Abstract
To investigate iodine status and characteristics of breastfeeding women and infants in Zhengzhou after the implementation of the new national standard of iodine in edible salt, so as to provide the basis for formulating prevention and control measures. Urine samples from 28,730 infants aged 0–2 years and 17,977 breastfeeding women who received preventive health care in 12 districts/cities of Zhengzhou from 2012 to 2019 were collected to measure urinary iodine concentration (UIC). A total of 350 pairs of unweaned infants and their mothers were included in this study. After the implementation of the new national standard of iodine in edible salt, the iodine deficiency of infants aged 0–2 years showed a trend of decreasing first and then increasing, but generally the iodine nutrition of infants aged 0–2 years was at the appropriate level in 8 years. There was a gradual decrease in iodine deficiency among breastfeeding women over an 8-year period. And the median UIC of breastfeeding women in 8 years was at iodine nutrition appropriate level. In addition, the UIC of breastfeeding mothers was positively associated with that of infants (r = 0.104, P = 0.004). After the implementation of the new national standard of iodine in edible salt, breastfeeding women and infants in Zhengzhou generally were at an appropriate level of iodine nutrition, and there was a significant positive correlation between the UIC of breastfeeding mothers and infants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iodine is an essential trace element for human beings and one of the key components for the synthesis of thyroid hormone [1]. The thyroid hormone regulates the metabolic process of most cells and plays an important role in human growth, development, and metabolism [2]. Chronic iodine deficiency can cause abnormal physical and mental development in infants and children, thus leading to cretinism [3]. Salt iodization has been recognized as an effective, convenient, and economical method of iodine supplementation [4], and is recognized as an important pillar of the global plan to eradicate deficiency diseases [5].
China used to be the largest country with iodine deficiency [6], and twelve districts and counties in Zhengzhou, Henan Province, are also iodine deficiency areas [7]. China began implementing the policy of “Universal Salt Iodization (USI)” in 1995 [8]. In the two decades since iodized salt was made mandatory, significant progress has been made and iodine deficiency has been greatly improved [9]. According to the National Survey on Iodine Deficiency Disorders (IDD), China has been on a sustainable path to eliminating IDD since 2005 [10]. As a result, interventions to combat IDD have also been geared towards preventing and controlling excessive iodine intake in the population. A community-based epidemiological survey of schoolchildren in China showed that the median urinary iodine was close to or higher than 200 μg/L in 2009–2010 [11]. Zhengzhou carried out iodine nutrition monitoring for key populations annually. According to the national iodine deficiency disease monitoring results in 2011 [12], the median urinary iodine concentration of children aged 8–10 years in Henan province was 201 μg/L. These data indicated that the iodine level of the general population in Henan province exceeded the suitable iodine range of 100 ~ 199 μg/L. Therefore, Since March 2012, Henan Province has implemented the national food safety standard “Iodine Content in Edible Salt,” and the iodized salt concentration has been reduced from the original (35 ± 15) mg/kg to 30 mg/kg ± 30% [13].
According to the survey, under the background of the universal implementation of salt iodization in China, there are still differences in iodine intake in different regions [14]. In addition, differences in iodine intake due to geographical distribution, dietary habits, and water iodine content are also of concern. According to the results of iodine nutrition monitoring of key population in 2019, the median UIC of children aged 8–10 years in Kunshan City, Jiangsu Province, Ningxia Hui Autonomous Region, and Beijing was 228.0 μg/L, 205 μg/L, and 173 μg/L, respectively [15,16,17]. Therefore, individualized assessment of the iodine deficiency of breastfeeding mothers and infants in Zhengzhou after the implementation of the new national salt iodine standard is very necessary for the follow-up adjustment of iodized salt in Henan Province.
