results are not consistent with the abovementioned study. In our study, the subjects in the IV+EVT group were intravenously thrombolyzed within 4.5 h, suggesting an increased risk of intracranial hemorrhage when intravenous thrombolysis was given before endovascular treatment. Based on clinical outcomes, such as the improvement of neurological function 24 h and 7 days after the operation as well as the mortality (90 days) after the operation, the efficacy of EVT in the 6–8 h subgroup was better than that in the same subgroup of IVT+EVT. However, there was no significant difference between those two treatments in the other subgroups.
However, due to the relatively small sample size in this study, especially in the 8–10 h subgroup, the reliability of the data might be reduced. Therefore, it is still unclear whether there will be differences in the 8–10 h subgroup with an increase in sample size, even including the differences between the two treatments after 6 h, which needs a larger sample size to confirm. Using current evidence, it is recommended that EVT be directly performed within 10 h after the onset of the disease, but IVT is not necessary. However, within this time window, the effectiveness of the treatment of IVT+EVT or EVT needs to be verified in larger randomized controlled trials.
Park [24] and others reported a prospective multicenter stroke registration database in Korea that included 639 AIS patients, of whom 458 received IVT before EVT. That report showed that giving IVT before EVT within 8 h after the onset of AIS could improve both the survival rate and recanalization rate without increasing the risk of symptomatic hemorrhage, leading to a decrease in disability symptoms 3 months after treatment. That report revealed that IVT is beneficial before endovascular treatment, which is inconsistent with our results. It is notable that the subjects enrolled in the abovementioned study also included those with posterior circulation AIS, which may be the reason why their findings are not consistent with our results.
Moreover, in some AIS patients with LVO, IVT before EVT may have several disadvantages, such as poor migration of embolus and an increase in the following aspects: ischemic area, the risk of intracranial hemorrhage, medical consumption, and the burden of patients. Administration of IVT before EVT may also delay the duration time from onset to femoral artery puncture, especially in the case of AIS patients with LVO who must be transferred to the comprehensive stroke center for further treatment after receiving intravenous injection in a local stroke center, where there are no EVT conditions [25]. Among the cases we collected, 65 patients were excluded due to a delayed time from onset to femoral artery puncture, because those patients were transferred to our hospital after receiving IVT in a lower level hospital without EVT conditions.
Despite its shortcomings, IVT can promote either intravascular reperfusion or the dissolution of microemboli lodged in the downstream precapillary vasculature and can also improve distal perfusion [26, 27]. The benefit of IVT therapy should not be ignored. It is important for clinicians to perform IVT in AIS patients who have no contraindications to thrombolysis within the time window.
Accordingly, we conducted EVT treatment in patients with acute anterior circulation ischemic stroke within 10 h from symptom onset to femoral artery puncture. The EVT was proven safe compared to the IVT+EVT, especially for patients with acute anterior circulation ischemic stroke within 6–8 h from symptom onset to femoral artery puncture. Thus, EVT can not only promote the recovery of neurological function but can also decrease the risk of intracranial hemorrhage.
This study had some limitations. First, this retrospective study was prone to selection bias. Second, we excluded some cases with contraindications to thrombolysis from the EVT group, resulting in a small sample size, which may have affected the reliability of our results. In previously reported studies, a paired analysis study based on two large registrations (no thrombolytic contraindications in the EVT group) showed that except for the high mortality of patients with ICA occlusion, there was no difference in the outcome of IVT patients with LVO anterior circulation stroke when EVT alone and IVT+EVT for those patients were compared [28]. That study could support the reliability of our results to some extent. Finally, compared to many Western countries, China’s prehospital triage system is more complex, where patients usually go to the hospital directly by private transportation; in such a situation, the stroke treatment team is usually mobilized only when the patient is admitted to the hospital, rather than before the patient arrives [13]. Moreover, most of the patients originally came from remote areas, and their families and patients themselves had limited knowledge about stroke. Therefore, after the onset of stroke, they cannot go to the hospital immediately. Even if they arrive at the hospital, timely treatment can also be delayed due to some preparation steps, such as talking to family members of the patient and providing signed informed consent before rt-PA use and thrombus removal. Similarly, the time interval from onset to femoral artery puncture also varied in our study. In some cases, the time interval was significantly greater than 10 h, leading to a small sample size in the subgroups, which may have had a certain impact on the reliability of our results.
In conclusion, our study provides a basis for the selection of treatment options in patients with acute anterior circulation ischemic stroke within 10 h after the onset of symptoms.
Availability of data and materials
The data sets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kim AS, Cahill E, Cheng NT. Global stroke belt: geographic variation in stroke burden worldwide. Stroke. 2015;46:3564–70.
Moran A, Gu D, Zhao D, Coxson P, Wang YC, Chen CS, et al. Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes. 2010;3(3):243–52.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–110.
Alves HC, Treurniet KM, Jansen IGH, Yoo AJ, Dutra BG, Zhang G, et al. Thrombus migration paradox in patients with acute ischemic stroke. Stroke. 2019;50(11):3156–63.
Kaesmacher J, Boeckh-Behrens T, Simon S, Maegerlein C, Kleine JF, Zimmer C, et al. Risk of thrombus fragmentation during endovascular stroke treatment. AJNR Am J Neuroradiol. 2017;38(5):991–8.
