Abstract
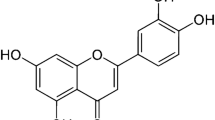
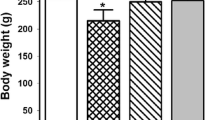
This study aimed to explore protective efficacy of Athelia rolfsii exopolysaccharides (AEPS) to mice kidney against lead-exposed injury with a focus on the role of nuclear factor erythroid-2-related factor 2 (Nrf2) signaling pathway. Lead accumulation in the kidney induces oxidative stress which causes low antioxidant activity, abnormal pathological changes, and apoptosis. Here, the changes in lead levels in the kidney and whole blood proved that AEPS inhibited lead accumulation. It might be related to AEPS enhancing glutathione (GSH) levels and glutathione-s-transferase (GST) activities, as well as the protein abundances of multidrug resistance–associated protein 1 (MRP1) and multidrug resistance–associated protein 2 (MRP2). Moreover, AEPS increased antioxidant activity by upregulating superoxide dismutase (SOD), catalase (CAT) activities, downregulating malondialdehyde (MDA) levels. It also restored kidney function by decreasing blood urea nitrogen (BUN) and creatinine (CRE) levels in the serum. Histopathologic analysis showed that AEPS alleviated the kidney injury induced by lead, too. AEPS also showed anti-apoptosis effect by downregulating caspase-3 and bax expression and upregulating bcl-2 expression. Importantly, AEPS activated Nrf2 signaling pathway by promoting nuclear translocation of Nrf2. However, all-trans-retinoic acid (ATRA), an Nrf2 inhibitor, reversed the effects on AEPS to activation of Nrf2, enhancement of antioxidant, alleviation of kidney injury, restoration of kidney function, prevention of apoptotic, and facilitation of lead exclusion. In brief, AEPS showed kidney protective effect and facilitated lead-expulsion in an Nrf2-dependent manner.








Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gottesfeld P, Pokhrel AK (2011) Review: Lead exposure in battery manufacturing and recycling in developing countries and among children in nearby communities. J Occup Environ Hyg 8(9):520–532. https://doi.org/10.1080/15459624.2011.601710
Martinez-Finley EJ, Chakraborty S, Fretham SJB, Aschner M (2012) Cellular transport and homeostasis of essential and nonessential metals. Metallomics 4(7):593–605. https://doi.org/10.1039/c2mt00185c
Amin I, Hussain I, Rehman MU, Mir BA, Ahmad P (2020) Zingerone prevents lead-induced toxicity in liver and kidney tissues by regulating the oxidative damage in Wistar rats. J Food Biochem 45(3):13241. https://doi.org/10.1111/jfbc.13241
Kaur I, Behl T, Aleya L, Rahman MH, Kumar A, Arora S, Akter R (2021) Role of metallic pollutants in neurodegeneration: effects of aluminum, lead, mercury, and arsenic in mediating brain impairment events and autism spectrum disorder. Environ Sci Pollut Res 28(8):8989–9001. https://doi.org/10.1007/s11356-020-12255-0
Jiang X, Xing X, Zhang Y, Zhang C, Wu Y, Chen Y, Meng R, Jia H, Cheng Y, Zhang Y, Su J (2021) Lead exposure activates the Nrf2/Keap1 pathway, aggravates oxidative stress, and induces reproductive damage in female mice. Ecotoxicol Environ Saf 207:111231. https://doi.org/10.1016/j.ecoenv.2020.111231
Cai SZ, Zhao LN, Liu J, Ji YT, Che Y (2019) Allicin alleviates lead-induced hematopoietic stem cell aging by upregulating PKM2. Biosci Rep 39(7):BSR20190243. https://doi.org/10.1042/BSR20190243
Roy A, Kordas K (2016) The relation between low-level lead exposure and oxidative stress: a review of the epidemiological evidence in children and non-occupationally exposed adults. Curr Environ Health Rep 3(4):478–492. https://doi.org/10.1007/s40572-016-0115-y
Chen Y, Feng X, Hu X, Sha J, Li B, Zhang H, Fan H (2018) Dexmedetomidine ameliorates acute stress-induced kidney injury by attenuating oxidative stress and apoptosis through inhibition of the ROS/JNK signaling pathway. Oxid Med Cell Longev 2018:4035310. https://doi.org/10.1155/2018/4035310
