Abstract
Background
Severe iodine deficiency during gestation is associated with adverse pregnancy outcomes; however, the impact of mild-to-moderate iodine deficiency, though prevalent in pregnancy, remains unclear.
Methods
We extracted follow-up data for 7435 pregnant women from a national iodine deficiency disorders monitoring program from 2016 to 2018 and a mother–child cohort study in 2017 based on a birth registry in Shanghai. Birth outcomes were collected from the registry. Spot urine and household salt samples were collected for iodine testing. Single-factor analysis and logistic regression were used to evaluate the association between maternal iodine status and pregnancy outcomes.
Results
The median urine iodine level in pregnant women was 137.5 μg/L (interquartile range 82.4–211.5), suggesting mild deficiency according to WHO standards. The incidence of pregnancy termination, preterm birth, congenital malformations, low birth weight, and cesarean section was 3.2%, 4.3%, 1.4%, 2.7%, and 45.2% in the mildly iodine-deficient group and 3.4%, 4.5%, 1.4%, 2.7%, and 44.5% in the normal group, respectively. After adjusting for maternal age and education, trimesters, and preterm birth rate in the general population, the odds ratios for any outcome did not differ significantly between the two groups.
Conclusion
The present study suggests that mild maternal iodine deficiency is not associated with adverse pregnancy outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iodine is an essential micronutrient for the human body. It is an important element in the synthesis of thyroid hormone, which is closely related to growth, nervous system development, and substance metabolism throughout the body [1]. Fetal demands for iodine must all come from the mother; thus, the iodine status of pregnant women has a direct influence on fetal growth and development [2]. The World Health Organization (WHO) recommends using the median urinary iodine concentration (UIC) to assess iodine status in populations. Based on the recommended criteria of iodine deficiency in pregnancy population by WHO [3] and other published criteria [4], iodine deficiency is defined as a median UIC < 150 μg/L (subcategorized as severe < 50 μg/L, moderate 50–99 μg/L, or mild100–149 μg/L). Populations are considered iodine sufficient with a median UIC of 150–249 μg/L, iodine excess at median UIC of 250–499 μg/L, or severe excess at median UIC of > 500 μg/L.
Since the implementation of the global salt iodization program in 1990, approximately 70% of the world’s households consume iodized salt. Universal salt iodization regulations were established in 1996 in China, with the standards for edible salt iodine content adjusted three times. As a result, the iodine intake of the general population is adequate [5], although mild iodine deficiency may be present in pregnant women [6,7,8,9].
Iodine deficiency during pregnancy can affect maternal thyroid function and pregnancy outcome as well as fetal growth and development. Severe iodine deficiency during pregnancy carries risks for the mother, including miscarriage, placental abruption, and stillbirth [10], as well as for the child, including cretinism, cognitive, and psychological defects, deafness, and thyroxin-related nerve damage [11,12,13]. However, the effects of mild-to-moderate iodine deficiency during pregnancy are controversial. Some studies have shown that it can lead to maternal and fetal thyroid dysfunction; however, it is not clear whether there is damage to the baby’s cognitive and neurological functions [14]. In contrast, a study found no association between mild-to-moderate maternal iodine deficiency and adverse pregnancy outcomes [15]. Daily iodine supplementation for mildly iodine-deficient pregnant women had no effect on neurodevelopment in children at 5–6 years of age [16]. An Indian study suggested that in areas where the general population has adequate iodine intake, mild-to-moderate maternal iodine deficiency has a limited impact on the offspring’s development [17]. However, some studies have found it to be associated with attention-deficit hyperactivity disorder [18] and cognitive dysfunction [19, 20] in children.
The increase in maternal blood volume during pregnancy may lead to a decrease in the concentration of nutrients, in turn resulting in a decline in urine concentration. Therefore, some have hypothesized that maternal iodine deficiency during pregnancy is a physiologic change, just like physiological anemia resulting from a decrease in hemoglobin concentration during pregnancy. In animal experiments, the placenta was found to be iodine-rich, and mild maternal iodine deficiency did no harm to the offspring [21,22,23,24]. Therefore, there is concern that oversupplementation with iodine during pregnancy may induce a state of excess iodine in some women, which could adversely affect fetal thyroid function, causing neonatal hypothyroidism [25,26,27].
