Abstract
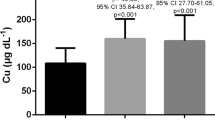
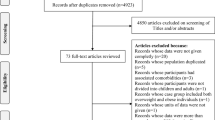
To assess the association between serum copper/zinc ratio (CZR) and overweight/obesity in children. Sociodemographic and clinical data of children aged 8–18 years old were extracted from the National Health and Nutrition Examination Survey (NHANES) database in this cross-sectional study. These associations were explored using weighted univariate and multivariate logistic regression analyses with the odds ratios (ORs) and 95% confidence intervals (CIs). High serum CZR level was related to higher odds of overweight (OR = 1.74), obesity (OR = 5.26), and central obesity (OR = 2.99). Subgroup analyses showed that high serum CZR levels were associated with high odds of overweight in children aged ≥ 12 years old (OR = 2.19) and females (OR = 2.02), while the increased odds of obesity and central obesity were found in children aged ≥ 12 years old and both male and female. Elevated serum CZR level was linked to high odds of childhood overweight, obesity, and central obesity, and this relationship was also found in children with different age and gender.

Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available in the NHANES database, https://www.cdc.gov/nchs/nhanes/index.htm.
References
The UNICEF/WHO/WB (2020) Joint Child Malnutrition Estimates (JME) group released new data. World Health Organization. https://www.who.int/publications/i/item/jme-2020-edition. Accessed 23 Aug 2022
Jebeile H, Kelly AS, O’Malley G, Baur LA (2022) Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol 10(5):351–365. https://doi.org/10.1016/S2213-8587(22)00047-X
Gu K, Xiang W, Zhang Y, Sun K, Jiang X (2019) The association between serum zinc level and overweight/obesity: a meta-analysis. Eur J Nutr 58(8):2971–2982. https://doi.org/10.1007/s00394-018-1876-x
Jeger R, Pfisterer M, Pfister O, Rickenbacher P, Handke M, Gilgen N, Coslovsky M, Kaiser C (2016) First-generation paclitaxel- vs. second-generation zotarolimus-eluting stents in small coronary arteries: the BASKET-SMALL Pilot Study. Postepy Kardiol Interwencyjnej 12(4):314–320. https://doi.org/10.5114/aic.2016.63630
Kim TJ, von dem Knesebeck O (2018) Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ Open 8(1):e019862. https://doi.org/10.1136/bmjopen-2017-019862
Fukunaka A, Fujitani Y (2018) Role of zinc homeostasis in the pathogenesis of diabetes and obesity. Int J Mol Sci 19(2):476. https://doi.org/10.3390/ijms19020476
Yang H, Liu CN, Wolf RM, Ralle M, Dev S, Pierson H, Askin F, Steele KE, Magnuson TH, Schweitzer MA, Wong GW, Lutsenko S (2019) Obesity is associated with copper elevation in serum and tissues. Metallomics 11(8):1363–1371. https://doi.org/10.1039/c9mt00148d
Soujanya KV, Jayadeep AP (2022) Obesity-associated biochemical markers of inflammation and the role of grain phytochemicals. J Food Biochem 46(9):e14257. https://doi.org/10.1111/jfbc.14257
Habib SA, Saad EA, Elsharkawy AA, Attia ZR (2015) Pro-inflammatory adipocytokines, oxidative stress, insulin, Zn and Cu: interrelations with obesity in Egyptian non-diabetic obese children and adolescents. Adv Med Sci 60(2):179–185. https://doi.org/10.1016/j.advms.2015.02.002
Latib A, Colombo A, Castriota F, Micari A, Cremonesi A, De Felice F, Marchese A, Tespili M, Presbitero P, Sgueglia GA, Buffoli F, Tamburino C, Varbella F, Menozzi A (2012) A randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels: the BELLO (Balloon Elution and Late Loss Optimization) study. J Am Coll Cardiol 60(24):2473–2480. https://doi.org/10.1016/j.jacc.2012.09.020
Maradi R, Joshi V, Balamurugan V, Thomas DS, Goud M (2022) Importance of microminerals for maintaining antioxidant function after COVID-19-induced oxidative stress. Rep Biochem Mol Biol 11(3):479–486. https://doi.org/10.52547/rbmb.11.3.479