Zhang DD, Lo SC, Cross JV, Templeton DJ, Hannink M (2004) Keap1 is a redox-regulated substrate adaptor protein for a Cul3-dependent ubiquitin ligase complex. Mol Cell Biol 24(24):10941–10953. https://doi.org/10.1128/MCB.24.24.10941-10953.2004
Tong KI, Katoh Y, Kusunoki H, Itoh K, Tanaka T, Yamamoto M (2006) Keap1 recruits Neh2 through binding to ETGE and DLG motifs: characterization of the two-site molecular recognition model. Mol Cell Biol 26(8):2887–2900. https://doi.org/10.1128/MCB.26.8.2887-2900.2006
Song Y, Sun H, Gao S, Tang K, Zhao Y, Xie G, Gao H (2020) Saikosaponin a attenuates lead-induced kidney injury through activating Nrf2 signaling pathway. Comp Biochem Physiol C: Toxicol Pharmacol 242:108945. https://doi.org/10.1016/j.cbpc.2020.108945
Chen C, Han X, Wang G, Liu D, Bao L, Jiao C, Luan J, Hou Y, Xu Y, Wang H, Zhang Q, Zhou H, Fu J, Pi J (2021) Nrf2 deficiency aggravates the kidney injury induced by subacute cadmium exposure in mice. Arch Toxicol 95(3):883–893. https://doi.org/10.1007/s00204-020-02964-3
Dong J, Li H, Min W (2018) Preparation, characterization and bioactivities of Athelia rolfsii exopolysaccharide-zinc complex (AEPS-zinc). Int J Biol Macromol 113:20–28. https://doi.org/10.1016/j.ijbiomac.2018.01.223
Li H, Wei M, Min W, Gao Y, Liu X, Liu J (2016) Removal of heavy metal ions in aqueous solution by exopolysaccharides from Athelia rolfsii. Biocatal Agric Biotechnol 6(28–32):13. https://doi.org/10.1016/j.bcab.2016.01.013
Li B, Li H, Gao Y, Fan C, Min W (2019) Inhibitory effect of Athelia rolfsii exopolysaccharides on organ damage in lead-exposed Kunming strain mice. Food Funct 10(2):1159–1166. https://doi.org/10.1039/c8fo02558d
Zhai Q, Liu Y, Wang C, Qu D, Zhao J, Zhang H, Tian F, Chen W (2019) Lactobacillus plantarum CCFM8661 modulates bile acid enterohepatic circulation and increases lead excretion in mice. Food Funct 10(3):1455–1464. https://doi.org/10.1039/c8fo02554a
Wang Z, Yan Y, Yu X, Li W, Li B, Qin C (2015) Protective effects of chitosan and its water-solublederivatives against lead-induced oxidative stress in mice. Int J Biol Macromol 83:442–449. https://doi.org/10.1016/j.ijbiomac.2015.10.017
Yang W, Tian ZK, Yang HX, Feng ZJ, Sun JM, Jiang H, Cheng C, Ming QL, Liu CM (2019) Fisetin improves lead-induced neuroinflammation, apoptosis and synaptic dysfunction in mice associated with the AMPK/SIRT1 and autophagy pathway. Food Chem Toxicol 134:110824. https://doi.org/10.1016/j.fct.2019.110824
de Sousa RA, Sabarense CM, Prado GL, Metze K, Cadore S (2013) Lead biomonitoring in different organs of lead intoxicated rats employing GFAAS and different sample preparations. Talanta 104:90–96. https://doi.org/10.1016/j.talanta.2012.11.043
Liu P, Xue Y, Zheng B, Liang Y, Zhang J, Shi J, Chu X, Han X, Chu L (2021) Crocetin attenuates the oxidative stress, inflammation and apoptosis in arsenic trioxide-induced nephrotoxic rats: implication of PI3K/AKT pathway. Int Immunopharmacol 88:106959. https://doi.org/10.1016/j.intimp.2020.106959
Ko JW, Shin NR, Jung TY, Shin IS, Moon C, Kim SH, Lee IC, Kim SH, Yun WK, Kim HC, Kim JC (2019) Melatonin attenuates cisplatin-induced acute kidney injury in rats via induction of anti-aging protein, Klotho. Food Chem Toxicol 129:201–210. https://doi.org/10.1016/j.fct.2019.04.049
Lin X, Yang F, Huang J, Jiang S, Tang Y, Li J (2020) Ameliorate effect of pyrroloquinoline quinone against cyclophosphamideinduced nephrotoxicity by activating the Nrf2 pathway and inhibiting the NLRP3 pathway. Life Sci 256:117901. https://doi.org/10.1016/j.lfs.2020.117901
Lee JS, Surh YJ (2005) Nrf2 as a novel molecular target for chemoprevention. Cancer Lett 224(2):171–184. https://doi.org/10.1016/j.canlet.2004.09.042
