Abstract
Background
Uncemented acetabular components have demonstrated low revision rates and high patient satisfaction but with concerns regarding increased costs compared with monoblock cups. Some newer lower-cost uncemented monoblock options have become available in the last decade, but limited data are available on their performance.
Questions/purposes
(1) Does an uncemented, titanium-backed all-polyethylene acetabular cup provide reliable fixation? (2) What is the frequency and what are the causes for revision with this cup?
Methods
Between 2004 and 2008, we elected to use an uncemented, titanium-backed all-polyethylene acetabular cup in older patients with limited physical demands. We performed 615 hip replacements in 550 patients with greater than 5 years of clinical and radiographic followup. When patients who were dead (80 hips in 75 patients), lost to followup (98 hips in 93 patients), or revised (three hips in three patients) were excluded, there were 434 hips in 379 patients for comparison of the postoperative and 5-year radiographs. Two observers not involved in the index surgical procedures (NH, HS) assessed radiographs for signs of migration or loosening. Some degree of early movement sometimes is seen before cup stabilization; however, to be conservative, we defined cups with greater than 3° of change of position (even if they subsequently stabilized) as potentially at risk and report them separately. Revision surgery, time from the index procedure, and the reason for revision were recorded from the New Zealand Joint Registry.
Results
By 5 years there was a median change in inclination of 2° (range, 0°–13°; 95% confidence interval [CI], 2.0–2.4; p < 0.001) and 2° of anteversion (range, 0°–11°; 95% CI, 2.0–2.4; p < 0.001). Although at last followup all cups appeared to have stabilized with no radiolucent lines or medial migration, 22% of the cups (94 of 434) had moved more than 3° and so were deemed to be potentially at risk. There were 11 revision procedures (of 429 hips; 2.5%) of which six were for recurrent dislocation, four for femoral fracture, and one for femoral loosening to give an overall all-cause revision rate for all components of 0.25 per 100 component years (95% CI, 0.13–0.43). No revisions were performed for acetabular loosening.
Conclusions
The short- to medium-term results of this all-polyethylene monoblock cup demonstrated a low frequency of revision. However, 94 cups were identified as potentially at risk based on movement of > 3° before apparent stabilization. Although those patients seem to be doing well enough now, the current duration of followup may not be sufficient to know that these cups will be durable, because other ongrowth designs have demonstrated a high frequency of late failure after apparent early success.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
Introduction
The use of uncemented acetabular components in THA has gained worldwide acceptance with low revision frequencies and high scores in patient-reported outcome studies [1, 2, 5, 19]. Joint registries show that the most common of these components are modular [5, 18], allowing the surgeon to change the articulating surfaces to best suit reconstructive demands. Modular cups have the advantage of giving the surgeon the option of using a lipped liner to help avoid postoperative dislocation, which is the most common cause for early revision [5], if the cup position is less than ideal. Compared with modular uncemented cups, the use of monoblock, uncemented cups has been less appealing to surgeons because of the uncertainty of adequate seating and positioning of the implant.
The aging population is predicted to place an increasing demand on health funding in the next 20 years, and in particular the rate of THA is predicted to markedly increase internationally [6, 11]. Implant costs contribute substantially to the overall procedure and surgeons are increasingly being called on to reduce these costs to allow wider access to THA. The use of a monoblock uncemented cup has the potential to reduce costs if it can be shown to be as equally effective as current modular implants with both radiological stability and comparable revision rates.
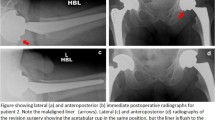
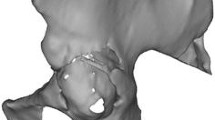
The RM classic cup (Mathys, Bettlach, Switzerland) (Fig. 1A) is an uncemented monoblock cup using ultrahigh-molecular-weight polyethylene with either a hydroxyapatite or titanium coating to achieve bony fixation. The rotational stability was enhanced with two pegs and additional screw fixation could be achieved if required. Results to date have been excellent with survivorship of 94% at 20 years [7]. Recently the RM Classic has been modified to the RM Pressfit cup (Fig. 1B) by removing the rotational pegs, increasing the size at the equator, and allowing the option of limited screw fixation. Adequate seating of the cup has been improved by overreaming the acetabulum by 1 mm. The RM Pressfit cup is available with two articulating surfaces, either ultrahigh-molecular-weight polyethylene or the vitamin E-stabilized highly crosslinked polyethylene (Vitamys; Mathys). A large number of these components have been implanted over a 10-year period, but there is little published evidence of their efficacy [12, 20].