Thus, the association between mild-to-moderate maternal iodine deficiency and pregnancy outcomes warrants further study. Over the past 4 years (2015–2018), the iodine status and pregnancy outcomes of women in Shanghai were monitored to investigate this question. In this study, we tested the association between urine iodine concentrations in pregnant women and pregnancy outcomes, including pregnancy termination, preterm birth, neonatal malformation, low birth weight, neonatal overweight, and a low Apgar score.
Materials and Methods
Study Design and Participants
This study included women in two cohort studies who had lived for over 1 year in the regions investigated and who had no recorded health problems including (1) heavy mental illness, hepatitis in the infected period, active tuberculosis, HIV infected, and other infectious diseases; (2) dementia and deaf-mute disabilities; (3) bedridden or activity limited; and (4) other diseases may disturb the study. All participants should comply with the inclusion and exclusion criteria and confirm written consent. The two studies were the national iodine deficiency disease (IDD) monitoring program from 2016 to 2018 and a cohort study evaluating the association between iodine status and offspring health in 2017. Both surveys were approved by the Medical Ethics Committee of Shanghai Municipal Center for Disease Prevention and Control and were aimed to continuously surveil participants’ iodine status via urine samples and family salt usage and include information on demography, lifestyle, medical history, and pregnancy as well as birth conditions in overall the same format. We aimed to detect the association between iodine status during pregnancy and gestational outcome. In each sampling unit, more than 20 pregnant women at different trimesters in each year were randomly recruited for a urine iodine test. At the same time, a household salt sample was collected from each woman’s home to test iodine content. A total of 4938 pregnant women were followed in the IDD monitoring program from 2016 to 2018. In the 2017 cohort study, complete follow-up data from 4805women and their offsprings were available.
Sample Size
We calculated the sample size for logistic regression of a binary response variable (Y), which was mainly based on the following parameters: power, alpha (significance level), P0 (baseline probability that Y = 1), odds ratio (OR, Odds1/Odds0), and R-squared of X1 with other Xs. Preterm birth was set as the response variable (Y) and urine iodine status was set as the main independent variable (X). It was reported by the Shanghai Center for Women and Children’s Health that the preterm birth rate in general newborns of Shanghai was 5.53%(28) in 2016, which determined the value of P0. R-squared of X1 with other Xs was set at 0.0114 according to the results of the linear regression between maternal urine iodine status and potential confounders including maternal education, age, and trimesters. The power analysis for logistic regression was set for both-sided tests and main parameters including power, alpha, and OR which was set as 0.90, 0.05, and 0.7, respectively. According to the final results, the least sample size requires 1599 participants for the logistic regression analysis.
Flowchart of the Study
Of the 9743 pregnant women eligible for the present study, we excluded those who were lost to follow-up or for whom information on UIC or neonatal outcome was incomplete (n = 1437), women who delivered outside of Shanghai (n = 478), those with twins or triplets (n = 125), or those who had pregnancy termination prior to study entry (n = 268). Finally, 7435 women with full information on iodine nutrition and pregnancy and neonatal outcomes were included in the analysis (Fig. 1).
Evaluating Method and Criteria of Obstetric Outcomes
All women were face-to-face or telephonic interviewed during the pregnancy or after birth through the Shanghai birth registry, and then, details of obstetric outcome were extracted from hospital records following delivery. The mother’s age and education, whether the pregnancy was terminated, the mode of delivery, gestational weeks, congenital malformations, birth weight, birth length, and Apgar score were recorded.
The modes of delivery were reported as natural birth, cesarean delivery, forceps, fetal suction, and breech presentation. Preterm delivery was defined as birth before 37 completed weeks of gestation, whether by spontaneous onset of labor or iatrogenic delivery. Birth weight was categorized as low (< 2500 g), normal (2500–4000 g), or overweight (> 4000 g). The Apgar score is based on five physical signs in the neonate, including heart rate, respiration, muscle tone, laryngeal reflex, and skin color assessed at 1, 5, and 10 minutes after birth. The score was used to judge the presence and severity of neonatal asphyxia. An Apgar score of 8–10 points was defined as asphyxia free, 4–7 points as mild asphyxia, and 0–3 points as severe asphyxia. Because there were relatively few neonates with scores of 0–3 or 4–7, we combined those two groups and included a low Apgar score (< 8) in the logistic regression model. The incidence of each pregnancy outcome was analyzed according to UIC levels.
