Abstract
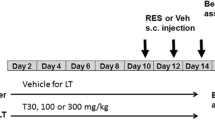
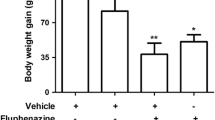
Reserpine administration results in a predictable animal model of orofacial dyskinesia (OD) that has been largely used to access movement disturbances related to extrapyramidal oxidative damage. Here, OD was acutely induced by reserpine (two doses of 0.7 mg/kg subcutaneous (s.c.)), every other day for 3 days), which was administered after (experiment 1) and before (experiment 2) magnesium (Mg) supplementation (40 mg/kg/mL, peroral (p.o.)). In experiment 1, Mg was administered for 28 days before reserpine treatment, while in experiment 2, it was initiated 24 h after the last reserpine administration and was maintained for 10 consecutive days. Experiment 1 (prevention) showed that Mg supplementation was able to prevent reserpine-induced OD and catalepsy development. Mg was also able to prevent reactive species (RS) generation, thus preventing increase of protein carbonyl (PC) levels in both cortex and substantia nigra, but not in striatum. Experiment 2 (reversion) showed that Mg was able to decrease OD and catalepsy at all times assessed. In addition, Mg was able to decrease RS generation, with lower levels of PC in both cortex and striatum, but not in substantia nigra. These outcomes indicate that Mg is an important metal that should be present in the diet, since its intake is able to prevent and minimize the development of movement disorders closely related to oxidative damage in the extrapyramidal brain areas, such as OD.





Similar content being viewed by others
References
Novick D, Haro JM, Bertsch J, Haddad PM (2010) Incidence of extrapyramidal symptoms and tardive dyskinesia in schizophrenia: thirty-six-month results from the European schizophrenia outpatient health outcomes study. J ClinPsychopharmacol 30:531–40. doi:10.1097/JCP.0b013e3181f14098
Bakker PR, de Groot IW, van Os J, van Harten PN (2011) Long-Stay psychiatric patients: a prospective study revealing persistent antipsychotic-induced movement disorder. PLoS One 6:1–6. doi:10.1371/journal.pone.0025588
Trevizol F, Benvegnú DM, Barcelos RCS et al (2011) Comparative study between two animal models of extrapyramidal movement disorders: prevention and reversion by pecan nut shell aqueous extract. Behav Brain Res 221:13–18. doi:10.1016/j.bbr.2011.02.026
Barcelos RCS, Benvegnu DM, Boufleur N et al (2011) Short term dietary fish oil supplementation improves motor deficiencies related to reserpine-induced Parkinsonism in rats. Lipids 46:143–149. doi:10.1007/s11745-010-3514-0
Bürger ME, Fachinetto R, Zeni G, Rocha JBT (2005) Ebselen attenuates haloperidol-induced orofacial dyskinesia and oxidative stress in rat brain. Pharmacol Biochem Behav 81:608–615. doi:10.1016/j.pbb.2005.05.002
Abílio VC, Araújo V, Bergamo M et al (2003) Vitamin E attenuates reserpine-induced Oral dyskinesia and striatal oxidized glutathione/reduced glutathione Ratio (GSSG/GSH) enhancement in rats. Prog Neuro Psychopharmacol 2:7109–7114. doi:10.1016/S0278-5846(02)00340-8
Bergamo M, Abílio VC, Queiroz CMT et al (1997) Effects of age on a new model of Tardive dyskinesia. Neurobiol Aging 18:623–629. doi:10.1016/S0197-4580(97)00152-8
Dutra RC, Andreazza AP, Andreatini ST, Vital MABF (2002) Behavioral effects of MK-801 on reserpine-treated mice. Prog Neuropsychopharmacol Biol Psychiatry 26:487–495. doi:10.1016/S0278-5846(01)00295-0
Raghavendra V, Naidu PS, Kulkarni SK (2001) Reversal of reserpine-induced vacuous chewing movements in rats by melatonin: involvement of peripheral benzodiazepine receptors. Brain Res 904:149–152. doi:10.1016/S0006-8993(01)02455-6