We therefore asked: (1) Does a cementless, titanium-backed all-polyethylene acetabular cup provide reliable fixation? (2) What is the frequency and cause for revision with this cup?
Patients and Methods
Between 2004 and 2008 we elected to use an uncemented, titanium-backed all-polyethylene acetabular cup in older patients with limited physical demands. We performed 615 hip replacements in 550 patients with a median age of 76 years (range, 44–94 years) and minimum followup of 5 years. This represented 24% (615 of 2556) of our THAs during the period in question. No patient was excluded because of sex, diagnosis, or reduced bone density. All eligible patients were reviewed preoperatively by their surgeon and after clinical and radiological evaluation were identified as requiring a THA. The group included 226 males and 389 females with a median body mass index of 27.6 kg/m2 (range, 16–43 kg/m2). The operations were performed by a number of different surgeons with varying skill level, including some trainees under supervision.
Because this was a low-risk observational study and audit of radiological and functional outcome in patients receiving standard treatment and followup, ethical review and approval were not required. When patients who were dead (80 hips in 75 patients), lost to followup (98 hips in 93 patients), or revised (three hips in three patients) were excluded, there were 434 hips in 379 patients for comparison of the postoperative and 5-year radiographs.
The radiological analysis comparing the initial postoperative radiographs with those taken at 5 years was undertaken by one of two independent observers (NH, HS), neither of whom was involved in any of the primary procedures. AP pelvic radiographs were assessed for any change in acetabular version using the method described by Liaw et al. [13]. Inclination was also measured off the AP pelvis radiograph using a horizontal line between the teardrops as the transverse axis and the angle was taken between this and the face of the acetabular component. Both of these methods have been validated and found to have reliable interobserver variability [16]. Radiographs were also evaluated for any periacetabular loosening judged by radiolucent lines around the border of the acetabulum or any migration defined as medial displacement with respect to the ilioischial line compared with previous radiographs. We further used the five criteria established by Moore et al. [14] for osseointegration. Cups demonstrating at least one, two, or three of five criteria were considered to be osseointegrated. Cups with no evidence of motion at latest followup compared with immediate postoperative radiographs were considered fibrous stable, whereas cups that demonstrated motion in any plane of more than 3° were considered at risk for later loosening if they stabilized and loose if they did not. Some degree of early migration sometimes is seen before cup stabilization; however, to be conservative, we defined cups with greater than 3° of migration (even if they subsequently stabilized) as potentially at risk, and we report them separately.
Revision surgery, time from the index procedure, and the reason for revision were recorded from the New Zealand Joint Registry (NZJR). The NZJR captures information on all arthroplasties performed in our country and has an over 97% capture rate and therefore was also used to validate the rate of revision surgery within the study group. Survival was recorded as the percentage of patients who had not undergone a revision procedure for any indication and the revision rate was recorded as the rate per 100 component years.
Statistical Analysis
The mean changes in inclination and anteversion between the postoperative and 5-year radiographs were analyzed using paired t-tests.
Results
Of the 434 hips available at 5 years, all of the cups demonstrated radiographic signs of osseointegration, and none were loose. We found no radiolucent lines and no medial displacement of the implant with respect to the ilioischial line in any cup. Although at last followup, all cups appeared to have stabilized with no radiolucent lines or medial migration, 22% of the cups (94 of 434) had changed position more than 3° and so were deemed to be potentially at risk, although all looked stable at 5 years. Postoperative inclination was variable and ranged from 25° to 73° with an average of 45°. By 5 years, there was a median change in inclination of 2° (range, 0°–13°; 95% confidence interval [CI], 2.0–2.4; p < 0.001). Postoperative anteversion ranged from 0° to 36° with a median of 19°. The change in version ranged from 0° to 11° with a median of 2° (95% CI, 2.0–2.4; p < 0.001).
A total of 11 revisions were performed in the 434 hips (2.5%) with 5-year followup, giving an overall all-cause revision rate for all components of 0.25 per 100 component years (95% CI, 0.13–0.43). The cause of revision was recurrent dislocation in six, femoral fracture in four, and one for femoral loosening. No revisions were performed for acetabular failure, giving a revision rate for the cup alone of 0.12 per 100 component years (95% CI, 0.04–0.25). Time from the index procedure to revision ranged from 2 to 1959 days with an average of 428 days. Two revisions were performed early (Days 2 and 3 postoperatively) for unrecognized intraoperative femoral fracture. Both of these required additional fixation and one had a change of femoral component. Five patients had their acetabular component revised for recurrent dislocations and the final patient had augmentation of their original acetabular component (without component removal) for component malpositioning.
