Abstract
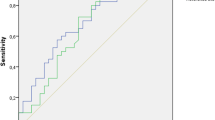
Determination of the copper content in the saliva of breast cancer patients was carried out to assess the potential diagnostic and prognostic value. The malignant group included 75 breast cancer patients; the benign group included 87 patients with fibroadenomas; and the control group included 20 volunteers without breast pathology. All participants had 1 ml of saliva collected prior to treatment. The determination of copper in saliva was carried out by the stripping voltammetric method. Overall survival was assessed using the Kaplan-Meier method with the presentation of survival curves and the calculation of the significance of differences by Log-rank. The average copper content in the saliva of breast cancer patients is 49.3% higher than in patients with fibroadenomas and 60.4% higher than in volunteers without breast pathologies. Within the group of breast cancer patients, the content of copper in saliva is heterogeneous, which limits the possibilities of using this indicator for diagnostic purposes. The copper content increases when comparing the initial stages and locally widespread (+ 22.4%) and then sharply increases by 3.5 times at the T3-4N0-2M0 stage. For HER2-positive breast cancer, the copper content in saliva is 51.9% higher than for HER2-negative, a similar pattern was observed for luminal A and B breast cancer subtypes. The content of copper in saliva less than 1.14 mg/l is a prognostically unfavorable sign, while the relative risk of dying from breast cancer more than doubles. Thus, the content of copper in saliva can be used in clinical practice for planning treatment tactics.


Similar content being viewed by others
References
Freitas I, Boncompagni E, Vaccarone R, Fenoglio C, Barni S, Baronzio GF (2007) Iron accumulation in mammary tumor suggests a tug of war between tumor and host for the microelement. Anticancer Res 27(5):3059–3066
Giri S, Singh AK (2015) Human health risk assessment via drinking water pathway due to metal contamination in the groundwater of Subarnarekha River Basin, India. Environ Monit Assess 187(3):63–69. https://doi.org/10.1007/s10661-015-4265-4
Valco M, Rhodes CJ, Moncol J, Izakovic M, Mazur M (2006) Free radicals metals and antioxidants in oxidative stress induced cancer. Chem Biol Interact 160(1):1–40. https://doi.org/10.1016/j.cbi.2005.12.009
Balsano C, Porcu C, Sideria S (2018) Is copper a new target to counteract the progression of chronic diseases? Metallomics 10(12):1712–1722. https://doi.org/10.1039/C8MT00219C
Mendoza M, Caltharp S, Song M, Collin L, Konomi JV, McClain CJ, Vos MB (2017) Low hepatic tissue copper in pediatric non-alcoholic fatty liver disease. J Pediatr Gastroenterol Nutr 65(1):89–92. https://doi.org/10.1097/MPG.0000000000001571
Meyer M (2019) Processing of collagen based biomaterials and the resulting materials properties. Biomed Eng Online 18:24. https://doi.org/10.1186/s12938-019-0647-0
Bhattacharya PT, Misra SR, Hussain M (2016) Nutritional aspects of essential trace elements in oral health and disease: an extensive review. Scientifica (Cairo):5464373. https://doi.org/10.1155/2016/5464373
Wolonciej M, Milewska E, Roszkowska-Jakimiec W (2016) Trace elements as an activator of antioxidant enzymes. Advances in hygiene and experimental medicine. Postepy Hig Med Dosw 70:1483–1498. https://doi.org/10.5604/17322693.1229074
Lutsenko S (2016) Copper trafficking to the secretory pathway. Metallomics. 8(9):840–852. https://doi.org/10.1039/C6MT00176A
Vetchy MPJVKKD (2018) Biological role of copper as an essential trace element in the human organism. Ceska Slov Farm 67(4):143–153
Shibazaki S, Uchiyama S, Tsuda K, Taniuchi N (2017) Copper deficiency caused by excessive alcohol consumption. BMJ Case Rep 2017:bcr-2017-220921. https://doi.org/10.1136/bcr-2017-220921