Lou M, Ding J, Hu B, Zhang Y, Li H, Tan Z, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update on organizational stroke management. Stroke Vasc Neurol. 2020;5(3):260–9.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–418.
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15(11):1138–47.
Martins SO, Mont’Alverne F, Rebello LC, Abud DG, Silva GS, Lima FO, et al. Thrombectomy for stroke in the public health care system of Brazil. N Engl J Med. 2020;382(24):2316–26.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–30.
Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Clark W, Dávalos A, et al. Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the SWIFT and STAR studies. JAMA Neurol. 2017;74(3):268–74.
Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without Intravenous alteplase in acute stroke. N Engl J Med. 2020;382(21):1981–93.
Zi W, Qiu Z, Li F, Sang H, Wu D, Luo W, et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: the DEVT randomized clinical trial. JAMA. 2021;325(3):234–43.
Luedi R, Hsieh K, Slezak A, El-Koussy M, Fischer U, Heldner MR, et al. Age dependency of safety and outcome of endovascular therapy for acute stroke. J Neurol. 2014;261(8):1622–7.
Berge E, Whiteley W, Audebert H, De Marchis GM, Fonseca AC, Padiglioni C, et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur Stroke J. 2021. https://doi.org/10.1177/2396987321989865.
Fan S, Bian Y, Wang E, Kang Y, Wang DJJ, Yang Q, et al. An automatic estimation of arterial input function based on multi-stream 3D CNN. Front Neuroinform. 2019;5(13):49.
Larrue V, von Kummer RR, Müller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 2001;32(2):438–41.
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998;352(9136):1245–51.
Tsivgoulis G, Katsanos AH, Mavridis D, Magoufis G, Arthur A, Alexandrov AV. Mechanical thrombectomy improves functional outcomes independent of pretreatment with intravenous thrombolysis. Stroke. 2016;47(6):1661–4.
Chen J, Wan TF, Xu TC, Chang GC, Chen HS, Liu L. Direct endovascular thrombectomy or with prior intravenous thrombolysis for acute ischemic stroke: a meta-analysis. Front Neurol. 2021;12:752698.
Weber R, Nordmeyer H, Hadisurya J, Heddier M, Stauder M, Stracke P, et al. Comparison of outcome and interventional complication rate in patients with acute stroke treated with mechanical thrombectomy with and without bridging thrombolysis. J Neurointerv Surg. 2017;9(3):229–33.
Reiff T, Barthel O, Ringleb PA, Pfaff J, Mundiyanapurath S. Safety of mechanical thrombectomy with combined intravenous thrombolysis in stroke treatment 4.5 to 9 hours from symptom onset. J Stroke Cerebrovasc Dis. 2020;29(11):105204.
Park HK, Chung JW, Hong JH, Jang MU, Noh HD, Park JM, et al. Preceding intravenous thrombolysis in patients receiving endovascular therapy. Cerebrovasc Dis. 2017;44(1–2):51–8.
Abilleira S, Ribera A, Cardona P, Rubiera M, López-Cancio E, Amaro S, et al. Outcomes after direct thrombectomy or combined intravenous and endovascular treatment are not different. Stroke. 2017;48(2):375–8.
Desilles JP, Loyau S, Syvannarath V, Gonzalez-Valcarcel J, Cantier M, Louedec L, et al. Alteplase reduces downstream microvascular thrombosis and improves the benefit of large artery recanalization in stroke. Stroke. 2015;46(11):3241–8.
Ren Y, Churilov L, Mitchell P, Dowling R, Bush S, Yan B. Clot migration is associated with intravenous thrombolysis in the setting of acute ischemic stroke. Stroke. 2018;49(12):3060–2.
Bellwald S, Weber R, Dobrocky T, Nordmeyer H, Jung S, Hadisurya J, et al. Direct mechanical intervention versus bridging therapy in stroke patients eligible for intravenous thrombolysis: a pooled analysis of 2 registries. Stroke. 2017;48(12):3282–8.
Acknowledgements
We thank Medjaden Inc. for their scientific editing of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
XJ wrote the main manuscript text. XJ, PC, and QZ have had access to and verified the data and performed the statistical analyses. PC was responsible for the decision to submit this manuscript and confirms that all authors have seen and approved the final text. XJ, ZJ, SW, JZ, LL, CD, MZ, DW, LZ, XZ, and QZ designed the trial and study protocol. XJ and LL designed or coded the figures and tables. BS, HZ, and FH were interventional neurologists in this study at three advanced stroke centers in Shanxi Province. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committees of Xianyang Hospital of Yan’an University. All patients submitted informed consent for tissue use.
Consent for publication
All authors have seen and agreed to publish the text.
Competing interests
The authors have no conflicts of interest or financial relationships relevant to the submitted work to disclose. No form of payment was given to anyone to produce the manuscript
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ji, X., Song, B., Zhu, H. et al. A study on endovascular treatment alone and bridging treatment for acute ischemic stroke. Eur J Med Res 28, 12 (2023). https://doi.org/10.1186/s40001-022-00966-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00966-8