Zero to 2 years old is also an important period of neural development for infants and young children. Adequate iodine intake is needed to maintain normal thyroid function and ensure brain development. Cao et al. [18] demonstrated that the intelligence quotient (IQ) of children in areas with severe iodine deficiency was 12.45 points lower than that of those in areas with sufficient iodine. A relevant meta-analysis also confirmed that the IQ scores of iodine-deficient children under 5 years old were 6.9 to 10.2 points lower than those of iodine-adequate children [19]. The World Health Organization recommends exclusive breastfeeding within 6 months after birth [20]. Iodine nutrition for breastfed infants depends on the amount of iodine in breast milk to ensure optimal thyroid function during the first 6 months of life [21]. In an experimental study of the effects of iodine deficiency on the brain development of neonatal rats, it was found that severe iodine deficiency in female rats significantly reduced the mRNA and protein levels of protein-2 in Purkinesia cells of neonatal rats, suggesting cerebellar retardation [22]. In a meta-analysis, the results showed that iodine supplementation during pregnancy can improve the iodine status in pregnant women and their offspring [23]. Therefore, iodine deficiency in breastfeeding mothers will affect the iodine nutrition of infants to a certain extent [24].
Therefore, we conducted this study to evaluate the iodine deficiency status of 0 ~ 2-year-old infants and breastfeeding women from 2012 to 2019, and to investigate the effect of maternal iodine nutritional status on their offspring.
Methods
Participants
This is a cross-sectional study. In each county (city, district) of Zhengzhou, one hospital, a center for disease control and prevention, and a community service center carrying out vaccination services were randomly selected. The participants included in this study were 0–2-year-old infants who were vaccinated and their mothers. The number of breastfeeding women and infants aged 0 to 2 years was surveyed each year. The inclusion criteria for the participants in this study were (1) healthy cases and (2) residents in each district or county of Zhengzhou for at least 6 months. Exclusion criteria were as follows: (1) multiple births and (2) a history of long-term medical conditions and medication. Because complementary foods for infants older than 6 months of age may affect their iodine intake, only exclusively breastfeeding mothers who had not consumed iodine-rich foods in the last 3 days and their infants (n = 350) up to 6 months of age were matched for analysis.
The Medical Ethics Committee of Zhengzhou Center for Disease Control and Prevention approved the study and was in accordance with the Declaration of Helsinki. Written informed consent was obtained from all mothers.
Collection of Questionnaires
The face-to-face structured questionnaire completed by trained researchers was adopted to collect the following information: (1) sociodemographic information: mother’s age, occupation, family monthly income, and infant feeding methods; (2) the UIC of infants and their mothers; (3) mother’s intake of iodine-rich food in recent 3 days: iodine-rich food is considered to be seaweed, kelp, and other seafood.
Laboratory Analysis
Approximately 10–20 mL mid-stream urine was collected from each subject in the morning, which was sealed in sterile polyethylene plastic test tubes and stored in an icebox at 4 to 8℃, and the collection date and time were recorded. UIC was tested using “WS/T 107–2006 Arsenic-Cerium Catalytic Spectrophotometric Determination of Iodine in Urine” [25]. The external quality control was provided by the China National Clinical Iodine Deficiency Disorders Reference Laboratory. The results showed that the coefficient of variation of UIC in our laboratory was 2.0% at 68.2 ± 1.3 μg/L and 0.9% at 193.0 ± 10.0 μg/L.
Definition of Iodine Deficiency
According to the evaluation standard of iodine nutritional status of the population recommended by WHO, UNICEF, and ICCIDD [26], a median urinary iodine level < 100 μg/L in breastfeeding women and infants aged < 2 years indicate iodine deficiency.
Statistical Analysis
The SPSS (Version 21.0.0.0, IBM, America) was subsequently used for statistical description and statistical analysis of the data obtained. UIC was not normally distributed; thus, the results were described for the median (25th percentile, 75th percentile). Numbers (percentages) for the categorical variables. The chi-square test was used to compare iodine deficiency rates among different groups. The Kruskal–Wallis test was used to compare urinary iodine between multiple groups. If the difference was statistically significant, pairwise comparisons were conducted and Bonferroni was used to correct the P values. Spearman was used for correlation analysis. Prism (Version 9.0.0, GraphPad Software, LLC, America) was used to plot the trend. Two-sided P values < 0.05 were considered statistically significant.