Morrell A, Tallino S, Yu L, Burkhead JL (2017) The role of insufficient copper in lipid synthesis and fatty-liver disease. IUBMB Life 69(4):263–270. https://doi.org/10.1002/iub.1613
Fukai T, Ushio-Fukai M, Kaplan JH (2018) Copper transporters and copper chaperones: roles in cardiovascular physiology and disease. Am J Phys Cell Phys 315:186–201. https://doi.org/10.1152/ajpcell.00132.2018
Marques CMS, Nunes EA, Lago L, Pedron CN, Manieri TM, Sato RH, Oliveira VX, Cerchiaro G (2017) Generation of advanced glycation end-products (AGEs) by glycoxidation mediated by copper and ROS in a human serum albumin (HSA) model peptide: reaction mechanism and damage in motor neuron cells. Mutat Res 824:42–51. https://doi.org/10.1016/j.mrgentox.2017.10.005
Shi Y, Wang R, Yuan W, Liu Q, Shi M, Feng W, Wu Z, Hu K, Li F (2018) Easy-to-use colorimetric cyanine probe for the detection of Cu2+ in Wilson's disease. ACS Appl Mater Interfaces 10(24):20377–20386. https://doi.org/10.1021/acsami.8b07081
Hordyjewska A, Popiołek L, Kocot J (2014) The many “faces” of copper in medicine and treatment. Biometals. 27(4):611–621. https://doi.org/10.1007/s10534-014-9736-5
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Global Burden of Disease Cancer Collaboration Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability and disability-adjusted life-years for 29 cancer groups, 1990 to 2017. A Systematic analysis for the global burden of disease study. JAMA Oncol 2019:1749–1768. https://doi.org/10.1001/jamaoncol.2019.2996
Kolyadina IV, Poddubnaya IV, Frank GA, Komov DV, Karseladze AI, Yermilova VD et al (2015) Stage I breast cancer heterogeneity: biological and prognostic significance. Malignant Tumors 1:31–40
Porto-Mascarenhas EC, Assad DX, Chardin H, Gozal D, Canto GDL, Acevedo AC et al (2017) Salivary biomarkers in the diagnosis of breast cancer: a review. Critical reviews in oncology. Hematology. 110:62–73. https://doi.org/10.1016/j.critrevonc.2016.12.009
Kaczor-Urbanowicz KE, Wei F, Rao SL, Kim J, Shin H, Cheng J, Tu M, Wong DTW, Kim Y (2019) Clinical validity of saliva and novel technology for cancer detection. BBA Rev Cancer 1872:49–59. https://doi.org/10.1016/j.bbcan.2019.05.007
Zhang L, Xiao H, Karlan S, Zhou H, Gross J, Elashoff D et al (2010) Discovery and preclinical validation of salivary transcriptomic and proteomic biomarkers for the non-invasive detection of breast cancer. PLoS One 5(12):15573. https://doi.org/10.1371/journal.pone.0015573
Cheng F, Wang Z, Huang Y, Duan Y, Wang X (2015) Investigation of salivary free amino acid profile for early diagnosis of breast cancer with ultra-performance liquid chromatography-mass spectrometry. Clin Chim Acta 447:23–31. https://doi.org/10.1016/j.cca.2015.05.008
Takayama T, Tsutsui H, Shimizu I, Toyama T, Yoshimoto N, Endo Y, Inoue K, Todoroki K, Min JZ, Mizuno H, Toyo'oka T (2016) Diagnostic approach to breast cancer patients based on target metabolomics in saliva by liquid chromatography with tandem mass spectrometry. Clin Chim Acta 452:18–26. https://doi.org/10.1016/j.cca.2015.10.032
Liu X, Yu H, Qiao Y, Yang J, Shu J, Zhang J, Zhang Z, He J, Li Z (2018) Salivary glycopatterns as potential biomarkers for screening of early-stage breast cancer. EBioMedicine. 28:70–79. https://doi.org/10.1016/j.ebiom.2018.01.026
Murata T, Yanagisawa T, Kurihara T, Kaneko M, Ota S, Enomoto A, Tomita M, Sugimoto M, Sunamura M, Hayashida T, Kitagawa Y, Jinno H (2019) Salivary metabolomics with alternative decision tree-based machine learning methods for breast cancer discrimination. Breast Cancer Res Treat 177:591–601. https://doi.org/10.1007/s10549-019-05330-9
Pereira JAM, Taware R, Porto-Figueira P, Rapole S, Câmara JS (2020) The salivary volatome in breast cancer, precision medicine for investigators. Pract Provide:301–306. https://doi.org/10.1016/B978-0-12-819178-1.00029-0