Discussion
Hip arthritis is a growing concern in our population with estimates that by 2030 there will be over 572,000 primary THAs and 97,000 revisions THAs performed in the United States alone [3]. THA is the definitive operation for end-stage hip arthritis and can achieve excellent clinical results. As our population ages, it is important to ensure we are using reliable, cost-effective implant choices to ensure this need is met. The RM Pressfit cup has been in use in our center for a number of years but to date there have been few published studies assessing the reliability of this component. We investigated the medium-term stability of this implant by performing a minimum 5-year radiological review. Although no revisions were performed for acetabular failure, we noted that 22% of available hips (94 of 434) were at risk for later loosening based on postoperative cup movement of more than 3° before apparent stabilization.
There are a number of limitations with this study. Most importantly, as noted, 22% (94 of 434) cups were identified as potentially at risk based on migration of 3° before apparent stabilization. Although those patients seem to be doing well enough now (no further migration, hip scores comparable to the rest of the group), the current duration of followup may not be enough to know that these cups will remain well fixed. We note that early migration has been reported by others [9] as a risk factor for late loosening and that some other ongrowth acetabular components have appeared stable early on but experienced later loosening [4, 8, 17]. Because of these issues, the hips in our series with early migration before apparent stabilization will need to be followed closely over time.
There were other limitations as well. First, it was a retrospective study using prospectively collected data with no comparative or control group. Second, all implants were selected by the surgeon at the time of surgery and initially its use was age-limited and therefore there was an age selection bias. The median age for THA in our country is 67 years compared with the median age in this cohort of 75 years [18]. This older age group may also have been responsible for reduced wear rates resulting from less activity, but it was reassuring to see that this was a stable implant that osseointegrates well into elderly patients who were likely to be prone to poorer bone quality and lower bone density. Third, there was also a large number lost to followup (30% [171 of 550 patients]), which was largely the result of the elderly nature of the patients involved with a large number of patients who were dead at followup (14% [75 of 550 patients]) as well as a large number in supported care or too unwell to attend. We are confident, however, that no major revisions have been missed because the data were crossreferenced with the NZJR, which has a > 97% national capture rate [18]. Fourth, a further limitation is the lack of standardized radiographs to assess version and inclination. Studies have shown poor interobserver reliability when using these methods [15]; however, we felt that the methodology was adequate to assess for any major changes in acetabular position.
Within the limits of radiographic technique, we found that all of the hips treated with the RM Pressfit cup were radiographically stable at 5 years with either osseointegration or fibrous stable fixation. We did not find periacetabular osteolysis or medial migration, which would suggest impending failure, in any cup. There was a wide range of values for both inclination and version recorded, which reflects the varying experience and the large number of independent surgeons involved in the operations. Our results are consistent with other recent studies [12, 20], which demonstrate low rates of early wear and migration of the RM Pressfit cup. Early wear and migration have been reported as predictors of early failure in THA [10, 17]; therefore, these promising short- to medium-term radiological results are reassuring. However, we note that other designs such as the Osteonics Dual Geometry and PSL cups (Howmedica Osteonics, Stryker, NJ, USA) demonstrated similar good early results with a subsequent alarming rise in failure rates.
The isolated revision rate for the RM cup alone in this study was low with only five (0.5%) having the acetabular component changed, all of which were for recurrent dislocations. There were no revisions for acetabular loosening or migration throughout the study period. A study by Wyss et al. [20] included 50 patients with an RM Pressfit cup with all implants maintained out to 5-year followup. A similar study by Lafon et al. [12] included 91 hips with an RM Pressfit cup and had a slightly higher revision rate at 3%, which was attributed to cup positioning at the time of surgery rather than any migration or osteolysis around the implant.
The overall revision rate for the acetabular component alone of 0.12 per 100 component years is lower than our current NZJR [18] data, which demonstrates a revision rate of 0.71 per 100 component years for all primary THAs. The RM Pressfit cup is gaining support around New Zealand and was the second most common acetabular implant used in the country in 2013 with a total of 975 implants.