Quality Control
Before the investigation, the on-site investigators were trained, the investigation methods and implementation rules were uniformly stipulated, and special personnel were programmed to be responsible for sample collection, laboratory testing, and laboratory quality control. Laboratories handling urine iodine testing were required to pass an external quality control assessment program before they could carry out laboratory testing. In the process of testing, the standard curve and quality control samples were to meet relevant requirements.
Results
General Characteristics of Infants and Breastfeeding Women
Maternal and infant characteristics are shown in Table 1. A total of 28,730 0–2-year-old infants (57.5% boys) were recruited from 2012 to 2019, of whom 44.2% were breastfed. Correspondingly, a total of 17,977 breastfeeding mothers were included, with an average age of 27.25 ± 4.7 years (range: 16–47 years). The flow chart of the inclusion process is shown in Fig. 1.
Iodine Status Among Infants and Associations with Their Characteristics
A total of 28,730 urine samples of infants aged 0 to 2 years were tested, among which the iodine deficiency rate was 4.9% in boys and 5.7 in girls. The sex distribution difference was statistically significant (P = 0.001). In terms of age range, the iodine deficiency rate was 3.4% for infants aged 0 to 3 months, 3.9% for infants aged 4 to 6 months, 7.6% for infants aged 7 to 12 months, and 15.7% for infants aged 13 to 24 months. The age distribution of iodine deficiency was statistically significant between 0 to 3 months, 7 to 12 months, and 13 to 24 months (P < 0.05), and there was no significant difference between 4 and 6 months of age (P < 0.05). The distribution of iodine deficiency in infants aged 0 to 2 was different between urban and rural areas (P = 0.001). The details are shown in Table 2.
The iodine deficiency rate of infants with different feeding methods in different age groups was compared (Table 3), and the difference in iodine deficiency rate in infants with different feeding methods was statistically significant from 0 to 3 months (P = 0.001). The iodine deficiency rate of artificially fed infants was significantly higher than that of the other two groups. The iodine deficiency rate of infants with different feeding methods in different age groups was compared, and the difference in iodine deficiency rate in infants with different feeding methods was statistically significant from 0 to 3 months. The iodine deficiency rate of artificially fed infants was significantly higher than that of the other two groups (P > 0.05).
Trend in UIC Across Time Among Infants
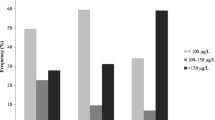
The mean or appropriate level of UIC in infants aged 0–2 years was 217.65 μg/L. From 2012 to 2019, there were differences in the number of infants aged 0–2 years with iodine deficiency in Zhengzhou during the 8 years (P < 0.001) (Table 4). From the line chart, the median UIC of infants aged 0–2 years was relatively stable and at the appropriate iodine level (Fig. 2), indicating that infants aged 0–2 years in Zhengzhou had a good iodine nutritional status.
Iodine Status of Breastfeeding Mothers and Associations with Their Characteristics
A total of 17,977 urine samples from breastfeeding women were tested, with an iodine deficiency rate of 16.4%. The iodine deficiency rates were 17.5%, 16.1%, 17.3%, and 16.4% for those under 20 years of age, 20–29 years of age, 30–39 years of age, and over 40 years of age. There was no difference in age distribution among breastfeeding women with iodine deficiency (P = 0.259). There was no significant difference in the distribution of iodine deficiency in breastfeeding women between urban and rural areas (P = 0.237). The details are shown in Table 5.
Trend in UIC Across Time Among Breastfeeding Women
From 2012 to 2019, there were significant differences in the number of breastfeeding women with iodine deficiency in Zhengzhou during the 8 years (P < 0.001) (Table 6). From the line chart, the median urinary iodine of breastfeeding women was at a relatively stable level and at the appropriate iodine level (Fig. 3), indicating that the iodine nutritional status of breastfeeding women in Zhengzhou was good.