Methods of Sampling and Testing and Evaluation Criteria of Urinary Iodine and Salt Iodine
The participants’ urine samples were collected at the community health service center on the day of the enrollment investigation. The participants discharge part of their urine first and then use a urine cup to collect mid-section urine for about 20 mL. The remaining urine can be discharged without collection, then transfer the urine sample from the urine cup to the urine collection tube, and tightly closed the tube cover. After collection, we temporarily store samples at 4 °C and – 80 °C for the long term. The iodine concentration of the spot urine sample was determined using the acid digestion method (As3 + -Ce4 + catalytic spectrophotometry) in the Shanghai Municipal Center for Disease Prevention and Control. Internal quality control samples for UIC were provided by the Chinese National Iodine Deficiency Disorders Reference Laboratory.
The iodine status of the pregnant women in the study was determined by the recommended WHO/UNICEF/ICCIDD criteria from 2007 [3] and other published criteria [17]. UIC of < 50 μg/L was considered severe insufficient: UIC of 50 to 100 μg/L moderate insufficient; UIC of 100 to150 mild insufficient; UIC of 150 to 249 μg/L adequate, UIC of > 250 μg/L greater than requirements or excessive.
Participants were required to take at least 20 g of the household salt sample using the light-proof sealed bag given by the investigators 3 days prior to the enrollment investigation. The iodine content of the household edible salt samples was determined by the direct titration method. According to the standard of edible salt iodine content of 30 mg/kg ± 30%, salt iodine content < 5 mg/kg was defined as non-iodized, 21 to 39 mg/kg as qualified or adequately iodized, and 5 to < 21 mg/kg or > 39 mg/kg as unqualified or inadequately iodized.
Statistical Analysis
Continuous data are presented as median (interquartile range) and categorical data as number (percentage). UIC was not normally distributed, and differences between groups were therefore compared using a nonparametric test (Mann–Whitney U test). Additionally, since UICs were stratified into five groups as described above, chi-square tests and Fisher exact probability method were used when comparing UIC groups with the presence or absence of pregnancy outcomes. One-way analysis of variance was used to compare continuous data among the UIC groups. For data that were not normally distributed, the Kruskal–Wallis H test was used. Logistic regression was used to examine the association between maternal iodine status and the likelihood of adverse pregnancy outcomes, with the adequate UIC group as the reference.
Statistical significance was at the 0.05 level, and odds ratios (ORs) and 95% confidence intervals were calculated accordingly. All analyses were conducted using IBM SPSS Statistics version 21.0(IBM Corp., Armonk, NY, USA).
Results
Characteristic of the Study Population
The median age of the 7435 pregnant women was 29 (27 ~ 32) years. The median UIC was 137.5 (82.4–211.5) μg/L, with values of 137.3, 134.9, and 141.4 μg/L obtained in the first, second, or third trimester, respectively. These were all considered mildly deficient according to WHO standards. Iodized salt was found in 74.4% of the Shanghai households and qualified iodized salt in 60.1%. A total of 44.9% of the deliveries were by cesarean section, while 45.1% were vaginal, including natural, forceps, suction, or breech.
Among the 7435 women in the cohort, the median UIC was < 50 μg/L in 872 (11.7%), 50–99.9 μg/L in 1600 (21.5%), 100–149.9 μg/L in 1669 (22.5%), 150–249.9 μg/L in 1987 (26.7%), and > 250 μg/L in 1307 (17.6%) (Table 1).
Obstetric Outcomes
During the study period, 3.5% of the pregnant women underwent pregnancy termination. The incidence of preterm birth was 4.1%, and cesarean deliveries were performed in 44.9%. Among the neonates, 1.3% showed congenital malformations, 2.4% were underweight, and 5.9% were overweight. Among full-term infants, 0.8% showed low birthweight, which was significantly lower than that in the entire cohort. Apgar scores at 1, 5, and 10 min, respectively, were 1–3 in 0.11%, 0.03%, and 0.02%; 4–7 in 0.99%, 0.13%, and 0.11%; and 8–10 in 98.90%, 99.84%, and 99.87%, respectively (Table 2). Among the full-term newborns, the median weight was 3350.0 (3075.0–3620.0) g and median length 50.0 (50.0–50.0) cm (Table 3).
