Abstract
Background
Most acetabular revisions are managed with cementless hemispherical or elliptical metal implants relying on bone ingrowth. Nonetheless, loss of acetabular bone stock and inability to achieve secure component fixation represent challenges in the setting of revision total hip arthroplasty. Impaction bone grafting (IBG) using allograft represents one option for treatment of this problem. However, cup migration and bone graft resorption are limitations when IBG is used for large segmental defects, and the precise role of IBG as well as the use of mesh (and the kinds of defects for which mesh does not work well) in this setting remains unknown.
Questions/purposes
We therefore evaluated patients undergoing acetabular revision surgery using IBG and a cemented cup in large bone defects to determine (1) the frequency with which the hip center could be restored in hips with Paprosky 3A and 3B defects and in hips with or without the use of metallic mesh during surgery; (2) survivorship of IBG acetabular-revision reconstructions in patients with severe Paprosky 3A and 3B defects; and (3) risk factors for failure of the reconstruction, including the use of mesh and defect severity (3A versus 3B).
Methods
Between 1997 and 2009, we performed 226 acetabular revisions using IBG. During that time, indications for using IBG in this setting included Paprosky 3A and 3B defects without pelvic discontinuity. Of these, 204 (90.2%) were available for followup at a minimum of 5 years (mean, 10 years; range, 5–17 years). There were 100 hips with an intraoperative bone defect of Paprosky 3A and 104 with a 3B. Medial or rim acetabular uncontained defects were treated with medial and/or lateral metallic mesh in 142 hips. We determined the postoperative radiological cup position and acetabular reconstruction of the hip center according to Ranawat in both groups. We assessed the appearance of cup loosening and the possible risk factors with regression analysis.
Results
Mean postoperative acetabular abduction angle and vertical, horizontal, and hip rotation center distances improved (p < 0.001 in all parameters). Nine hips showed radiological loosening in the group with bone defect 3A and 16 in Group 3B. The survival rate for loosening at 15 years was 83% (95% confidence interval [CI], 71%–95%) for Group 3A and 73% (95% CI, 60%–84%) for Group 3B (p = 0.04). The survivorship for loosening when using mesh or not at 15 years was: no mesh 89% (95% CI, 74%–99%), medial mesh 85% (95% CI, 72%–97%), lateral mesh 80% (95% CI, 67%–91%), and medial and lateral meshes 54% (95% CI, 31%–76%) (p = 0.008). After controlling the most relevant confounding variables we found that the most important factor associated with loosening was lateral mesh use (p = 0.008; hazard ratio, 2.942; 95% CI, 1.328–6.516).
Conclusions
IBG provides an improvement in reconstruction of the hip rotation center in acetabular revision surgery. Although results are good for contained or medial large defects, hips with a rim or lateral segmental defect may need other options for reconstruction of these challenging surgeries.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Cementless cups are a durable option in revision hip surgery, although they have shown some limitations when major acetabular bone loss is present [11]. The impaction bone grafting (IBG) technique was introduced for use in the acetabulum by Slooff et al. [35] and has proven to be effective in revision surgery. Different series have confirmed excellent results using this technique [10, 30, 32, 33] and bone graft incorporation has been reported in histologic and positron emission tomography studies [2, 4, 28, 31, 34, 37]. In a goat model of impacted allograft, Schimmel et al. [28] showed complete incorporation of the allograft by 48 weeks. Studying 24 human acetabular biopsies after reconstruction, Van der Donk et al. report similar findings [38].
However, cup migration and bone graft resorption are some of the limitations after IBG in revision surgery when used for large segmental defects despite the use of medial and lateral stainless steel meshes specifically designed to reconstruct segmental bone loss [12, 15, 27, 40]. Because of these concerns, the precise role of IBG as well as the use of mesh (and the kinds of defects for which mesh does not work well) in this setting remains unknown.
We therefore evaluated patients undergoing acetabular revision surgery using IBG and a cemented cup in large bone defects to determine (1) the frequency with which the hip center could be restored in hips with Paprosky 3A and 3B defects and in hips with or without the use of metallic mesh during surgery; (2) survivorship of IBG acetabular-revision reconstructions in patients with severe Paprosky 3A and 3B defects; and (3) risk factors for failure of the reconstruction, including use of mesh and defect severity (3A versus 3B).