Formigari A, Gregianin E, Irato P (2013) The effect of zinc and the role of p53 in copper-induced cellular stress responses. J Appl Toxicol 33(7):527–536. https://doi.org/10.1002/jat.2854
Hernandez-Mendoza H, Martinez-Navarro I, Hernandez-Ochoa E, Espinoza-Ruiz M, Lugo-Trampe A, Trujillo-Murillo KDC, Lopez-Garcia MA, Rios-Lugo MJ, Chang-Rueda C (2022) Serum zinc levels are associated with obesity and low-density lipoprotein cholesterol in Mexican adults. J Trace Elem Med Biol 73:127002. https://doi.org/10.1016/j.jtemb.2022.127002
Rios-Lugo MJ, Madrigal-Arellano C, Gaytan-Hernandez D, Hernandez-Mendoza H, Romero-Guzman ET (2020) Association of serum zinc levels in overweight and obesity. Biol Trace Elem Res 198(1):51–57. https://doi.org/10.1007/s12011-020-02060-8
Gu K, Li X, Xiang W, Jiang X (2020) The relationship between serum copper and overweight/obesity: a meta-analysis. Biol Trace Elem Res 194(2):336–347. https://doi.org/10.1007/s12011-019-01803-6
Martinez-Navarro I, Vilchis-Gil J, Cossio-Torres PE, Hernandez-Mendoza H, Klunder-Klunder M, Layseca-Espinosa E, Galicia-Cruz OG, Rios-Lugo MJ (2022) Relationship of serum zinc levels with cardiometabolic traits in overweight and obese schoolchildren from Mexico City. Biol Trace Elem Res 201(9):4307–4319. https://doi.org/10.1007/s12011-022-03533-8
Malavolta M, Piacenza F, Basso A, Giacconi R, Costarelli L, Mocchegiani E (2015) Serum copper to zinc ratio: relationship with aging and health status. Mech Ageing Dev 151:93–100. https://doi.org/10.1016/j.mad.2015.01.004
Kunutsor SK, Voutilainen A, Laukkanen JA (2022) Serum copper-to-zinc ratio and risk of incident pneumonia in Caucasian men: a prospective cohort study. Biometals 35(5):921–933. https://doi.org/10.1007/s10534-022-00414-4
Guo CH, Chen PC, Yeh MS, Hsiung DY, Wang CL (2011) Cu/Zn ratios are associated with nutritional status, oxidative stress, inflammation, and immune abnormalities in patients on peritoneal dialysis. Clin Biochem 44(4):275–280. https://doi.org/10.1016/j.clinbiochem.2010.12.017
Malavolta M, Giacconi R, Piacenza F, Santarelli L, Cipriano C, Costarelli L, Tesei S, Pierpaoli S, Basso A, Galeazzi R, Lattanzio F, Mocchegiani E (2010) Plasma copper/zinc ratio: an inflammatory/nutritional biomarker as predictor of all-cause mortality in elderly population. Biogerontology 11(3):309–319. https://doi.org/10.1007/s10522-009-9251-1
Jeong SY, Shim HY, Lee YJ, Park B (2021) Association between copper-zinc ratio in hair and neutrophil-lymphocyte ratio within the context of a normal white blood cell count among overweight or obese Korean individuals: a pilot study. Korean J Fam Med 42(3):240–244. https://doi.org/10.4082/kjfm.20.0018
Rodriguez A, Rodriguez Alemparte M, Fernandez Pereira C, Sampaolesi A, da Rocha Loures Bueno R, Vigo F, Obregon A, Palacios IF, Investigators L (2005) Latin American randomized trial of balloon angioplasty vs coronary stenting for small vessels (LASMAL): immediate and long-term results. Am J Med 118 (7):743–751. https://doi.org/10.1016/j.amjmed.2005.03.030
Savage MP, Fischman DL, Rake R, Leon MB, Schatz RA, Penn I, Nobuyoshi M, Moses J, Hirshfeld J, Heuser R, Baim D, Cleman M, Brinker J, Gebhardt S, Goldberg S (1998) Efficacy of coronary stenting versus balloon angioplasty in small coronary arteries fn1fn1This study was supported in part by a grant from Johnson & Johnson Interventional Systems Inc, Warren, New Jersey. J Am Coll Cardiol 31(2):307–311. https://doi.org/10.1016/s0735-1097(97)00511-1
Wang YY, Sun RH (2016) Application of PASS in sample size estimation of non-inferiority, equivalence and superiority design in clinical trials. Zhonghua Liu Xing Bing Xue Za Zhi 37(5):741–744. Chinese. https://doi.org/10.3760/cma.j.issn.0254-6450.2016.05.032.