Silva RH, Abilio VC, Torres-Leite D et al (2002) Concomitant development of oral dyskinesia and memory deficits in reserpine-treated male and female mice. Behav Brain Res 132:171–177. doi:10.1016/S0166-4328(01)00409-0
Sussman AN, Trannguyen LTL, Neisewander JL (1997) Acute reserpine administration elicits long-term spontaneous oral dyskinesia. Eur J Pharmacol 337:157–160. doi:10.1016/S0014-2999(97)01271-5
Bürger ME, Alves A, Callegari L, Athayde FAR, Nogueira CW, Rocha JBT (2003) Ebselen attenuates reserpine-induced orofacial dyskinesia and oxidative stress in rat striatum. Prog Neuro Psychopharmacol 27:135–140. doi:10.1016/S0278-5846(02)00344-5
Neisewander JL, Castañeda E, Davisv DA (1994) Dose-dependent Differences in the development of reserpine-induced oral-dyskinesia in rats: support for a model of tardive dyskinesia. Psychopharmacology 116:79–84. doi:10.1007/BF02244874
Queiróz CMT, Frussa-Filho R (1999) Effects of buspirone on na animal model of tardive dyskinesia. Prog Neuro Psychopharmacol 23:1405–1418. doi:10.1016/S0278-5846(99)00074-3
Fuentes P, Paris I, Nassif M, Caviedes P, Segura-Aguilar J (2007) Inhibition of VMAT-2 and DT-diaphorase induce cell death in a substantia nigra-derived cell Line - An experimental cell model for dopamine toxicity studies. Chem Res Toxicol 20:776–783. doi:10.1021/tx600325u
Bilska A, Dubiela M, Sokołowska-Jez˙ewicz M et al (2007) Alpha-lipoic acid differently affects the reserpine-induced oxidative stress in the striatum and prefrontal cortex of rat brain. Neuroscience 146:1758–71. doi:10.1016/j.neuroscience.2007.04.002
Naidu PS, Singh A, Kulkarni SK (2004) Reversal of reserpine-induced orofacial dyskinesia and cognitive dysfunction by quercetin. Pharmacology 70:59–67. doi:10.1159/000074669
Lohr JB, Kuczenski R, Niculescu AB (2003) Oxidative mechanisms and tardive dyskinesia. CNS Drugs 17:47–62. doi:10.2165/00023210-200317010-00004
Teixeira AM, Reckziegel P, Müller L et al (2009) Intense exercise potentiates oxidative stress in striatum of reserpine-treated animals. Pharmacol Biochem Behav 92:231–235. doi:10.1016/j.pbb.2008.11.015
Fachinetto R, Villarinho JG, Wagner C et al (2007) Valerianaofficinalis does not alter the orofacial dyskinesia induced by haloperidol in rats: role of dopamine transporter. Prog Neuropsychopharmacol Biol Psychiatry 31:1478–86. doi:10.1016/j.pnpbp.2007.06.028
Reckziegel P, Dias VT, Benvegnú DM et al (2011) Locomotor damage and brain oxidative stress induced by lead exposure are attenuated by gallic acid treatment. Toxicol Lett 203:74–81. doi:10.1016/j.toxlet.2011.03.006
Ford ES, Mokdad AH (2003) Dietary magnesium intake in a national sample of US adults. J Nutr 133:2879–82
Kowal A, Panaszek B, Barg W, Obojski A (2007) The use of magnesium in bronchial asthma: a new approach to an old problem. Arch Immunol Ther Ex 55:35–9. doi:10.1007/s00005-007-0008-8
Porter NS, Jason LA, Boulton A, Bothne N, Coleman B (2010) Alternative medical interventions used in the treatment and management of myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia. J Altern Complement Med 16:235–49. doi:10.1089/acm.2008.0376
Soave PM, Conti G, Costa R, Arcangeli A (2009) Magnesium and anaesthesia. Curr Drug Targets 10:734–43. doi:10.2174/138945009788982487
Euser AG, Cipolla MJ (2009) Magnesium sulfate for the treatment of eclampsia. Stroke 40:1169–75. doi:10.1161/STROKEAHA.108.527788
Manrique AM, Arroyo M, Lin Y et al (2010) Magnesium supplementation during cardiopulmonary bypass to prevent junctional ectopic tachycardia after pediatric cardiac surgery: a randomized controlled study. J Thorac Cardiovasc Surg 139:162–9. doi:10.1016/j.jtcvs.2009.07.064