Patients and Methods
Between January 1, 1997, and December 31, 2009, we performed 226 acetabular revision surgeries using IBG and a cemented cup in 217 patients. The indications were hips with Paprosky 3A and 3B defects [24]. During that time patients with milder bone defects were treated with a cementless porous-coated or tantalum cups and hips with a pelvic discontinuity with alternate techniques including stabilization of both columns. Two hundred and four hips (196 patients [90.2%]) were available for followup at a minimum of 5 years (mean, 10 years; range, 5–17 years). Twenty-one patients (22 hips) were excluded: nine patients had died for reasons unrelated to the revision surgery and 12 (13 hips) were lost to followup. Each revised cup was individually assessed; 76 (37%) only underwent acetabular revision, whereas 128 (63%) underwent revision of both components. There were 100 Grade 3A hips and 104 Grade 3B hips.
Mean age was 69 years (± 13.1) for the whole series and the most frequent diagnosis was primary osteoarthritis (Table 1). There was no difference in age between the Grade 3A patients and the Grade 3B patients. The groups were different in terms of sex; the Grade 3A group included 24 men and 76 women, whereas the 3B group included 37 men and 67 women (p = 0.49). Data on body mass index were not available. The average time between the initial THA and the revision acetabular surgery described here was 76 months (range, 38–194 months). First revision surgeries were more frequent in 3A than in 3B defects (p < 0.001). Medial and lateral stainless steel meshes specifically designed to reconstruct loss of bone (X-change; Stryker, Howmedica International, Staines, Middlesex, UK) were used for segmental uncontained defects with a size greater than 2 cm3 on the medial side or the roof of the acetabulum. The use of metallic meshes was also more frequent in 3B defects (Table 1).
All surgeries were done by the same surgical team (three different surgeons) using a posterolateral approach. The acetabular cup and cement were removed and the membrane excised and sent for histologic and bacteriologic study. The acetabular margins were defined. When appropriate, segmental acetabular defects were reconstructed with metallic meshes screwed to the bone bed. We used medial and/or rim metallic meshes for uncontained defects in 142 hips in 134 patients, including medial mesh in 56, lateral mesh in 51, and both in 35. No mesh was used in 62 hips (Table 1). Fresh-frozen femoral heads allograft from the bone bank were used in all hips. Allograft bone chips were morselized with a bone mill (Lere Bone Mill; Johnson & Johnson, DePuy, Warsaw, IN, USA) or manually using a rongeur with a size of 0.7 to 1 cm3 and impacted with a trial prosthesis socket from X-Change instruments (Stryker, Howmedica International) according to the Nijmegen technique [36, 39]. The acetabulum was cleaned and filled with bone graft to a thickness of at least 5 mm [38]. A standard low-profile all-polyethylene cup (Stryker, Howmedica International) was cemented using antibiotic-loaded PMMA (Palacos with gentamicin; Merck, Darmstadt, Germany) in 177 hips in 170 patients. In cases in which a well-fixed Charnley stem was associated with a loosened 22.25-mm Charnley cup, a Charnley cemented cup (Johnson & Johnson, DePuy) was used (27 hips in 26 patients).
Standard AP and lateral radiographs of the pelvis were made for all patients immediately after operation and at every followup examination. All postoperative and followup radiographs were made at our institution following the same protocol [18]. Measurements were made by a single author (EG-R). The locations of radiolucent lines around the cup were recorded using the DeLee and Charnley zones [9]. The preoperative and postoperative positions of the cup were assessed by determining the acetabular inclination of the cup. The center of rotation of the hip was defined using the center of the femoral head and the interteardrop line or obturator foramina. The true acetabular region was defined according to Ranawat et al. [26]. The approximate femoral head center was used as the reference point to measure distances between the center of rotation of the patient’s normal hip and the center of the prosthetic femoral head. These distances were recorded for each hip. Radiographic cup loosening was difficult to evaluate because of the frequent use of metallic meshes. However, cup migration was defined as a change of more than of 5º in the acetabular abduction angle or of 5 mm in either the height or lateral position of the cup. Radiographic cup loosening was defined based on Schmalzried and Harris criteria [29] and classified as definite loosening, probable loosening, or possible loosening. Although bone graft density, appearance of the graft-host junction, and trabecular continuity between bone graft and acetabular bone could be assessed by radiographs, these parameters are of limited usefulness in evaluating bone graft remodeling [14, 33]. The anatomic center of the hip was considered as reconstructed when the distance between the femoral head and the desired center of rotation was less than 5 mm.