Concordance Between Iodine Status Among Infants and Their Mothers
Of all the participants, 350 pairs of unweaned infants and their mothers were matched. As is shown in Fig. 4, paired correlation analysis was conducted to compare the UIC between breastfed infants who had not been weaned and their breastfeeding mothers. The results showed that there was a significant positive correlation between breastfed infants and their mothers (n = 350, r = 0.104, P = 0.004).
Discussion
Iodine is one of the essential trace elements in the human body and plays an important role in human growth, development, and metabolism [27]. The definition of iodine nutrition status in the population recommended by WHO is an important indicator to evaluate the iodine nutrition level of the population, which can reflect the recent iodine nutrition status [28]. Iodine deficiency has resurfaced in some developed countries, especially in pregnant and breastfeeding women and children [29]. Through the implementation of this study, we found that the iodine nutrition level of lactating women and infants in Zhengzhou, China, is generally at an appropriate level. When a breastfeeding woman is iodine-deficient, the amount of iodine available to the baby through breast milk decreases, resulting in the baby’s own iodine deficiency, which affects the development of the nervous system. In this study, it is found that the UIC of breastfeeding mothers and infants is significantly positively correlated (r = 0.104, P = 0.004). In a randomized controlled trial conducted in Ningxia Hui Autonomous Prefecture [30], infants weaned under 3 years of age in the intervention group were given 40 mg iodized oil every year for 4 consecutive years. It was found that the developmental quotient (DQ) value increased from 92.8 to 104.3, the proportion of normal height and above increased from 65.0 to 82.1%, and the proportion of normal weight and above increased from 59.3 to 81.4%. DQ value, height, and weight were significantly different from those before the intervention (P < 0.05). Therefore, appropriate iodine levels are critical for breastfeeding women and infants.
According to the urine iodine standard recommended by WHO, the urine iodine status of key populations in Zhengzhou City during the past 8 years was evaluated and the iodine nutrition of breastfeeding women and infants was found to be in an appropriate state. Monitoring of infants found that there was a statistically significant difference in urinary iodine in infants of different ages, and the number of people with iodine deficiency increased with age, which was consistent with the findings of Song et al. [31], because the potential reason might be that infants get less iodine from breast milk as they get older [32], and some parents believe that salt should be avoided in supplement food for infants [33]. Results of this study on the effects of different feeding methods at different ages on infant iodine deficiency showed that the iodine deficiency rate of infants with mixed feeding at 0–3 months was significantly higher than that of infants with breastfeeding and mixed feeding, while there was no difference in the distribution of iodine deficiency in other ages. This is consistent with other research finding that formula-fed infants are more likely to develop iodine deficiency than breastfed infants [34, 35]. In addition, the protective effect of breastfeeding against iodine deficiency in infants aged 0–3 months is more pronounced, possibly because of the gradual introduction of complementary foods at 4–6 months.
Since March 2012, Henan Province has implemented the national food safety standard “Iodine content in Edible Salt,” and the iodized salt concentration has been adjusted from the original (35 ± 15) mg/kg to 30 mg/kg ± 30% [13]. According to the survey results from 2012 to 2019, the median urine iodine of breastfeeding women and infants aged 0–2 years in Zhengzhou has reached the appropriate iodine level every year, maintaining the elimination of iodine deficiency disease. In this study, the correlation analysis of urine iodine concentration of breastfed infants and their mothers showed that there was a significant positive correlation between the urine iodine concentration of breastfeeding mothers and infants, which was consistent with the results of some studies [1, 24, 36, 37]. The results showed that the iodine nutritional status of breastfeeding mothers could reflect the iodine nutritional status of infants.