Saris NE, Mervaala E, Karppanen H et al (2000) Magnesium: an update on physiological, clinical and analytical aspects. Clin Chim Acta 294:1–26. doi:10.1016/S0009-8981(99)00258-2
Sabatier M, Arnaud MJ, Kastenmayer P, Rytz A, Barclay DV (2002) Meal effect on magnesium bioavailability from mineral water in healthy women. Am J Clin Nutr 75:65–71
Wolf FI, Cittadini A (2003) Chemistry and biochemistry of magnesium. Mol Asp Med 24:3–9. doi:10.1016/S0098-2997(02)00087-0
Barra A, Camardese G, Tonioni F et al (2007) Plasma magnesium level and psychomotor retardation in major depressed patients. Magnes Res 20:245–249. doi:10.1684/mrh.2007.0115
Vink R, Cook NL, van den Heuvel C (2009) Magnesium in acute and chronic brain injury: an update. Magnes Res 22:158–162. doi:10.1684/mrh.2009.0175
Hoane MR (2007) Assessment of cognitive function following magnesium therapy in the traumatically injured brain. Magnes Res 20:229–36. doi:10.1684/mrh.2007.0113
Hoane MR, Gilbert DR, Barbre AB, Harrison SA (2008) Magnesium dietary manipulation and recovery of function following controlled cortical damage in the rat. Magnes Res 21:29–37. doi:10.1684/mrh.2008.0128
Regan RF, Jasper E, Guo Y, Panter SS (1998) Effect of magnesium on oxidative neuronal injury in vitro. J Neurochem 70:77–85. doi:10.1046/j.1471-4159.1998.70010077.x
Ariza AC, Bobadilla N, Fernandez C et al (2005) Effects of magnesium sulfate on lipid peroxidation and blood pressure regulators in pre-eclampsia. Clin Biochem 38:128–33. doi:10.1016/j.clinbiochem.2004.09.018
Wolf FI, Trapani V, Simonacci M, Ferre S, Maier JAM (2008) Magnesium deficiency and endothelial dysfunction: is oxidative stress involved? Magnes Res 21:58–64. doi:10.1684/mrh.2008.0129
Turkoglu OF, Eroglu H, Okutan O et al (2008) A comparative study of treatment for brain edema Magnesium sulphate versus dexamethasone sodium phosphate. J Clin Neurosci 15:60–65. doi:10.1016/j.jocn.2007.03.005
Altura BM, Shah NC, Jiang X et al (2009) Short-term magnesium deficiency results in decreased levels of serum sphingomyelin, lipid peroxidation and apoptosis in cardiovascular tissues. Am J Physiol Heart C 297:86–92. doi:10.1152/ajpheart.01154.2008
Safar MM, Abdallah DM, Arafa NM, Abdel-Aziz MT (2010) Magnesium supplementation enhances the anticonvulsant potential of valproate in pentylenetetrazol-treated rats. Brain Res 1334:58–64. doi:10.1016/j.brainres.2010.03.076
Rocha JBT, Santos JET, Rocha LK, Kleinpaul ER (1997) Undernutrition during suckling changes the sensivity to haloperidol and chlorpromazine in two behavioural measures in weaning rats. Pharmacol Toxicol 80:114–123. doi:10.1111/j.1600-0773.1997.tb00040.x
Paxinos G, Watson C (2007) The rat brain in stereotaxic coordinates. Elsevier, Amsterdam
Hempel SL, Buettner GRO, Malley YQ, Wessels DA, Flaherty DM (1999) Dihydrofluo-resceindiacetate is superior for detecting intracellular oxidants: comparisonwith 2′, 7′-dichloro dihydrofluoresceindiacetate, 5 (and 6)- carboxy-2′, 7′-dichloro dihydrofluoresceindiacetate, and dihydrorhodamine. Free Radical Biol Med 27:146–59. doi:10.1016/S0891-5849(99)00061-1
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin–Phenol reagents. J Biol Chem 193:265–275
Levine RL, Williams JA, Stadtman ER, Shacter E (1994) Carbonyl assays for determination of oxidatively modified proteins. Method Enzymol 233:346–357. doi:10.1016/S0076-6879(94)33040-9
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358. doi:10.1016/0003-2697(79)90738-3
Lohr JB (1991) Oxygen radicals and neuropsychiatric illness: some speculations. Arch Gen Psychiatry 48:1097–1106. doi:10.1001/archpsyc.1991.01810360061009
Asanuma M, Miyazaki I, Ogawa N (2003) Dopamine- or L-DOPA-induced neurotoxicity: the role of dopamine quinone formation and tyrosinase in a model of Parkinson’s disease. Neurotox Res 5:165–176. doi:10.1016/j.febslet.2004.12.091