Ayeser T, Basak M, Arslan K, Sayan I (2016) Investigating the correlation of the number of diagnostic criteria to serum adiponectin, leptin, resistin, TNF-alpha, EGFR levels and abdominal adipose tissue. Diabetes Metab Syndr 10(2 Suppl 1):S165-169. https://doi.org/10.1016/j.dsx.2016.03.010
Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE (2011) Measurement of adults’ sedentary time in population-based studies. Am J Prev Med 41(2):216–227. https://doi.org/10.1016/j.amepre.2011.05.005
Wang P, Chen C, Song C, Jia J, Wang Y, Mu W (2022) High cholesterol and low triglycerides are associated with total lumbar bone mineral density among adults aged 50 years and over: The NHANES 2017–2020. Front Med (Lausanne) 9:923730. https://doi.org/10.3389/fmed.2022.923730
Habib A, Molayemat M, Habib A (2020) Elevated serum TSH concentrations are associated with higher BMI Z-scores in southern Iranian children and adolescents. Thyroid Res 13:9. https://doi.org/10.1186/s13044-020-00084-9
Gutin I (2020) Educational differences in mortality associated with central obesity: Decomposing the contribution of risk and prevalence. Soc Sci Res 90:102445. https://doi.org/10.1016/j.ssresearch.2020.102445
Peterson SJ, Foley S (2021) Clinician’s guide to understanding effect size, alpha level, power, and sample size. Nutr Clin Pract 36(3):598–605. https://doi.org/10.1002/ncp.10674
Escobedo-Monge MF, Barrado E, Parodi-Román J, Escobedo-Monge MA, Torres-Hinojal MC, Marugán-Miguelsanz JM (2021) Copper and copper/Zn ratio in a series of children with chronic diseases: a cross-sectional study. Nutrients 13(10):3578. https://doi.org/10.3390/nu13103578
Laouali N, MacDonald CJ, Shah S, El Fatouhi D, Mancini FR, Fagherazzi G, Boutron-Ruault MC (2021) Dietary copper/zinc ratio and type 2 diabetes risk in women: the E3N cohort study. Nutrients 13(8):2502. https://doi.org/10.3390/nu13082502
Bonaventura P, Benedetti G, Albarede F, Miossec P (2015) Zinc and its role in immunity and inflammation. Autoimmun Rev 14(4):277–285. https://doi.org/10.1016/j.autrev.2014.11.008
Malavolta M, Piacenza F, Basso A, Giacconi R, Costarelli L, Mocchegiani E (2015) Serum Cu to Zn ratio: relationship with aging and health status. Mech Ageing Dev 151:93–100. https://doi.org/10.1016/j.mad.2015.01.004
El-Jamal S, Elfane H, Chamlal H, Barakat I, Daif H, Mziwira M, Fassouane A, Belahsen R (2022) Assessment of diet quality in children and adolescents with type 1 diabetes. Rocz Panstw Zakl Hig 73(4):413–422. https://doi.org/10.32394/rpzh.2022.0229
Wang L, Liu M, Ning D, Zhu H, Shan G, Wang D, Ping B, Yu Y, Yang H, Yan K, Pan H, Gong F (2020) Low serum ZAG levels correlate with determinants of the metabolic syndrome in Chinese subjects. Front Endocrinol (Lausanne) 24(11):154. https://doi.org/10.3389/fendo.2020.00154
Wang X, Karvonen-Gutierrez CA, Herman WH, Mukherjee B, Park SK (2022) Metals and risk of incident metabolic syndrome in a prospective cohort of midlife women in the United States. Environ Res 210:112976. https://doi.org/10.1016/j.envres.2022.112976
Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L, Keshteli AH, Feizi A, Feinle-Bisset C, Adibi P (2016) Nutrient patterns and their relation to general and abdominal obesity in Iranian adults: findings from the SEPAHAN study. Eur J Nutr 55(2):505–518. https://doi.org/10.1007/s00394-015-0867-4
Osadchuk LV, Danilenko AD, Osadchuk AV (2022) A relationship between zinc and anthropometric and metabolic indicators of obesity in the population of young Russian men. Biomed Khim 68(5):383–389. https://doi.org/10.18097/PBMC20226805383
Shi L, Jiang Z, Zhang L (2022) Childhood obesity and central precocious puberty. Front Endocrinol (Lausanne) 13:1056871. https://doi.org/10.3389/fendo.2022.1056871
Dubois V, Laurent MR, Jardi F, Antonio L, Lemaire K, Goyvaerts L, Deldicque L, Carmeliet G, Decallonne B, Vanderschueren D, Claessens F (2016) Androgen deficiency exacerbates high-fat diet-induced metabolic alterations in male mice. Endocrinology 157(2):648–665. https://doi.org/10.1210/en.2015-1713
De Paoli M, Zakharia A, Werstuck GH (2021) The role of estrogen in insulin resistance: a review of clinical and preclinical data. Am J Pathol 191(9):1490–1498. https://doi.org/10.1016/j.ajpath.2021.05.011
Lima SC, Arrais RF, Sales CH, Almeida MG, de Sena KC, Oliveira VT, de Andrade AS, Pedrosa LF (2006) Assessment of copper and lipid profile in obese children and adolescents. Biol Trace Elem Res 114(1–3):19–29. https://doi.org/10.1385/BTER:114:1:19
Fan Y, Zhang C, Bu J (2017) Relationship between selected serum metallic elements and obesity in children and adolescent in the U.S. Nutrients 9(2):104. https://doi.org/10.3390/nu9020104
Marreiro DN, Fisberg M, Cozzolino SM (2004) Zinc nutritional status and its relationships with hyperinsulinemia in obese children and adolescents. Biol Trace Elem Res 100(2):137–149. https://doi.org/10.1385/bter:100:2:137
Olusi S, Al-Awadhi A, Abiaka C, Abraham M, George S (2003) Serum copper levels and not zinc are positively associated with serum leptin concentrations in the healthy adult population. Biol Trace Elem Res 91(2):137–144. https://doi.org/10.1385/BTER:91:2:137
Funding
This study was supported by China International Medical Foundation Pediatric Endocrinology young and middle-aged physicians growth research fund project (NO: Z-2019- 41-2101- 01).
Author information
Authors and Affiliations
Contributions
MD and XC designed the study. MD wrote the manuscript. MQ, YQ, and TW collected, analyzed, and interpreted the data. XC critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The data were deidentified, and all the participants provided informed consent. No ethical approval of our agency’s IRB was required since this survey was publicly available.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, M., Qiu, M., Qian, Y. et al. Serum Copper/Zinc Ratio in Overweight and Obese Children: a Cross-Sectional Study. Biol Trace Elem Res 202, 1539–1549 (2024). https://doi.org/10.1007/s12011-023-03790-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03790-1