Adverse Pregnancy Outcomes According to Maternal Urinary Iodine
The pregnant women were divided into four age groups, and then, the incidence of adverse obstetric outcomes in each group was compared according to five UIC levels. There were no significant differences among the five UIC groups in terms of Apgar scores or the incidence of preterm births, cesarean deliveries, congenital malformations, underweight, or overweight (Table 2).
To exclude the influence of preterm birth, 7312 cases of full-term birth were reanalyzed based on the mothers’ age groups. The low birth weight incidence and the newborns’ weights and lengths were compared according to UIC levels. Again, none of the groups differed significantly (Tables 2 and 3).
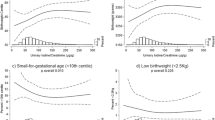
Logistic Regression Analysis
We calculated ORs of adverse pregnancy outcomes including preterm birth, congenital malformations, low birthweight, overweight, cesarean delivery, and low Apgar scores among the UIC groups with models adjusting for the confounders of mother’s age and education and the trimester when the urine samples were collected. When assessing low birthweight, the model was also adjusted for preterm birth. None of the adjusted ORs differed significantly for any of the adverse outcomes (Table 4).
Discussion
In this study, we found that mild iodine deficiency in pregnant women was not associated with an adverse pregnancy outcome including pregnancy termination, preterm birth, congenital malformations, low birth weight, or overweight.
Because of increased thyroid hormone synthesis, transfer of iodine to the fetus, and increased glomerular filtration rates resulting in increased passive loss of iodine in the urine, pregnant women require a higher iodine intake than non-pregnant women [29, 30]. We found that many pregnant women in Shanghai were in the state of mild iodine deficiency according to the current WHO standard. However, we did not find any adverse maternal or neonatal outcomes associated with this deficiency. According to the published incidence of congenital hypothyroidism (CH) in newborns in Shanghai, it has been a relatively low level at 32.50 per 100,000 people from 1997 to 2007 [31, 32], which is lower than that in China at 49.2 per 100,000 people from 1985 to 2006 [33]. This is consistent with our findings, supporting our contention that mild gestational iodine deficiency does no harm to mothers or their newborns. Another study reported that daily iodine supplementation in women with mild iodine deficiency had no effect on their children’s neurodevelopment assessed at the age of 5 or 6 years [18]. Therefore, iodine supplements should not automatically be prescribed for pregnant women just because the population is mildly iodine deficient, particularly when the safe upper limit of iodine intake for pregnant women is unknown.
Both iodine deficiency and excess have been posited to be associated with adverse effects on thyroid function since iodine is an essential constituent of thyroid hormones [34]. However, most individuals reportedly tolerate high exposure to iodine or compensate for mild-to-moderate iodine deficiency by means of homeostatic mechanisms [35]. There is evidence that maintaining an adequate iodide supply for the developing fetus is dependent on both maternal dietary iodine intake and placental iodide transport. Pregnancy-associated hormones, particularly oxytocin and human chorionic gonadotropin, help promote placental iodide uptake, which may protect the fetus against iodine deficiency [24]. The results of our study show that mild maternal iodine deficiency is not associated with adverse pregnancy outcomes, suggesting that unlike the thyroid and brain, maternal and fetal placental tissues are not particularly sensitive to minor perturbations in iodine availability and can therefore continue to function normally in pregnancy. The effects of iodine deficiency might also be compensated for by the population-wide improvement in nutritional status as living standards have improved.
We found no association between different maternal UICs and pregnancy outcomes, consistent with a British study that also found no significant difference in the incidence of preterm delivery and mode of delivery among groups based on the urinary iodine-to-creatinine ratio [15]. A study in Spain demonstrates that birthweight was associated with maternal iodine status. They found neonates born to women with a third trimester UIC between 100 μg/L and 149 μg/L were less likely to be small for gestational age than those born to women with a UIC of below 50 μg/L [36]. This study provides side proof to the minor severity of health risks due to mild iodine deficiency and also hints that severe iodine deficiency may be more likely to be associated with adverse birth outcomes than mild or moderate iodine deficiency. However, our findings contradict those of a study in Thailand in which the rates of preterm birth and low birthweight were significantly higher in women with iodine deficiency. They found that iodine status was an independent risk factor for preterm birth and low birthweight [37]. Given these conflicting results, the true association between the iodine status of pregnant women and neonatal outcomes requires further study.
