Abstract
This study is based on the premise that the application of chemical synthesis strategies to structurally modify commercial drugs by complexation with biometals is a valid procedure to improve their biological effects. Our purpose is to synthesize a compound with greater efficacy than the original drug, able to enhance its antihypertensive and cardiac pharmacological activity. Herein, the structure of the coordination compound of Zn(II) and the antihypertensive drug olmesartan, [Zn(Olme)(H2O)2] (ZnOlme), is presented. After 8 weeks of treatment in SHR male rats, ZnOlme displayed a better blood pressure-lowering activity compared with olmesartan, with a noticeable effect even in the first weeks of treatment, while ZnCl2 showed similar results than the control. ZnOlme also reduced left ventricle (LV) weight and left ventricle/tibia length ratio (LV/TL), posterior wall thickness (PWT), and intraventricular septum in diastole (IVSd) suggesting its potential to prevent LV hypertrophy. Besides, ZnOlme reduced interstitial fibrosis (contents of collagen types I and III, responsible for giving rigidity and promoting vascular elasticity, respectively). The recovery of heart function was also evidenced by fractional shortening (diastolic left ventricular/systolic left ventricular) diameter determinations. Furthermore, ZnOlme increased the antioxidant capacity and prevented cardiac oxidative stress: it enhanced the reduction of reactive oxygen species generation, exerted a significant decrease in lipid peroxidation and enhanced glutathione contents in heart tissues compared to the control, Zn, and olmesartan treatments. Our results demonstrate that continuous oral administration of ZnOlme causes a better antihypertensive effect and grants enhancement of cardioprotection through antioxidant activity, in combination with hemodynamic improvement.
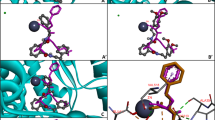
Graphical Abstract








Similar content being viewed by others
Data Availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Al-Makki A, DiPette D, Whelton PK et al (2022) Hypertension pharmacological treatment in adults: a World Health Organization guideline executive summary. Hypertension 79:293–301. https://doi.org/10.1161/hypertensionaha.121.18192
van Haaster MC, McDonough AA, Gurley SB (2018) Blood pressure regulation by the angiotensin type 1 receptor in the proximal tubule. Curr Opin Nephrol Hypertens 27:1–7. https://doi.org/10.1097/MNH.0000000000000373
Carabello BA (2021) The pathophysiology of afterload mismatch and ventricular hypertrophy. Structural Heart 5:446–456. https://doi.org/10.1080/24748706.2021.1944708
Bhullar SK, Shah AK, Dhalla NS (2021) Role of angiotensin II in the development of subcellular remodeling in heart failure. Exp Ther Med 2:352–371. https://doi.org/10.37349/emed.2021.00054
Ladhari A, la Mura G, di Marino C et al (2021) Sartans: what they are for, how they degrade, where they are found and how they transform. Sustain Chem Pharm 20:100409. https://doi.org/10.1016/j.scp.2021.100409
Zhang H, Unal H, Desnoyer R et al (2015) Structural basis for ligand recognition and functional selectivity at angiotensin receptor. J Biol Chem 290:29127–29139. https://doi.org/10.1074/jbc.M115.689000
Sharma P, Reddy PK, Kumar B (2021) Trace element zinc, a nature’s gift to fight unprecedented global pandemic COVID-19. Biol Trace Elem Res 199:3213–3221. https://doi.org/10.1007/s12011-020-02462-8
Jurowski K, Szewczyk B, Nowak G, Piekoszewski W (2014) Biological consequences of zinc deficiency in the pathomechanisms of selected diseases. J Biol Inorg Chem 19:1069–1079. https://doi.org/10.1007/s00775-014-1139-0