Qualitative data were expressed as counts and percentages and quantitative data by means ± SD. Qualitative data for hips with and bone defect 3A and 3B were compared using the chi-square test or Fisher’s exact test, and quantitative data for these groups and for hips with or without mesh were compared using Student’s t-test. Pearson’s chi square test was used to compare the demographic qualitative data of patients between groups. Kaplan-Meier survivorship analysis [19] with 95% confidence intervals (CIs) was used to estimate the cumulative probabilities of not having cup loosening related to the bone defect or the use of metallic mesh. Differences in survival were determined using the log-rank test. Pre- and postoperative changes in the inclination angle, the height and location of the center of the hip, and/or the distance between the femoral head and the desired center of rotation for the two groups were compared using two-way analysis of variance of repeated-measures factoring for Grade 3A and 3B hips. To assess the possible risk factors for cup loosening, Cox proportional hazard regression analysis [8] was performed to determine whether bone defect (3A or 3B), the use of a lateral mesh, and the postoperative radiological cup position (vertical distance and hip rotation center distance) affected the loosening rate over time. Statistical analysis was performed using statistical package SAS 9.3 (SAS Institute Inc, Cary, NC, USA).
Results
There was an improvement in both groups in the postoperative cup position for all measurements, including acetabular abduction angle, horizontal and vertical distances, and distance from the femoral head to the desired center of rotation (p < 0.001 in all parameters) (Fig. 1). Preoperative radiological findings showed that cup position was worse in 3B hips than 3A hips; however, postoperative acetabular abduction angle and horizontal distance were similar (p = 0.813 and p = 0.196, respectively) (Table 2). Postoperative vertical and hip rotation distances were greater in 3B hips (p < 0.001 for both parameters). No differences were found in postoperative cup position regarding the use of different metallic mesh (Table 3).
(A) Preoperative radiograph of a 65-year-old woman showing a loosened threaded cup. (B) Postoperative radiograph of the same patient taken at the 14th year followup examination shows the segmental acetabular defect treated with IBG and cement. A metallic mesh with screws had been used to reconstruct the acetabulum. The cup is stable, the bone graft is incorporated, and the patient has a good clinical result.
Nine hips showed radiologically probable or definite loosening in the group with a 3A bone defect and 19 in Group 3B (Fig. 2). The cumulative probability of not having definite or probable loosening at 15 years by bone defect was 83% (95% CI, 71%–95%) for Group 3A and 73% (95% CI, 60%–84%) for Group 3B (Mantel-Cox, p = 0.04) (Fig. 3). The cumulative probability of not having probable or possible loosening with the use of a metallic mesh at 15 years was: no mesh 89% (95% CI, 74%–99%), medial wall mesh 85% (95% CI, 72%–97%), lateral mesh 80% (95% CI, 67%–91%), and medial and lateral meshes 54% (95% CI, 31%–76%) (Mantel Cox, p = 0.008) (Fig. 4). There were 14 hips rerevised: three resulting from recurrent dislocation, two for infection, eight attributable to cup loosening rerevised to a new reconstruction using IBG, and one hip with severe congenital hip disease and major bone graft resorption converted to permanent resection arthroplasty at last followup. Nineteen loosened hips were not revised because the patients reported only mild symptoms, their physical activity was not high, and they refused surgery (Table 4).
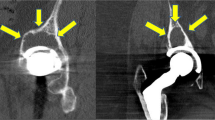
(A) Postoperative radiograph of a 78-year-old woman showing a segmental acetabular defect treated with IBG and cement. A metallic mesh with screws was used to reconstruct the acetabulum. (B) Postoperative radiograph of the same patient taken at the 20-month followup examination showing definite loosening of the cup. The cup is migrated, the bone graft presents major resorption, the lateral mesh has failed, and the patient has a poor clinical result.
Finally, we analyzed the possible relationship among the preoperative bone defect, the use or not of meshes, surgical technique according to the radiographic reconstruction on the postoperative radiograph, and the appearance of cup loosening. After controlling these relevant confounding variables, we found that the most important factor associated with loosening was lateral mesh use (p = 0.008; hazard ratio, 2.942; 95% CI, 1.328–6.516; Table 5).