However, there are still some limitations in this study. Firstly, the lack of 24 h urine iodine data from key participants involved in the study. Iodine nutritional status is considered to be most closely estimated by the amount of iodine excreted in urine over 24 h [38]. Secondly, due to the lack of iodine deficiency data of breastfeeding women and infants aged 0–2 years in Zhengzhou before 2012, the trend of UIC after the implementation of the new national salt iodine standard was not compared. In addition, we did not investigate the use of iodine supplements in lactating women and could not rule out the effect of iodine supplements on UIC. In future studies, we need to use a generalized linear logistic regression model to further explore the multivariate effects of dietary habits of iodine intake, the use of iodine supplements, and geographical location on iodine deficiency.
In conclusion, our study shows that after the implementation of the new national standard of iodine in edible salt, the iodine deficiency of breastfeeding women in Zhengzhou is gradually reduced, while the iodine deficiency of infants still needs to be improved by measures, and there is a significant positive correlation between the UIC of breastfeeding mothers and infants. In the future, in addition to the continuous implementation of the national salt iodization strategy, more efforts are urgently needed, such as strengthening iodine nutrition monitoring among key populations and paying attention to behavioral intervention with iodine supplementation among key populations, so as to improve the iodine deficiency situation among them.
Data Availability
For raw data for this study, please contact the corresponding author.
References
Pal N, Samanta SK, Chakraborty A, Chandra NK, Chandra AK (2018) Interrelationship between iodine nutritional status of lactating mothers and their absolutely breast-fed infants in coastal districts of Gangetic West Bengal in India. Eur J Pediatr 177(1):39–45. https://doi.org/10.1007/s00431-017-3025-6
Bilek R, Dvorakova M, Grimmichova T, Jiskra J (2020) Iodine, thyroglobulin and thyroid gland. Physiol Res 69(Suppl 2):S225–S36. https://doi.org/10.33549/physiolres.934514
Zimmermann MB (2016) The importance of adequate iodine during pregnancy and infancy. World Rev Nutr Diet 115:118–124. https://doi.org/10.1159/000442078
Wang Z, Liu P, Su X, Zou S, Song J, Liu S (2018) A comparison of iodine status in children and pregnant women after a policy change in the iodized salt standard in Shanghai. China Biol Trace Elem Res 185(2):275–281. https://doi.org/10.1007/s12011-018-1257-6
Pearce EN (2014) Iodine deficiency in children. Endocr Dev 26:130–138. https://doi.org/10.1159/000363160
Delange F, Bürgi H, Chen ZP, Dunn JT (2002) World status of monitoring iodine deficiency disorders control programs. Thyroid 12(10):915–924. https://doi.org/10.1089/105072502761016557
Zhao M, Li K, Wei J, Li W, Zhai G (2011) Analysis of iodine deficiency disorders surveillance in Zhengzhou, Henan province in 2010. Chin J Endemiol 30:84–5
Wang Z, Xing M, Zhu W, Mao G, Mo Z, Wang Y, Chen Z, Lou X, Xia S, Wang X (2018) Iodine deficiency in Zhejiang pregnant women in the context of universal Salt iodization programme. Sci Rep 8(1):8835. https://doi.org/10.1038/s41598-018-26942-z
Yang J, Zhu L, Li X, Zheng H, Wang Z, Liu Y, Hao Z (2016) Iodine status of vulnerable populations in Henan province of China 2013–2014 after the implementation of the new iodized salt standard. Biol Trace Elem Res 173(1):7–13. https://doi.org/10.1007/s12011-016-0619-1