Zhang Q, Xue Y, Fu Y et al (2022) Zinc Deficiency aggravates oxidative stress leading to inflammation and fibrosis in lung of mice. Biol Trace Elem Res 200:4045–4057. https://doi.org/10.1007/s12011-021-03011-7
Pellei M, del Bello F, Porchia M, Santini C (2021) Zinc coordination complexes as anticancer agents. Coord Chem Rev 445:214088. https://doi.org/10.1016/j.ccr.2021.214088
Martínez VR, Aguirre MV, Todaro JS et al (2021) Zinc complexation improves angiotensin II receptor type 1 blockade and in vivo antihypertensive activity of telmisartan. Future Med Chem 13:13–23. https://doi.org/10.4155/fmc-2020-0093
Säbel CE, Neureuther JM, Siemann S (2010) A spectrophotometric method for the determination of zinc, copper, and cobalt ions in metalloproteins using Zincon. Anal Biochem 397:218–226. https://doi.org/10.1016/j.ab.2009.10.037
Al-Majed AA, Bakheit AHH, Abdel Aziz HA, Al-Jallal AAM (2017) Olmesartan. In: Profiles of Drug Substances, Excipients and Related Methodology. Academic Press Inc., pp 241–286
Dams I, Ostaszewska A, Puchalska M et al (2015) Synthesis and physicochemical characterization of the process-related impurities of olmesartan medoxomil. Do 5-(Biphenyl-2-yl)-1-triphenylmethyltetrazole Intermediates in Sartan Syntheses Exist? Molecules 20:21346–21363. https://doi.org/10.3390/molecules201219762
Li J, Kemp BA, Howell NL et al (2019) Metabolic changes in spontaneously hypertensive rat hearts precede cardiac dysfunction and left ventricular hypertrophy. J Am Heart Assoc 8. https://doi.org/10.1161/JAHA.118.010926
Charan J, Kantharia ND (2013) How to calculate sample size in animal studies? J Pharmacol Pharmacother 4:303–306. https://doi.org/10.4103/0976-500X.119726
Fernandes-Santos C, de Souza ML, Mandarim-de-Lacerda CA (2009) Favorable cardiac and aortic remodeling in olmesartan-treated spontaneously hypertensive rats. Heart Vessels 24:219–227. https://doi.org/10.1007/s00380-008-1104-3
Jones EF, Harrap SB, Calafiore P, Tonkin AM (1992) Development and validation of echocardiography methods for estimating left ventricular mass in rats. Clin Exp Pharmacol Physiol 19:361–364. https://doi.org/10.1111/j.1440-1681.1992.tb00472.x
Devereux RB, Reichek N (1977) Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 55:613–618. https://doi.org/10.1161/01.CIR.55.4.613
Mousavi K, Niknahad H, Ghalamfarsa A et al (2020) Taurine mitigates cirrhosis-associated heart injury through mitochondrial-dependent and antioxidative mechanisms. Clin Exp Hepatol 6:207–219. https://doi.org/10.5114/ceh.2020.99513
Hissin PJ, Hilf R (1976) A fluorometric method for determination of oxidized and reduced glutathione in tissues. Anal Biochem 74:214–226. https://doi.org/10.1016/0003-2697(76)90326-2
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358. https://doi.org/10.1016/0003-2697(79)90738-3
National Center for Biotechnology Information (2022) PubChem Compound Summary for CID 158781, Olmesartan. https://pubchem.ncbi.nlm.nih.gov/compound/Olmesartan. Accessed 18 Sept 2022
Yanagisawa H, Amemiya Y, Kanazaki T et al (1996) Nonpeptide angiotensin II receptor antagonists: synthesis, biological activities, and structure−activity relationships of imidazole-5-carboxylic acids bearing alkyl, alkenyl, and hydroxyalkyl substituents at the 4-position and their related compounds. J Med Chem 39:323–338. https://doi.org/10.1021/jm950450f
Deacon G (1980) Relationships between the carbon-oxygen stretching frequencies of carboxylato complexes and the type of carboxylate coordination. Coord Chem Rev 33:227–250. https://doi.org/10.1016/S0010-8545(00)80455-5