Some recent studies have suggested that mild maternal iodine deficiency may be associated with a low IQ, poor language development [38,39,40], or attention-deficit hyperactivity disorder [41] in their children. Another study has reported that iodine deficiency might adversely affect women’s fertility [42]. The reasons for these discrepancies are unclear. However, different confounders related to iodine deficiency may affect pregnancy outcomes in different settings.
The main advantages of our study are the robust evidence derived from a large sample size of pregnant women and their newborns that were followed up in the IDD monitoring program, which supports the strength of our findings. However, one limitation of this study is the limited number of covariates considered. In addition, the use of only one urinary iodine measurement to classify iodine status may not represent a woman’s iodine status throughout pregnancy [43]. Therefore, there may have been some misclassification, which could mask possible differences between groups. Besides, because the incidence of some adverse pregnancy outcomes in this study was very low, the study may have been underpowered to detect differences for those outcomes. At last, Shanghai is an environmentally iodine-deficient area, but due to the sufficient intake of iodine-rich seafood as well as the iodized salt, and the high overall dietary quality of the population, the overall iodine level of the population in Shanghai is appropriate. Therefore, mild to moderate iodine deficiency of pregnant women in Shanghai may have a limited impact on pregnancy and birth outcomes. However, in other areas where iodine is deficient in the environment and the population’s overall intake of iodine and dietary quality is insufficient or in certain areas with high iodine level in the environment, the study’s results may be less applicable.
Conclusions
Mild maternal iodine deficiency is not associated with adverse pregnancy outcomes and may not be a threat to pregnancy outcomes.
Data Availability
Restrictions apply to the availability of data generated or analyzed during this study to preserve patient confidentiality or because they were used under license. The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.
Code Availability
Not applicable.
References
Pearce EN (2018) Iodine nutrition: recent research and unanswered questions. Eur J Clin Nutr 72:1226–1228
Xia L, Yu Y, Qin X, Chen Y (2015) Correlation study between pregnant women urine iodine content and thyroid dysfunction during pregnancy. Journal of Guiyang Medical College 40:863–866
WHO (2007) Assessment of iodine deficiency disorders and monitoring their elimination A guide for programme managers, 3rd ed [WH Organization, edito. Geneva, Switzerland.
Mills JL, Ali M, Louis GMB, Kannan K, Weck J, Wan Y, Maisog J, Giannakou A, Sundaram R (2019) Pregnancy loss and iodine status: the LIFE prospective cohort study. Nutrients 3:E534
Pearce EN, Andersson M, Zimmermann MB (2013) Global iodine nutrition: Where do we stand in 2013? Thyroid 23:523–528
Zang J, Zhou J, Zou S, Wang Z, Cheng Y, Zhu Z, Jia X, Guo C (2017) Comprehensive assessment on iodine nutrition and dietary iodine intake_x000a_among Shanghai residents. Shanghai Journal of Preventive Medicine 29:417–422
Zhao J, Li W, Guo Y, Sun H, Feng B, Yang L (2019) Analysis of iodine nutrition level of population after three adjustment of iodized salt concentration in Jilin province. Chinese Journal of Control of Endemic Disenaces 34:41–42
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, Grobman WA, Laurberg P, Lazarus JH, Mandel SJ, Peeters RP, Sullivan S (2017) 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 27:315–389
Caldwell KL, Pan Y, Mortensen ME, Makhmudov A, Merrill L, Moye J (2013) Iodine status in pregnant women in the National Children’s Study and in U.S. women (15–44 years), National Health and Nutrition Examination Survey 2005–2010. Thyroid 23:927–937
Zimmermann MB (2009) Iodine deficiency in pregnancy and the effects of maternal iodine supplementation on the offspring: a review. Am J Clin Nutr 89:668S-672S
Pearce EN (2012) Effects of iodine deficiency in pregnancy. JOURNAL OF TRACE ELEMENTS IN MEDICINE AND BIOLOGY 2–3:131–133
Melse-Boonstra A, Mackenzie I (2013) Iodine deficiency, thyroid function and hearing deficit a review. Nutr Res Rev 2:110–117
Skeaff SA (2011) Iodine deficiency in pregnancy the effect on neurodevelopment in the child. Nutrients 2:265–273
Zimmermann MB (2016) The Importance of Adequate Iodine during Pregnancy and Infancy. World Rev Nutr Diet 115:118–124
Torlinska B, Bath SC, Janjua A, Boelaert K & Chan SY (2018) Iodine status during pregnancy in a region of mild-to-moderate iodine deficiency is not associated with adverse obstetric outcomes; results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Nutrients 10.