Asanuma M, Miyazaki I, Diaz-Corrales FJ, Ogawa N (2004) Quinone formation as dopaminergic neuron-specific oxidative stress in pathogenesis of sporadic Parkinson’s disease and neurotoxina-induced parkinsonismo. Acta Med Okayama 58:221–233
Naidu PS, Singh A, Kulkarni SK (2003) Quercetin, a bioflavonoid, attenuates haloperidol-induced orofacial dyskinesia. Neuropharmacology 44:1100–1106. doi:10.1016/S0028-3908(03)00101-1
Andreassen OA, Jorgensen HA (2000) Neurotoxicity associated with neuroleptic-induced oral dyskinesi as in rats. Implications for tardive dyskinesia. Prog Neurobiol 61:525–541. doi:10.1016/S0301-0082(99)00064-7
Faria RR, Abílio VC, Grassl C et al (2005) Beneficial effects of vitamin C and vitamin E on reserpine-induced oral dyskinesia in rats: critical role of striatal catalase activity. Neuropharmacology 48:993–1001. doi:10.1016/S0301-0082(99)00064-7
Peroza LR, Busanello A, Leal CQ et al (2013) Bauhinia forficata prevents vacuous chewing movements induced by haloperidol in rats and has antioxidant potential in vitro. Neurochem Res 38:789–796. doi:10.1007/s11064-013-0981-8
Reckziegel P, Peroza LR, Schaeffer LF et al (2013) Gallic acid decreases vacuous chewing movements induced by reserpine in rats. Pharmacol Biochem Be 104:132–137. doi:10.1016/j.pbb.2013.01.001
Taniguchi R, Nakagawasai O, Tan-no K et al (2013) Combined low calcium and lack magnesium is a risk fator for motor déficit in mice. Biosci Biotech Biochem 77:266–270. doi:10.1271/bbb.120671
Schmidt WJ, Kretschmer BD (1997) Behavioural pharmacology of glutamate receptors in the basal ganglia. Neurosci Biobehav Rev 21:381–392. doi:10.1016/S0149-7634(96)00044-9
Oyanagi K, Ka-wakami E, Kikuchi-Horie K et al (2006) Magnesium deficiency over generations in rats with special references to the pathogenesis of the Parkinsonism-dementia complex and amyotrophic lateral sclerosis of Guam. Neuropathology 26:115–128. doi:10.1111/j.1440-1789.2006.00672.x
Kuzniar A, Mitura P, Kurys P et al (2003) The influence of hypomagnesemia on erythrocyte antioxidant enzyme defence system in mice. Biometals 16:349–357. doi:10.1023/A:1020632505289
Minnnich et al (1971) Glutathione biosynthesis in human erythrocytes. 1. Identification of the enzymes of glutathione synthesis in hemolysates. J Clin Invest 50:507–513. doi:10.1172/JCI106519
Boparai RK, Kiran R, Bansal DD (2007) Insinuation of exacerbated oxidative stress in sucrose-fed rats with a low dietary intake of magnesium: evidence of oxidative damage to proteins. Free Radic Res 41:981–989. doi:10.1080/10715760701447892
Regan RF, Guo Y (2001) Magnesium deprivation decreases cellular reduced glutathione and causes oxidative neuronal death in murine cortical cultures. Brain Res 890:177–183. doi:10.1016/S0006-8993(00)03156-5
Colpo G, Trevizol F, Teixeira AM et al (2007) Ilex paraguariensis has antioxidant and attenuates haloperidol-induced orofacial dyskinesia and memory dysfunction in rats. Neurotox Res 12:171–180. doi:10.1007/BF03033914
Nade VS, Kawale LA, Yadav AV (2010) Protective effect of Morusalba leaves on haloperidol-induced orofacial dyskinesia and oxidative stress. Pharm Biol 48:17–22. doi:10.3109/13880200903029357
Daya RP, Tan ML, Sookram CD, Skoblenick K, Mishra RK (2011) Alpha-phenyl-N-tert-butylnitrone prevents oxidative stress in a haloperidol-induced animal model of tardive dyskinesia: investigating the behavioural and biochemical changes. Brain Res 1412:28–36. doi:10.1016/j.brainres.2011.07.014
Macêdo DS, de Oliveira GV, Gomes PXL et al (2011) B vitamins attenuate haloperidol-induced orofacial dyskinesia in rats: possible involvement of antioxidant mechanisms. Behav Pharmacol 22:674–680. doi:10.1097/FBP.0b013e32834aff6d