Discussion
Most acetabular revisions can be managed with cementless hemispherical or elliptical metal implants relying on bone ingrowth. However, these provide poor results when acetabular bone defects are greater than 50%, particularly if the posterior column and the dome are not intact [11]. Other options are available, including extralarge components [41], antiprotrusio cages [1], and trabecular metal devices [20]. Nonetheless, loss of acetabular bone stock and inability to achieve secure component fixation represent challenges in the setting of revision THA. IBG combined with cemented fixation offers the opportunity for regeneration of bone stock and allows restoration of the anatomic and biomechanical natural center of rotation of the hip [12, 30]. Low rates of aseptic loosening at different followups have been reported using this technique (Table 6). However, other series also report cup migration and bone graft resorption after IBG in revision surgery when used for large segmental defects [27, 40]. We therefore evaluated patients undergoing IBG and a cemented cup to determine (1) the frequency with which the hip center could be restored in hips with Paprosky 3A and 3B defects and in hips with or without the use of metallic mesh during surgery; (2) survivorship of IBG acetabular revision reconstructions in patients with severe Paprosky 3A and 3B defects; and (3) risk factors for failure of the reconstruction, including the use of mesh and defect severity (3A versus 3B).
Some of the limitations in our study may be the case number because this might have influenced some statistical p values close to 0.05; a larger number may have powered these findings. However, our series represents a large group with extended followup, and we doubt that a larger patient group would result in substantial changes in either our technique or our conclusions. Although we followed the surgical recommendations from Nijmegen, we are aware that differences between this and other institutions may also affect the results. We lacked a control group of patients with similar ages and acetabular defects who were operated on with other techniques with which to compare our observations. Different postoperative management regarding bone defect and acetabular and femoral sides could also influence results [22]. Cup migration and bone allograft resorption were difficult to evaluate when metallic mesh was used on conventional radiographs. This analysis could be inadequate for detecting migration of less than 4 to 6 mm, a less accurate method than radiostereometric analysis (RSA), which could have detected migration and rotation of the cup at an early stage and over time [19]. Last, we also lacked biopsies and autopsy retrieval of acetabula reconstructed with this technique to confirm the bone graft remodeling and new bone formation.
Like in other series [12, 32], we observed that the use of IBG and a cemented cup in acetabular revision surgery is a durable option for large defects. Postoperative cup position improved in this series, even for hips with 3B, findings that may promote low rates for rerevision, which depends on achieving adequate fixation of the new implant, restoring the anatomic center of rotation of the hip, and restoring bone stock loss [39]. This new cup position reflects the amount of filling, which is a combination of graft, which may be greater than 5 mm thickness in large defects, and cement [38]. The better radiological reconstruction in 3A patients, particularly for the vertical distance and reconstruction of the hip rotation center according to Ranawat et al. [26], may also have influenced differences observed between groups. Metallic mesh use was more frequent in 3B hips; however, postoperative clinical score was similar except for ROM and the postoperative cup position. This might be explained because adequate reconstruction with this technique can be obtained, but the different rates for loosening between medial and lateral mesh use can also be one of the reasons for these observations as described subsequently.
The rates of cup loosening were worse for hips with 3B defects and particularly when we used a large lateral mesh to repair a large segmental defect. We also observed that all loosened cups did not require rerevision because mild groin pain is well tolerated in some patients [12, 25]. Although there is a place for IBG, and the advantage of this method is that if a further operation is required, there is likely to be more living bone present; the poorer result when a large rim mesh was used has led surgeons to consider the use of acetabular tantalum augments combined with or without IBG [27]. Metal augments try to create peripheral acetabular containment to facilitate graft impaction [16]. Different series have been recently published reporting good preliminary results [3, 13, 15, 16].