Liu P, Fan L, Meng F, Su X, Liu S, Shen H, Sun D (2020) Prevention and control of iodine deficiency disorders— China, 1995–2020. China CDC Weekly 2(20):345. https://doi.org/10.3760/cma.j.issn.2095-4255.2013.05.015
Li WH, Dong BS, Li P, Li YF (2012) Benefits and risks from the national strategy for improvement of iodine nutrition: a community-based epidemiologic survey in Chinese schoolchildren. Nutrition 28(11–12):1142–1145. https://doi.org/10.1016/j.nut.2012.04.014
Zheng H, Li X, Yang J, Wang C, Sun N, Wang Y (2013) Current status of iodine deficiency disorders in Henan Province in 2011. Chin J Endemiol 32(526–528). https://doi.org/10.3760/cma.j.issn.2095-4255.2013.05.015
Ministry of Health of the People’s Republic of China (2011) GB 26878–2011 National Standards for Food safety - Iodine content of edible salt. Standards Press of China, Beijing
Wu Y, Li X, Chang S, Liu L, Zou S, Hipgrave DB (2012) Variable iodine intake persists in the context of universal salt iodization in China. J Nutr 142(9):1728–1734. https://doi.org/10.3945/jn.112.157982
Ding X, Han C, Sun X (2021) Surveillance results of iodine nutrition among key population in Kunshan, Jiangsu from 2016 to 202. Henan J Prev Med 32(11):840–2+64. https://doi.org/10.13515/j.cnki.hnjpm.1006-8414.2021.11.011
Chen A, Wang J, Han S, Yu L (2021) Monitoring of iodized salt and analysis of iodine nutritional status of key population in Ningxia in 2019. Ningxia Med J 43(10):889–91. https://doi.org/10.13621/j.1001-5949.2021.10.0889
Du D, Ren H, Liu B, Li X, Li X, Wang Q, Li Y (2021) Monitoring results of iodine nutrition level in different populations in Beijing from 2016 to 2019. J Prev Med Inf 37(09):1189–1193
Cao X, Jiang X, Dou Z, Rakeman MA, Zhang M, O’Donnell K, Ma T, Kareem A, Delong N, Delong GR (1994) Timing of vulnerability of the brain to iodine deficiency in endemic cretinism. N Engl J Med 331(26):1739–1744. https://doi.org/10.1056/NEJM199412293312603
Bougma K, Aboud FE, Harding KB, Marquis GS (2013) Iodine and mental development of children 5 years old and under: a systematic review and meta-analysis. Nutrients 5(4):1384–1416. https://doi.org/10.3390/nu5041384
Holla-Bhar R, Iellamo A, Gupta A, Smith JP, Dadhich JP (2015) Investing in breastfeeding - the world breastfeeding costing initiative. Int Breastfeed J 10:8. https://doi.org/10.1186/s13006-015-0032-y
Semba RD, Delange F (2001) Iodine in human milk perspectives for infant health. Nutr Rev(1):269–8. https://doi.org/10.1111/j.1753-4887.2001.tb05512.x
Zhang L, Sun YN, Li YM, Lin LX, Ye Y, Yan YQ, Chen ZP (2011) Effect of different iodine nutrition on cerebellum Pcp-2 in rat offspring during lactation. Biol Trace Elem Res 143(3):1629–1639. https://doi.org/10.1007/s12011-011-8991-3
Nazeri P, Shariat M, Azizi F (2021) Effects of iodine supplementation during pregnancy on pregnant women and their offspring: a systematic review and meta-analysis of trials over the past 3 decades. Eur J Endocrinol 184(1):91–106. https://doi.org/10.1530/EJE-20-0927
Du C, Wang C, Zhang Y, Fan L, Wang W, Chen W, Shen J, Zhang W (2018) The iodine status of lactating women and the influence on infants in Tianjin City. J Hyg Res 47(4):543–7. https://doi.org/10.19813/j.cnki.weishengyanjiu.2018.04.008
Yan Y, Zhang Y, Liu L (2006) Method for determination of iodine in urine by AS3+-Ce4+ catalytic spectrophotometry. Beijing: Health Standard of China WS/T 107–2006
World Health Organization United Nations Children’s Fund, International Council for the Control of Iodine Deficiency Disorders (2007) Assessment of iodine deficiency disorders and monitoring their elimination. Geneva: A guide for programme managers, 3rd edn
Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine-deficiency disorders. The Lancet 372(9645):1251–1262. https://doi.org/10.1016/s0140-6736(08)61005-3