Yong L, Li Q, WanY CZ (2011) MRP proteins as potential mediators of heavy metal resistance in zebrafish cells. Comp Biochem Physiol C: Toxicol Pharmacol 153(3):310–317. https://doi.org/10.1016/j.cbpc.2010.12.001
Zalups RK, Joshee L, Bridges CC (2014) Novel Hg2+-induced nephropathy in rats and mice lacking Mrp2: evidence of axial heterogeneity in the handling of Hg2+ along the proximal tubule. Toxicol Sci 142(1):250–260. https://doi.org/10.1093/toxsci/kfu171
Yong L, Li Q, Cui Z (2011) Molecular analysis and heavy metal detoxification of ABCC1/MRP1 in zebrafish. Mol Biol Rep 38(3):1703–1711. https://doi.org/10.1007/s11033-010-0283-z
Ajsuvakova OP, Tinkov AA, Aschner M, Rocha JBT, Bjrklund G (2020) Sulfhydryl groups as targets of mercury toxicity. Coord Chem Rev 417:213343. https://doi.org/10.1016/j.ccr.2020.213343
Devóz PP, Reis MBD, Gomes WR, Maraslis FT, Ribeiro DL, Antunes LMG, Batista BL, Grotto D, Reis RM, Barbosa FJ, Barcelos GRM (2020) Adaptive epigenetic response of glutathione (GSH)-related genes against lead (Pb)-induced toxicity, in individuals chronically exposed to the metal. Chemosphere 269:128758. https://doi.org/10.1016/j.chemosphere.2020.128758
Kirtane AJ, Leder DM, Waikar SS, Chertow GM, Ray KK, Pinto DS, Karmpaliotis D, Burger AJ, Murphy SA, Cannon CP (2005) Serum blood urea nitrogen as an independent marker of subsequent mortality among patients with acute coronary syndromes and normal to mildly reduced glomerular filtration rates. J Am Coll Cardiol 45(11):1781–1786. https://doi.org/10.1016/j.jacc.2005.02.068
Paithankar JG, Saini S, Dwivedi S, Sharma A, Chowdhuri DK (2020) Heavy metal associated health hazards: an interplay of oxidative stress and signal transduction. Chemosphere 262:128350. https://doi.org/10.1016/j.chemosphere.2020.128350
Ighodaro OM, Akinloye OA (2017) First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): their fundamental role in the entire antioxidant defence grid. Alex J Med. https://doi.org/10.1016/j.ajme.2017.09.001
Giuseppina B, Stefania P, Martina D, Chiara D, Alessia A, Paolo CG, Giulio G, Angele CM, Maria G, Fabrizio G (2018) Lipid peroxidation-derived aldehydes, 4-hydroxynonenal and malondialdehyde in aging-related disorders. Antioxidants 7(8):102. https://doi.org/10.3390/antiox7080102
Mas-Bargues C, Escrivá C, Dromant M, Borrás C, Viña J (2021) Lipid peroxidation as measured by chromatographic determination of malondialdehyde. Human plasma reference values in health and disease. Arch Biochem Biophys 709:108941. https://doi.org/10.1016/j.abb.2021.108941
Simon HU, Haj-Yehia A, Levi-Schaffer F (2000) Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis 5(5):415–418. https://doi.org/10.1023/a:1009616228304
D’Arcy MS (2019) Cell death: a review of the major forms of apoptosis, necrosis and autophagy. Cell Biol Int 43(6):582–592. https://doi.org/10.1002/cbin.11137
Xu X, Lai Y, Hua Z (2018) Apoptosis and apoptotic body: disease message and therapeutic target potentials. Biosci Rep 39(1):BSR20180992. https://doi.org/10.1042/BSR20180992
Cory S, Adams JM (2002) The Bcl2 family: regulators of the cellular life-or-death switch. Nat Rev Cancer 2(9):647–656. https://doi.org/10.1038/nrc883
Hou G, Surhio MM, Ye H, Gao X, Ye Z, Li J, Ye M (2018) Protective effects of a Lachnum polysaccharide against liver and kidney injury induced by lead exposure in mice. Int J Biol Macromol 124:716–723. https://doi.org/10.1016/j.ijbiomac.2018.11.133
Bradberry S, Vale A (2009) A comparison of sodium calcium edetate (edetate calcium disodium) and succimer (DMSA) in the treatment of inorganic lead poisoning. Clin Toxicol 47(9):841–858. https://doi.org/10.3109/15563650903321064
Rajak C, Singh N, Parashar P (2020) Metal toxicity and natural antidotes: prevention is better than cure. Environ Sci Pollut Res 27(35):43582–43598. https://doi.org/10.1007/s11356-020-10783-3