After controlling for relevant confounding variables such as preoperative bone defect and postoperative radiological position, we found that the most important factor for loosening was the use of a lateral mesh, which suggests that this option for reconstruction may not be enough for a large segmental defect on the rim rather than bone defect and the postoperative radiological reconstruction. Rigby et al. [27] and Van Haaren et al. [40] also report poor results in patients with these large segmental defects. Rigby et al. explain that the mechanism of failure of these cups consisted of movement and rotation of the cup/cement composite within the graft. This was followed, eventually, by the mesh being pulled off the reconstructed rim. Another possible explanation for this failure rate in this series could be that in large segmental defects, the absence of superior bony support leads to a large amount of bone graft being placed at the most loaded area above the acetabular component. Owing to insufficient support for the bone graft, it is likely that micromovement of the prosthesis results in implant failure [40]. RSA studies have shown that almost all impacted sockets migrate in the postoperative period, although the rate of migration decreases with time. Ornstein et al. report that 41% of sockets were still found to be migrating 18 to 24 months after surgery [23]. Only fresh-frozen allograft has been used in this series and results and histology with untreated graft have been reported [17]. Although we used chips with a size of 0.7 to 1 cm3 [39], larger chips and larger diameter cups make it possible to fill the cavity and could improve these poor results. Obviously, in challenging cases with large rim segmental defects, a substantial layer of bone graft to a thickness of at least 5 mm under the large rim mesh could not be obtained in all cases in this series [38].
These findings allow us to conclude that IBG combined with cemented fixation offers the opportunity for regeneration of bone stock and provides improvement of the reconstruction of the rotation of the hip center in most hips in acetabular revision surgery; however, although results are good for contained or medial large defects, hips with a large rim segmental defect may need other options for reconstruction of these challenging surgeries.
References
Berry DJ, Müller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg Br. 1992;74:711–715.
Board TN, Rooney P, Kay PR. Strain imparted during impaction grafting may contribute to bony incorporation; an in vitro study of the release of BMP-7 from allograft. J Bone Joint Surg Br. 2008;90:821–824.
Borland WS, Bhattacharya R, Holland JP, Brewster NT. Use of porous trabecular metal augments with impaction bone grafting in management of acetabular bone loss. Early to medium-term results. Acta Orthop. 2012;83:347–352.
Buma P, Lamerigts N, Schreurs BW, Gardeniers J, Verslayen D, Slooff TJJH. Impacted graft incorporation after cemented acetabular revision. Histological evaluation in 8 patients. Acta Orthop Scand. 1996;67:536–540.
Buttaro MA, Comba F, Pusso R, Piccaluga F. Acetabular revision with metal mesh, impaction grafting, and a cemented cup. Clin Orthop Relat Res. 2008;466:2482–2490.
Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular reconstruction with impacted bone allografts and cemented acetabular components: a 2- to 13-year follow-up study of 142 aseptic revisions. J Bone Joint Surg Br. 2006;88:865–869.
Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular revision surgery with impacted bone allograft and cemented cups in patients younger than 55 years. Int Orthop. 2009;33:611–616.
Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34:187–220.
DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip arthroplasty. Clin Orthop Relat Res. 1976;121:20–32.
El-Kawy S, Hay D, Drabu K. Clinical and radiological bone allograft technique results of impaction in acetabular revisions associated with massive bone stock deficiencies: four to seven years follow-up study. Hip Int. 2005;15:46–51.
García-Cimbrelo E. Porous-coated cementless acetabular cups in revision surgery: a 6- to 11-year follow-up study. J Arthroplasty. 1999;14:397–406.
García-Cimbrelo E, Cruz-Pardos A, Garcia-Rey E, Ortega-Chamarro J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin Orthop Relat Res. 2010;468:3304–3313.
Gehrke T, Bangert Y, Schwantes B, Gebauer M, Kendoff D. Acetabular revision in THA using tantalum augments combined with impaction bone grafting. Hip Int. 2013;23:359–365.
Gerber SD, Harris WH. Femoral head autografting to augment acetabular deficiency in patients requiring total hip replacement: a minimum five-year and an average seven-year follow-up study. J Bone Joint Surg Am. 1986;68:1241–1248.
Gilbody J, Taylor C, Bartlett GE, Whitehouse SL, Hubble MJW, Timperley AJ, Howell JR, Wilson MJ. Clinical and radiographic outcome of acetabular impaction grafting without cage reinforcement for revision hip replacement. A minimum ten-year follow-up study. Bone Joint J. 2014;96:188–194.
Gill K, Wilson MJ, Whitehouse SL, Timperley AJ. Results using Trabecular Metal augments in combination with acetabular impaction bone grafting in deficient acetabula. Hip Int. 2013:23:522–528.
Heekin RD, Engh CA, Vinh T. Morselized allograft in acetabular reconstruction. A postmortem retrieval analysis. Clin Orthop Relat Res. 1995;319:184–190.
Johnston RC, Fitzgerald RH Jr, Harris WH, Poss R, Müller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement: a standard system of terminology for reporting results. J Bone Joint Surg Am. 1990;72:161–168.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481.