López-Jornet P, Aznar C, Ceron JJ, Tvarijonaviciute A (2021) Salivary biomarkers in breast cancer: a cross-sectional study. Support Care Cancer 29:889–896. https://doi.org/10.1007/s00520-020-05561-3
Assad DX, Mascarenhas ECP, de Lima CL, de Toledo IP, Chardin H, Combes A, Acevedo AC, Guerra ENS (2020) Salivary metabolites to detect patients with cancer: a systematic review. Int J Clin Oncol 25(6):1016–1036. https://doi.org/10.1007/s10147-020-01660-7
Yang J, Liu X, Shu J, Hou Y, Chen M, Yu H, Ma T, du H, Zhang J, Qiao Y, He J, Niu L, Yang F, Li Z (2020) Abnormal galactosylated–glycans recognized by Bandeiraea Simplicifolia Lectin I in saliva of patients with breast cancer. Glycoconj J 37:373–394. https://doi.org/10.1007/s10719-020-09910-6
Ilić IR, Stojanović NM, Radulović NS, Živković VV, Randjelović PJ, Petrović AS et al (2019) The Quantitative ER immunohistochemical analysis in breast cancer: detecting the 3 + 0, 4 + 0, and 5 + 0 Allred score cases. Medicina (Kaunas) 55(8):461. https://doi.org/10.3390/medicina55080461
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P, Hanna W, Jenkins RB, Press MF, Spears PA, Vance GH, Viale G, McShane LM, Dowsett M (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol 36(20):2105–2122. https://doi.org/10.1200/JCO.2018.77.8738
Bel’skaya LV, Kosenok VK, Sarf EA (2017) Chronophysiological features of the normal mineral composition of human saliva. Arch Oral Biol 82:286–292. https://doi.org/10.1016/j.archoralbio.2017.06.024
Jakmunee J, Junsomboon J (2008) Determination of cadmium, lead, copper and zinc in the acetic acid extract of glazed ceramic surfaces by anodic stripping voltammetric method. Talanta. 77(1):172–175. https://doi.org/10.1016/j.talanta.2008.06.003
Nizamani P, Afridi HI, Kazi TG, Talpur FN, Baig JA (2019) Essential trace elemental levels (zinc, iron and copper) in the biological samples of smoker referent and pulmonary tuberculosis patients. Toxicol Rep 6:1230–1239. https://doi.org/10.1016/j.toxrep.2019.11.011
Marín-Martínez L, Molino-Pagán D, López-Jornet P (2019) Trace elements in saliva and plasma of patients with type 2 diabetes: association to metabolic control and complications. Diabetes Res Clin Pract 157:107871. https://doi.org/10.1016/j.diabres.2019.107871
Lan X, Chan JYK, Pu JJ, Qiao W, Pang S, Yang W-F, Wong KCW, Kwong DLW, Su Y-X (2020) Saliva electrolyte analysis and xerostomia-related quality of life in nasopharyngeal carcinoma patients following intensity-modulated radiation therapy. Radiother Oncol 150:97–103. https://doi.org/10.1016/j.radonc.2020.06.016
Wang D, Du X, Zheng W (2008) Alteration of saliva and serum concentrations of manganese, copper, zinc, cadmium and lead among career welders. Toxicol Lett 176(1):40–47. https://doi.org/10.1016/j.toxlet.2007.10.003
Bel'skaya LV, Kosenok VK, Sarf EA, Titov AV (2014) Determination of copper and ceruloplasmin in saliva. Butlerov Commun 39(8):161–164
Vavilova TP, Gusarova YN, Koroleva OV, Medvedev AYE (2005) The role of ceruloplasmin in the development of neoplastic processes. Biomeditsinskaya khimiya 51(3):263–275
Alyasova AV, Kontorshchikova KN, Korkotoshvilli LV, Terent’yev IG (2009) Influence of antitumor treatment and ozone therapy on the parameters of lipid peroxidation and the concentration of some trace elements in the blood plasma of patients with breast cancer. Sovremennyye tekhnologii v meditsine 1:21–27
Zatulovskaia YA, Ilyechova EY, Puchkova LV (2015) The features of copper metabolism in the rat liver during development. PLoS One 10(10). https://doi.org/10.1371/journal.pone.0140797
Gaetke LM, Chow-Johnson HS, Chow CK (2014) Copper: toxicological relevance and mechanisms. Arch Toxicol 88(11):1929–1938. https://doi.org/10.1007/s00204-014-1355-y