Gowachirapant S, Jaiswal N, Melse-Boonstra A, Galetti V, Stinca S, Mackenzie I, Thomas S, Thomas T, Winichagoon P, Srinivasan K, Zimmermann MB (2017) Effect of iodine supplementation in pregnant women on child neurodevelopment: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 5:853–863
Lean MI, Lean ME, Yajnik CS, Bhat DS, Joshi SM, Raut DA, Lubree HG, Combet E (2014) Iodine status during pregnancy in India and related neonatal and infant outcomes. Public Health Nutr 17:1353–1362
Vermiglio F, Lo PV, Moleti M, Sidoti M, Tortorella G, Scaffidi G, Castagna MG, Mattina F, Violi MA, Crisa A, Artemisia A, Trimarchi F (2004) Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. J Clin Endocrinol Metab 89:6054–6060
Hynes KL, Otahal P, Hay I, Burgess JR (2013) Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort. J Clin Endocrinol Metab 98:1954–1962
Bath SC, Steer CD, Golding J, Emmett P, Rayman MP (2013) Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 382:331–337
Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, O’Heir CE, Mitchell ML, Hermos RJ, Waisbren SE, Faix JD, Klein RZ (1999) Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med 341:549–555
Lazarus JH, Bestwick JP, Channon S, Paradice R, Maina A, Rees R, Chiusano E, John R, Guaraldo V, George LM, Perona M, Dall’Amico D, Parkes AB, Joomun M & Wald NJ, (2012) Antenatal thyroid screening and childhood cognitive function. N Engl J Med 366:493–501
Li H, Richard K, McKinnon B, Mortimer RH (2007) Effect of iodide on human choriogonadotropin, sodium-iodide symporter expression, and iodide uptake in BeWo choriocarcinoma cells. J Clin Endocrinol Metab 92:4046–4051
Burns R, O’Herlihy C, Smyth PP (2013) Regulation of iodide uptake in placental primary cultures. Eur Thyroid J 2:243–251
Connelly KJ, Boston BA, Pearce EN, Sesser D, Snyder D, Braverman LE, Pino S, LaFranchi SH (2012) Congenital hypothyroidism caused by excess prenatal maternal iodine ingestion. J Pediatr 161:760–762
Kurtoglu S, Akin L, Akin MA, Coban D (2009) Iodine overload and severe hypothyroidism in two neonates. J Clin Res Pediatr Endocrinol 1:275–277
Weber G, Vigone MC, Rapa A, Bona G, Chiumello G (1998) Neonatal transient hypothyroidism: aetiological study. Italian Collaborative Study on Transient Hypothyroidism. Arch Dis Child Fetal Neonatal Ed 79:F70–F72
Liyun HE, Li D, Hui J, Shuang L, Liping Z (2020) The occurrence and risk factors of preterm birth in Shanghai city. Chinese Journal of Woman and Child Health Research 31:706–711
Glinoer D (2007) The importance of iodine nutrition during pregnancy. Public Health Nutr 10:1542–1546
Dafnis E, Sabatini S (1992) The effect of pregnancy on renal function: physiology and pathophysiology. Am J Med Sci 303:184–205
Tian G, Xu H, Zhu W, Guan Y & Wang Y (2007) Report on 20 years neonatal screening for congenital hypothyroidism and phenyletonuria. SHANGHAI JOURNAL OF PREVENTIVE MEDICINE 5.