Franca CA, Etcheverry SB, Pis Diez R, Williams PAM (2009) Irbesartan: FTIR and Raman spectra. Density functional study on vibrational and NMR spectra. J Raman Spectrosc 40:1296–1300. https://doi.org/10.1002/jrs.2282
Akhlaghinia B, Rezazadeh S (2012) A novel approach for the synthesis of 5-substituted-1H-tetrazoles. J Braz Chem Soc 23:2197–2203. https://doi.org/10.1590/S0103-50532013005000005
Sinirlioglu D, Muftuoglu AE, Bozkurt A (2014) Investigation of proton conductivity of inorganic–organic hybrid membranes based on boronic acid and tetrazole. J Polym Res 21:526. https://doi.org/10.1007/s10965-014-0526-0
Kellici T, Ntountaniotis D, Kritsi E et al (2015) Leveraging NMR and X-ray data of the free ligands to build better drugs targeting angiotensin II type 1 G-protein coupled receptor. Curr Med Chem 23:36–59. https://doi.org/10.2174/0929867323666151117122116
Zhang H, Unal H, Gati C et al (2015) Structure of the angiotensin receptor revealed by serial femtosecond crystallography. Cell 161:833–844. https://doi.org/10.1016/j.cell.2015.04.011
Benesi HA, Hildebrand JH (1949) A spectrophotometric investigation of the interaction of iodine with aromatic hydrocarbons. J Am Chem Soc 71:2703–2707. https://doi.org/10.1021/ja01176a030
Uchinaka A, Yoshida M, Tanaka K et al (2018) Overexpression of collagen type III in injured myocardium prevents cardiac systolic dysfunction by changing the balance of collagen distribution. J Thorac Cardiovasc Surg 156:217–226.e3. https://doi.org/10.1016/j.jtcvs.2018.01.097
Wu C-Y, Hu H-Y, Chou Y-J et al (2015) High blood pressure and all-cause and cardiovascular disease mortalities in community-dwelling older adults. Medicine 94:e2160. https://doi.org/10.1097/MD.0000000000002160
Maulik SK, Kumar S (2012) Oxidative stress and cardiac hypertrophy: a review. Toxicol Mech Methods 22:359–366. https://doi.org/10.3109/15376516.2012.666650
Blaustein MP (2017) How does pressure overload cause cardiac hypertrophy and dysfunction? High-ouabain affinity cardiac Na + pumps are crucial. Am J Physiol Heart Circ Physiol 313:H919–H930. https://doi.org/10.1152/ajpheart.00131.2017
Shimizu I, Minamino T (2016) Physiological and pathological cardiac hypertrophy. J Mol Cell Cardiol 97:245–262. https://doi.org/10.1016/j.yjmcc.2016.06.001
Sukumaran V, Watanabe K, Veeraveedu PT et al (2011) Olmesartan, an AT 1 antagonist, attenuates oxidative stress, endoplasmic reticulum stress and cardiac inflammatory mediators in rats with heart failure induced by experimental autoimmune myocarditis. Int J Biol Sci 7:154–167. https://doi.org/10.7150/ijbs.7.154
Bernardo BC, Weeks KL, Pretorius L, McMullen JR (2010) Molecular distinction between physiological and pathological cardiac hypertrophy: experimental findings and therapeutic strategies. Pharmacol Ther 128:191–227. https://doi.org/10.1016/j.pharmthera.2010.04.005
Tomita N, Yamasaki K, Osako MK, Komai N, Shimosato T, Morishita R (2009) Combination therapy based on the angiotensin receptor blocker olmesartan for vascular protection in spontaneously hypertensive rats. Mol Med Rep 2:733–738. https://doi.org/10.3892/mmr_00000164
Nagasu H, Satoh M, Yorimitsu D et al (2011) Comparison of combination therapy of olmesartan plus azelnidipine or hydrochlorothiazide on renal and vascular damage in SHR/NDmcr-cp rats. Kidney Blood Press Res 34:87–96. https://doi.org/10.1159/000323535