Kumar H, Lim HW, More SV, Kim BW, Koppula S, Kim IS, Choi DK (2012) The Role of free radicals in the aging brain and Parkinson’s disease: convergence and parallelism. Int J Mol Sci 13(8):10478–10504. https://doi.org/10.3390/ijms130810478
Alkadi HA (2020) Review on free radicals and antioxidants. Infect Disord Drug Targets 20(1):16–26. https://doi.org/10.2174/1871526518666180628124323
Aliaga ME, López-Alarcón C, Bridi R, Speisky H (2016) Redox-implications associated with the formation of complexes between copper ions and reduced or oxidized glutathione. J Inorg Biochem 154:78–88. https://doi.org/10.1016/j.jinorgbio.2015.08.005
Boulet A, Vest KE, Maynard MK, Gammon MG, Russell AC, Mathews AT, Cole SE, Zhu X, Phillips CB, Kwong JQ, Dodani SC, Leary SC, Cobine PA (2018) The mammalian phosphate carrier SLC25A3 is a mitochondrial copper transporter required for cytochrome c oxidase biogenesis. J Biol Chem 293(6):1887–1896. https://doi.org/10.1074/jbc.RA117.000265
Djurdjevic P, Jakovljevic I, Joksovic L, Ivanovic N, Jelikic-Stankov M (2014) The effect of some fluoroquinolone family members on biospeciation of copper (II), nickel (II) and zinc (II) ions in human plasma. Molecules. 19(8):12194–12223. https://doi.org/10.3390/molecules190812194
Catalani S, Paganelli M, Gilberti ME, Rozzini L, Lanfranchi F, Lanfranchi F, Padovani A, Apostoli P (2018) Free copper in serum: an analytical challenge and its possible applications. J Trace Elem Med Biol 45:176–180. https://doi.org/10.1016/j.jtemb.2017.11.006
Cabrera A, Alonzo E, Sauble E, , Chu YL, Nguyen D, Linder MC, Sato DS, Mason AZ. Copper binding components of blood plasma and organs, and their responses to influx of large doses of 65 Cu, in the mouse. BioMetals. 2008; 21 (5): 525-543. https://doi.org/10.1007/s10534-008-9139-6
Bernevic B, El-Khatib AH, Jakubowski N, Weller MG (2018) Online immunocapture ICP-MS for the determination of the metalloprotein ceruloplasmin in human serum. BMC Res Notes 11:213. https://doi.org/10.1186/s13104-018-3324-7
Vashchenko G, MacGillivray RTA (2013) Multi-copper oxidases and human iron metabolism. Nutrients. 5(7):2289–2313. https://doi.org/10.3390/nu5072289
Adamczyk-Sowa M, Sowa P, Mucha S, Zostawa J, Mazur B, Owczarek M, Pierzchala K (2016) Changes in serum ceruloplasmin levels based on immunomodulatory treatments and melatonin supplementation in multiple sclerosis patients. Med Sci Monit 22:2484–2491. https://doi.org/10.12659/MSM.895702
Blockhuys S, Zhang X, Wittung-Stafshede P (2020) Single-cell tracking demonstrates copper chaperone Atox1 to be required for breast cancer cell migration. PNAS. 117(4):2014–2019. https://doi.org/10.1073/pnas.1910722117
Arredondo М, Nunez Н, Lopez G, Pizarro F, Ayala M, Araya M (2010) Influence of estrogens on copper indicators: in vivo and in vitro studies. Biol Trace Elem Res 134(3):252–264. https://doi.org/10.1007/s12011-009-8475-x
Ayala M, Pizarro F, Mendez MA, Arredondo M, Araya M (2008) Copper and liver function indicators vary depending on the female hormonal cycle and serum hormone binding globulin (SHBG) concentration in healthy women. Biol Trace Elem Res 121(1):9–15. https://doi.org/10.1007/s12011-007-8029-z
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was carried out in accordance with the Helsinki Declaration (adopted in June 1964 in Helsinki, Finland, and revised in October 2000 in Edinburgh, Scotland) and was approved at a meeting of the Ethics Committee of the Omsk Regional Clinical Hospital “Clinical Oncology Center” on July 21, 2016 (Protocol No. 15). All of the volunteers provided written informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bel’skaya, L.V., Sarf, E.A., Shalygin, S.P. et al. Potential Diagnostic Significance of Salivary Copper Determination in Breast Cancer Patients: A Pilot Study. Biol Trace Elem Res 200, 953–960 (2022). https://doi.org/10.1007/s12011-021-02710-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02710-5