Lachiewicz PF, Soileau ES. Tantalum components in difficult acetabular revisions. Clin Orthop Relat Res. 2010;468:454–458.
Merle D’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475.
Ornstein E, Franzen H, Johnsson R, Stefansdottir A, Sundberg M, Tagil M. Hip revision with impacted morselized allograft: unrestricted weight-bearing and restricted weight-bearing have similar effect on migration. A radiostereometry analysis. Arch Orthop Trauma Surg. 2003;123:261–267.
Ornstein E, Franzén H, Johnsson R, Stefánsdóttir A, Sundberg M, Tägil M. Five-year follow-up of socket movements and loosening after revision with impacted morselized allograft bone and cement. A radiostereometric and radiographic analysis. J Arthroplasty. 2006;21:975–984.
Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44.
Pupparo F, Engh CA. Comparison of porous-threaded and smooth-threaded acetabular components of identical design. Two- to four-year results. Clin Orthop Relat Res. 1991;271:201–206.
Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am. 1980;62:1059–1065.
Rigby M, Kenny PJ, Sharp R, Whitehouse SL, Gie GA, Timperley JA. Acetabular impaction grafting in total hip replacement. Hip Int. 2011;21:399–408.
Schimmel JW, Buma P, Versleyen D, Huiskes R, Slooff TJJH. Acetabular reconstruction with impacted morcellized cancellous allografts in cemented hip arthroplasty: a histologic and biomechanical study on the goat. J Arthroplasty. 1998;13:438–448.
Schmalzried TP, Harris WH. The Harris-Galante porous-coated acetabular component with screw fixation: radiographic analysis of eighty-three primary hip replacement at a minimum of five years. J Bone Joint Surg Am. 1992;74:1130–1139.
Schreurs BW, Bolder SBT, Gardeniers JWM, Verdonschot N, Slooff TJJH, Veth RPH. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup. A 10- to 20-year follow-up. J Bone Joint Surg Br. 2004;86:492–497.
Schreurs BW, Buma P, Huiskes R, Slagter JL, Slooff TJ. Morselized allografts for fixation of the hip prosthesis femoral component: a mechanical and histological study in the goat. Acta Orthop Scand. 1994;65:267–275.
Schreurs BW, Keurentjes JC, Gardeniers JWM, Verdonschot N, Slooff TJJH, Veth RPH. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component. A 20- to 25-year follow-up. J Bone Joint Surg Br. 2009;91:1148–1153.
Schreurs BW, Slooff TJJH, Buma P, Gardeniers JWM, Huiskes R. Acetabular reconstruction with impacted morselized cancellous bone graft and cement. A 10- to 15-year follow-up of 60 revision arthroplasties. J Bone Joint Surg Br. 1998;80:391–395.
Singer GC, Muirhead-Allwood SK. The histology of impacted cancellous allograft in acetabular reconstruction. Hip Int. 1999;9:20–24
Slooff TJ, Buma P, Schreurs BW, Schimmel JW, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop Relat Res. 1996;324:108–115.
Slooff TJJH, Schimmel JW, Buma P. Cemented fixation with bone grafts. Orthop Clin North Am. 1993;24:667–677.
Ullmark G, Sörensen J, Nilsson O. Bone healing of severe acetabular defects after revision arthroplasty. A clinical positron emission tomography study of 7 cases. Acta Orthop. 2009;80:179–183.
Van der Donk S, Buma P, Slooff TJJH, Gardeniers JWM, Schreurs BW. Incorporation of moreselized bone grafts: a study of 24 acetabular biopsy specimens. Clin Orthop Relat Res. 2002;396:131–141.
Van Egmond N, De Kam DCJ, Gardeniers JWM, Schreurs BW. Revisions of extensive acetabular defects with impaction grafting and a cement cup. Clin Orthop Relat Res. 2011;469:562–573.
Van Haaren EH, Heyligers IC, Alexander FG, Wuisman PI. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg Br. 2007;89:296–300.
Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83:1352–1357.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
García-Rey, E., Madero, R. & García-Cimbrelo, E. THA Revisions Using Impaction Allografting With Mesh Is Durable for Medial but Not Lateral Acetabular Defects. Clin Orthop Relat Res 473, 3882–3891 (2015). https://doi.org/10.1007/s11999-015-4483-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4483-7