Chasapis CT, Ntoupa P-SA, Spiliopoulou CA, Stefanidou ME (2020) Recent aspects of the effects of zinc on human health. Arch Toxicol 94:1443–1460. https://doi.org/10.1007/s00204-020-02702-9
Yoshikawa Y, Yasui H (2012) Zinc Complexes developed as metallopharmaceutics for treating diabetes mellitus based on the bio-medicinal inorganic chemistry. Curr Top Med Chem 12:210–218. https://doi.org/10.2174/156802612799078874
Martinez VR, Martins Lima A, Stergiopulos N et al (2023) Effect of the structural modification of Candesartan with Zinc on hypertension and left ventricular hypertrophy. Eur J Pharmacol 946:175654. https://doi.org/10.1016/j.ejphar.2023.175654
Conrad CH, Brooks WW, Hayes JA et al (1995) Myocardial fibrosis and stiffness with hypertrophy and heart failure in the spontaneously hypertensive rat. Circulation 91:161–170. https://doi.org/10.1161/01.CIR.91.1.161
Kupfahl C (2000) Angiotensin II directly increases transforming growth factor β1 and osteopontin and indirectly affects collagen mRNA expression in the human heart. Cardiovasc Res 46:463–475. https://doi.org/10.1016/S0008-6363(00)00037-7
Khan R, Sheppard R (2006) Fibrosis in heart disease: understanding the role of transforming growth factor-beta1 in cardiomyopathy, valvular disease and arrhythmia. Immunology 118:10–24. https://doi.org/10.1111/j.1365-2567.2006.02336.x
Tian H, Yu D, Hu Y et al (2018) Angiotensin II upregulates cyclophilin A by enhancing ROS production in rat cardiomyocytes. Mol Med Rep 18:4349–4355. https://doi.org/10.3892/mmr.2018.9448
Seddon M, Looi YH, Shah AM (2007) Oxidative stress and redox signalling in cardiac hypertrophy and heart failure. Heart 93:903–907. https://doi.org/10.1136/hrt.2005.068270
Tanaka M, Umemoto S, Kawahara S et al (2005) Angiotensin II type 1 receptor antagonist and angiotensin-converting enzyme inhibitor altered the activation of Cu/Zn-containing superoxide dismutase in the heart of stroke-prone spontaneously hypertensive rats. Hypertens Res 28:67–77. https://doi.org/10.1291/hypres.28.67
Bajic VP, van Neste C, Obradovic M et al (2019) Glutathione “redox homeostasis” and its relation to cardiovascular disease. Oxid Med Cell Longev 2019:1–14. https://doi.org/10.1155/2019/5028181
Acknowledgements
The authors thank to Leandro Di Cianni for the technical support to measure the blood pressure.
Funding
The following grants supported this work: UNLP [X/871, V720], CONICET [PIP 1999], CICPBA and ANPCyT [PICT-2019-0945] Argentina. AGRG and VRM are fellowship holders of CONICET. ELP, VDG, and EGF are research fellows of CONICET and PAMW is research fellow of CICPBA.
Author information
Authors and Affiliations
Contributions
Andrés G. Restrepo Guerrero: conceptualization, methodology, software, data curation. Valeria R. Martinez: methodology, data curation, writing—original draft review and editing. Jorge O. Velez Rueda: methodology and data curation. Enrique L. Portiansky: conceptualization, methodology, writing—review and editing. Verónica De Giusti; methodology writing—review and editing. Evelina G. Ferrer: conceptualization, methodology, writing—review and editing. Patricia A.M Williams: conceptualization, methodology, writing original draft—review and editing, supervision.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 3.51 MB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Restrepo Guerrero, A.G., Martinez, V.R., Velez Rueda, J.O. et al. Complexation of the Antihypertensive Drug Olmesartan with Zn: In Vivo Antihypertensive and Cardiac Effects. Biol Trace Elem Res 202, 246–257 (2024). https://doi.org/10.1007/s12011-023-03670-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03670-8