Tian G (2008) Study on the screening of congenital hypothyroidism in newborns in Shanghai and the incidence trend., Shanghai Jiao Tong University.
Xu Y, Qin Y & Zhao Z (2009) Retrospective study on neonatal screening for congenital hypothyroidism and phenylketonuria in China in the past 22 years. Chinese Journal of Pediatrics, 18–22.
Pearce EN (2018) Iodine nutrition: recent research and unanswered questions. Eur J Clin Nutr 72:1226–1228
Zimmermann M, Delange F (2004) Iodine supplementation of pregnant women in Europe: a review and recommendations. Eur J Clin Nutr 58:979–984
Alvarez-Pedrerol M, Guxens M, Mendez M, Canet Y, Martorell R, Espada M, Plana E, Rebagliato M, Sunyer J (2009) Iodine levels and thyroid hormones in healthy pregnant women and birth weight of their offspring. Eur J Endocrinol 160:423–429
Charoenratana C, Leelapat P, Traisrisilp K, Tongsong T (2016) Maternal iodine insufficiency and adverse pregnancy outcomes. Matern Child Nutr 12:680–687
Bath SC, Steer CD, Golding J, Emmett P, Rayman MP (2013) Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 382:331–337
Hynes KL, Otahal P, Hay I, Burgess JR (2013) Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort. J Clin Endocrinol Metab 98:1954–1962
Abel MH, Caspersen IH, Meltzer HM, Haugen M, Brandlistuen RE, Aase H, Alexander J, Torheim LE, Brantsaeter AL (2017) Suboptimal maternal iodine intake is associated with impaired child neurodevelopment at 3 years of age in the Norwegian Mother and Child Cohort Study. J Nutr 147:1314–1324
Abel MH, Ystrom E, Caspersen IH, Meltzer HM, Aase H, Torheim LE, Askeland RB, Reichborn-Kjennerud T & Brantsaeter AL (2017) Maternal iodine intake and offspring attention-deficit/hyperactivity disorder: results from a large prospective cohort study. Nutrients 9.
Mills JL, Buck LG, Kannan K, Weck J, Wan Y, Maisog J, Giannakou A, Wu Q, Sundaram R (2018) Delayed conception in women with low-urinary iodine concentrations: a population-based prospective cohort study. Hum Reprod 33:426–433
Zimmermann MB, Andersson M (2012) Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev 70:553–570
Acknowledgements
We are grateful to the pregnant women and the healthcare professionals who participated in this study.
Funding
The current study was financially supported by key disciplines in the three-year Plan of Shanghai municipal public health system (2020–2022) (GWV-10.1-XK11), academic leader in the three-year Plan of Shanghai municipal public health system (2020–2022) (GWV-10.2-XD18) and outstanding young Talents in the three-year Plan of Shanghai municipal public health system (2020–2022) (GWV-10.3-YQ22) and Top Young Talents in Shanghai (No. 2020-8). None of the funders played a role in the study design, data analysis, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jiajie Zang; methodology: Changyi Guo and Jiajie Zang; formal analysis: Xueying Cui, Huiting Yu, and Zhengyuan Wang; investigation: Huiting Yu, Zhengyuan Wang, Hai Wang, Zehuan Shi, Wei Jin, Qi Song, and Hongmei Tang; data curation, Xueying Cui, Huiting Yu, and Zhengyuan Wang; writing—original draft preparation: Xueying Cui, Huiting Yu, and Zhengyaun Wang; writing—review & editing: Xueying Cui, Huiting Yu, Zhengyaun Wang, and Jaijie Zang; funding acquisition: Jiajie Zang and Zhengyuan Wang. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The survey protocol was approved by the Medical Ethics Committee of Shanghai Municipal Center for Disease Control and Prevention.
Consent to Participate
Written informed consent was obtained from all of the participants.
Consent for Publication
All authors were approved of the publication of this manuscript.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cui, X., Yu, H., Wang, Z. et al. No Association Was Found Between Mild Iodine Deficiency During Pregnancy and Pregnancy Outcomes: a Follow-up Study Based on a Birth Registry. Biol Trace Elem Res 200, 4267–4277 (2022). https://doi.org/10.1007/s12011-021-03028-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-03028-y