Geng G, Lyu Q, Qin W, Xu Y, Chen S (2015) Monitoring analysis and validation of the method of urine iodine level in 400 children 8–10 years old. Modern Prev Med 42(01):49–50+75
Olivieri A, Trimarchi F, Vitti P (2020) Global iodine nutrition 2020: Italy is an iodine sufficient country. J Endocrinol Invest 43(11):1671–1672. https://doi.org/10.1007/s40618-020-01402-6
Wang Y, Ge P, Ma Q, Cao Y, Li H, Zheng J, Shi W, Sun W (2012) Study on the relationship between iodine nutrition and growth and development during the critical period of infant brain development. Chin J Epidemiol (02):164–167
Song L, Ma G, Su L, Yang S (2017) Analysis of iodine nutritional status and its influencing factors of infants at 0–2 years old in Anyang city. Chin J Child Health Care 25(06):601–603
Wang W, Sun Y, Zhang M, Y Z, W C, L T, J S, Z Z, S L, W Z (2018) Breast milk and infant iodine status during the first 12 weeks of lactation in Tianjin City, China. Asia Pac J Clin Nutr 27(2):393-8https://doi.org/10.6133/apjcn.062017.03
Klerks M, Roman S, Bernal MJ, Haro-Vicente JF, Sanchez-Siles LM (2021) Complementary feeding practices and parental pressure to eat among Spanish infants and toddlers: a cross-sectional study. Int J Environ Res Public Health 18(4):1982. https://doi.org/10.3390/ijerph18041982
Dumrongwongsiri O, Chatvutinun S, Phoonlabdacha P, Sangcakul A, Chailurkit LO, Siripinyanond A, Suthutvoravut U, Chongviriyaphan N (2018) High urinary iodine concentration among breastfed infants and the factors associated with iodine content in breast milk. Biol Trace Elem Res 186(1):106–113. https://doi.org/10.1007/s12011-018-1303-4
Smyth P, Hetherton A, Smith D, Radcliff M, O’Herlihy C (1997) Maternal iodine status and thyroid volume during pregnancy: correlation with neonatal iodine intake. J Clin Endocrinol Metab 82(9):2840–2843. https://doi.org/10.1210/jcem.82.9.4203
Nazeri P, Dalili H, Mehrabi Y, Hedayati M, Mirmiran P, Azizi F (2018) Is there any difference between the iodine statuses of breast-fed and formula-fed infants and their mothers in an area with iodine sufficiency? Br J Nutr 119(9):1012–1018. https://doi.org/10.1017/S0007114518000351
Chen Y, Gao M, Bai Y, Hao Y, Chen W, Cui T, Guo W, Pan Z, Lin L, Wang C, Shen J, Zhang W (2020) Variation of iodine concentration in breast milk and urine in exclusively breastfeeding women and their infants during the first 24 wk after childbirth. Nutrition 71:110599. https://doi.org/10.1016/j.nut.2019.110599
Soldin O (2002) Controversies in urinary iodine determinations. Clin Biochem 35(8):575–579. https://doi.org/10.1016/s0009-9120(02)00406-x
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. XYW and JHL contributed equally as the first authors of this manuscript. JHL, WXL, WHJ, and QZL contributed to the formulation of the question under investigation, the conception of the study, and design and data acquisition. XYW contributed to the analysis, interpretation, and drafting of the manuscript. S.S.T and QJL contributed to the critical revision of the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This is an observational study. The Medical Ethics Committee of Zhengzhou Center for Disease Control and Prevention has confirmed that no ethical approval is required.
Consent to Participate
Written informed consent was obtained from all mothers.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Liu, J., Lu, W. et al. Iodine Deficiency of Breastfeeding Mothers and Infants from 2012 to 2019 in Zhengzhou, China. Biol Trace Elem Res 201, 4298–4306 (2023). https://doi.org/10.1007/s12011-022-03531-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03531-w