Wang Y, Fang J, Huang S, Chen L, Fan G, Wang C (2012) The chronic effects of low lead level on the expressions of Nrf2 and Mrp1 of the testes in the rats. Environ Toxicol Pharmacol 35(1):109–116. https://doi.org/10.1016/j.etap.2012.12.001
Li H, Lan T, Yun C, Yang K, Du Z, Luo X, Hao E, Deng J (2020) Mangiferin exerts neuroprotective activity against lead-induced toxicity and oxidative strevss ia Nrf2 pathway. Chin Herb Med 12(1):36–46. https://doi.org/10.1016/j.chmed.2019.12.002
Piet B, Raymond E, Marcel K, Jan W (2000) A family of drug transporters: the multidrug resistance-associated proteins. J Natl Cancer Inst 92(16):1295–1302. https://doi.org/10.1093/jnci/92.16.1295
Okada K, Shoda J, Taguchi K, Maher JM, Ishizaki K, Inoue Y, Ohtsuki M, Goto N, Takeda K, Utsunomiya H, Oda K, Warabi E, Ishii T, Osaka K, Hyodo I, Yamamoto M (2008) Ursodeoxycholic acid stimulates Nrf2-mediated hepatocellular transport, detoxification, and antioxidative stress systems in mice. Am J Physiol-Gastrointest Liver Physiol 295(4):735–747. https://doi.org/10.1152/ajpgi.90321.2008
Ibbotson K, Yell J, Ronaldson PT (2017) Nrf2 signaling increases expression of ATP-binding cassette subfamily C mRNA transcripts at the blood-brain barrier following hypoxia-reoxygenation stress. Fluids Barriers CNS 14(1):6. https://doi.org/10.1186/s12987-017-0055-4
Hazelhoff MH, Torres AM (2018) Gender differences in mercury-induced hepatotoxicity: potential mechanisms. Chemosphere Environ Toxicol Risk Assess 202:330–338. https://doi.org/10.1016/j.chemosphere.2018.03.106
Leslie EM, Deeley RG, Cole SPC (2005) Multidrug resistance proteins: role of P-glycoprotein, MRP1, MRP2, and BCRP (ABCG2) in tissue defense. Toxicol Appl Pharmacol 204(3):216–237. https://doi.org/10.1016/j.taap.2004.10.012
Kala SV, Neely MW, Kala G, Prater CI, Atwood DW, Rice JS, Lieberman MW (2000) The MRP2/cMOAT transporter and arsenic-glutathione complex formation are required for biliary excretion of arsenic. J Biol Chem 275(43):33404–33408. https://doi.org/10.1074/jbc.M007030200
Vernhet L, Allain N, Payen L, Anger JP, Guillouzo A, Fardel O (2001) Resistance of human multidrug resistance-associated protein 1-overexpressing lung tumor cells to the anticancer drug arsenic trioxide 1. Biochem Pharmacol 61(11):1387–1391. https://doi.org/10.1016/s0006-2952(01)00606-2
Valenzuela M, Glorieux C, Stockis J, Sid B, Sandoval JM, Felipe KB, Kviecinski MR, Verrax J, Calderon PB (2014) Retinoic acid synergizes ATO-mediated cytotoxicity by precluding Nrf2 activity in AML cells. Br J Cancer 111(5):874–882. https://doi.org/10.1038/bjc.2014.380
Author information
Authors and Affiliations
Contributions
We would like to thank all participants involved in this study. Pan Zhao designed experiments, carried out the experiments, and prepared the manuscript. Hongmei Li supervised the manuscript and revised the final version of the manuscript. ZhiChao Wang carried out the experiments. Weihong Min and Yawen Gao supervised the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The experiment procedures were approved by the guidelines of the Jilin Agricultural University Institutional Animal Care and Use Committee (Jilin, China) (approval number: 2021 04 13 001).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Disclaimer
All authors have read the manuscript and agreed to submit it in its current form for consideration for publication in the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, P., Li, H., Wang, Z. et al. Athelia rolfsii Exopolysaccharide Protection Against Kidney Injury in Lead-Exposed Mice via Nrf2 Signaling Pathway. Biol Trace Elem Res 201, 1864–1877 (2023). https://doi.org/10.1007/s12011-022-03287-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03287-3