Patil R, Hiray Y, Shinde S, Langade P (2012) Reversal of haloperidol induced orofacial dyskinesia by Murrayakoenigii leaves in experimental animals. Pharm Biol 50:691–697. doi:10.3109/13880209.2011.618841
Teixeira A, Müller LG, Reckziegel P et al (2011) Beneficial effects of an innovative exercise model on motor and oxidative disorders induced by haloperidol in rats. Neuropharmacology 60:432–438. doi:10.1016/j.neuropharm.2010.10.017
Fix JD (2008) Basal Ganglia and the Striatal Motor System. Neuroanatomy (Board Review Series) (4th ed). Baltimore: Wulters Kluwer & Lippincott Wiliams& Wilkins. pp. 274–281. ISBN 0-7817-7245-1
Lin JY, Chung SY, Lin MC, Cheng FC (2002) Effects of magnesium sulfate on energy metabolites and glutamate in the cortex during focal cerebral ischemia and reperfusion in the gerbil monitored by a dural probe microdialysis technique. Life Sci 71:803–811. doi:10.1016/S0024-3205(02)01738-1
Mayer ML, Westbrook GL, Guthrie PB (1984) Voltage-dependent block by Mg2+ of NMDA responses in spinal cord neurones. Nature 309:261–263. doi:10.1038/309261a0
Bekkers JM, Stevens CF (1993) NMDA receptors at excitatory synapses in the hippocampus: test of a theory of magnesium block. Neurosci Lett 156:73–7. doi:10.1016/0304-3940(93)90443-O
Dingledine R, Borges K, Bowie D, Traynelis SF (1999) The glutamate receptor ion channels. Pharmacol Rev 51:7–61
Trump BF, Berezesky IK (1995) Calcium-mediated cell injury and cell death. FASEB J 9:219–28
Norberg E, Gogvadze V, Ott M et al (2008) An increase in intracellular Ca2+ is required for the activation of mitochondrial calpain to release AIF during cell death. Cell Death Differ 15:1857–1864. doi:10.1038/cdd.2008.123
Lemasters JJ, Theruvath TP, Zhong Z, Nieminen AL (2009) Mitochondrial calcium and the permeability transition in cell death. Biochim Biophys Acta Bioenerg 1787:1395–1401. doi:10.1016/j.bbabio.2009.06.009
Seo JH, Fox JG, Peek RM, Hagen SJ (2012) N-methyl-D-aspartate (NMDA) Channels regulate apoptosis in helicobacter pylori infection by ammonia-induced calcium permeation mechanisms. FASEB J 26:1156.1. doi:10.1053/j.gastro.2011.08.048
Surmeier DJ, Guzman JN, Sanchez-Padilla J (2010) Calcium, cellular aging, and selective neuronal vulnerability in Parkinson’s disease. Cell Calcium 47:175–182. doi:10.1016/j.ceca.2009.12.003
Tang TS, Slow E, Lupu V et al (2005) Disturbed Ca2+ signaling and apoptosis of medium spiny neurons in Hungtingon’s disease. P Natl Acad Sci USA 102:2602–2607. doi:10.1073/pnas.0409402102
Solaroglu I, Kaptanoglu E, Okutan O, Beskonakli E, Attar A, Kilinc K (2005) Magnesium sulfate treatment decreases caspase-3 activity after experimental spinal cord injury in rats. Surg Neurol 64:17–21. doi:10.1016/j.surneu.2005.07.058
Sencer A, Aydoseli A, Aras Y et al (2013) Effects of combined and individual use of N-methyl-D aspartate receptor antagonist magnesium sulphate and caspase-9 inhibitor z-LEDH-fmk in experimental spinal cord injury. Ulus Travma Acil Cer 19:313–319. doi:10.5505/tjtes.2013.45804
Acknowledgments
The authors are grateful to CAPES (M.K., H.J.S., C.T.D.A., K.R., and C.S.P.) and CNPq (Kr.R.) for the fellowships, as well to CNPq (M.E.B.) for the research grants. Authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kronbauer, M., Segat, H.J., De David Antoniazzi, C.T. et al. Magnesium Supplementation Prevents and Reverses Experimentally Induced Movement Disturbances in Rats: Biochemical and Behavioral Parameters. Biol Trace Elem Res 166, 163–172 (2015). https://doi.org/10.1007/s12011-015-0268-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-015-0268-9