This short- to medium-term study has demonstrated excellent outcomes with stable radiological findings and few revisions in the first 5 years. These results appear similar to those of an older version of the RM cup [7]. Although we are cautiously optimistic, we also sound a cautionary note because of the relatively high level of loss to followup in our study as well as because of the early migration observed. Early migration has been a harbinger of later loosening [9], and several other historical designs that relied on ongrowth rather than bony ingrowth showed similar early good results only to fail later [4, 8, 17]. Because of these factors, these patients will need to be followed closely.
References
Bjørgul K, Novicoff WM, Andersen ST, Brevig K, Thu F, Wiig M, Ahlund O. No differences in outcomes between cemented and uncemented acetabular components after 12–14 years: results from a randomized controlled trial comparing Duraloc with Charnley cups. J Orthop Traumatol. 2010;11:37–45.
Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190.
Hall A, Eilers M, Hansen R, Robinson BS, Maloney WJ, Paprosky WG, Ries MD, Saleh KJ. Advances in Acetabular reconstruction in revision total hip arthroplasty. J Bone Joint Surg Am. 2013;95:1709.
Havelin LI, Espehaug B, Engesaeter LB. The performance of two hydroxyapatite-coated acetabular cups compared with Charnley cups. J Bone Joint Surg Br. 2002;84:839–844.
Hooper G, Rothwell AG, Stringer M, Frampton CM. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–458.
Hooper GJ, Lee AJ, Rothwell AG, Frampton C. Current trends and projctions in the utilisation rates of hip and knee replacement in New Zealand from 2001 to 2026. N Z Med J. 2014;127:82–93.
Ihle M, Mai S, Pfluger D, Siebert W. The results of the titanium-coated RM acetabular component at 20 years: a long-term follow-up of an uncemented primary total hip replacement. J Bone Joint Surg Br. 2008;90:1284–1290.
Jiranek WA, Whiddon DR, Johnstone WT. Late loosening of press-fit cementless acetabular components. Clin Orthop Relat Res. 2004;418:172–178.
Klerken T, Mohaddes M, Nemes S, Karrholm J. High early migration of the revised acetabular component is a predictor of late cup loosening: 312 cup revisions followed with radioisometric analysis for 2–20 years. Hip Int. 2015 Apr 27 [Epub ahead of print].
Kostakos AT, Macheras GA, Frangakis CE, Stafilas KS, Baltas D, Xenakis TA. Migration of the trabecular metal monoblock acetabular cup system. J Arthroplasty. 2010;25:35–40.
Kurtz S. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780.
Lafon L, Moubarak H, Druon J, Rosset P. Cementless RM Pressfit® Cup. A clinical and radiological study of 91 cases with at least four years follow-up. Orthop Traumatol Surg Res. 2014;100:S225–S229.
Liaw C-K, Hou S-M, Yang R-S, Wu T-Y, Fuh C-S. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res. 2006;451:134–139.
Moore MS, McAuley JP, Young AM, Engh CA Sr. Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176–183.
Mullaji A, Shetty GM. Cemented stems: a requisite in revision total knee replacement. Bone Joint J. 2014;96(Suppl A):115–117.
Nho J-H, Lee Y-K, Kim HJ, Ha Y-C, Suh Y-S, Koo K-H. Reliability and validity of measuring version of the acetabular component. J Bone Joint Surg Br. 2012;94:32–36.
Rahbek O, Overgaard S, Soballe S, Bunger C. Polyethylene wear, osteolysis and acetabular loosening with an HA-coated prosthests: a follow up of 94 consecutive arthroplasties. J Bone Joint Surg Br. 1996;81:582–589.
The New Zealand Joint Registry. Available at: www.nzoa.org.nz/nz-joint-registry. Accessed January 8, 2015.
Wyatt M, Hooper G, Frampton C, Rothwell A. Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World J Orthop. 2014;5:591.
Wyss T, Kägi P, Mayrhofer P, Nötzli H, Pfluger D, Knahr K. Five-year results of the uncemented RM Pressfit Cup clinical evaluation and migration measurements by EBRA. J Arthroplasty. 2013;28:1291–1296.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Hooper, N., Sargeant, H., Frampton, C. et al. Does a Titanium-coated Polyethylene Press-fit Cup Give Reliable Midterm Results?. Clin Orthop Relat Res 473, 3806–3810 (2015). https://doi.org/10.1007/s11999-015-4556-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4556-7