Abstract
Background
Injury to subchondral bone is associated with knee pain and osteoarthritis (OA). A percutaneous calcium phosphate injection is a novel approach in which subchondral bone marrow edema lesions are percutaneously injected with calcium phosphate. In theory, calcium phosphate provides structural support while it is gradually replaced by bone. However, little clinical evidence supports the efficacy of percutaneous calcium phosphate injections.
Questions/purposes
We asked: (1) Does percutaneous calcium phosphate injection improve validated patient-reported outcome measures? (2) What proportion of patients experience failure of treatment (defined as a low score on the Tegner Lysholm Knee Scoring Scale)? (3) Is there a relationship between outcome and age, sex, BMI, and preoperative grade of OA?
Methods
Between September 2012 and January 2014, we treated 33 patients with percutaneous calcium phosphate injections. Twenty-five satisfied our study inclusion criteria; of those, three patients were lost to followup and 22 (88%; 13 men, nine women) with a median age of 53.5 years (range, 38–70 years) were available for retrospective chart review and telephone evaluation at a minimum of 6 months (median, 12 months; range, 6–24 months). Our general indications for this procedure were the presence of subchondral bone marrow edema lesions observed on MR images involving weightbearing regions of the knee associated with localized pain on weightbearing and palpation and failure to respond to conservative therapy (> 3 months). Patients with pain secondary to extensive nondegenerative meniscal tears with a flipped displaced component at the level of bone marrow edema lesions, or with mechanical axis deviation greater than 8° were excluded. All patients had Grades III or IV chondral lesions (modified Outerbridge grading system for chondromalacia) overlying MRI-identified subchondral bone marrow edema lesions. Percutaneous calcium phosphate injection was performed on the medial tibial condyle (15 patients), the medial femoral condyle (five patients), and the lateral femoral condyle (two patients). Concomitant partial meniscectomy was performed in 18 patients. Preoperative and postoperative scores from the Knee Injury and Arthritis Outcome Score (KOOS) and the Tegner Lysholm Knee Scoring Scale were analyzed.
Results
For patients available for followup, the outcome scores improved after treatment. The KOOS improved from a mean of 39.5 ± 21.8 to 71.3 ± 23 (95% CI, 18.6–45.2; p < 0.001) and the Tegner and Lysholm score from 48 ± 15.1 to 77.5 ± 20.6 (95% CI, 18.8–40.2; p < 0.001). However, seven of the 22 patients had poor clinical outcomes as assessed by the Tegner Lysholm Knee Scoring Scale, whereas three had fair results, five had good results, and seven had excellent results. The postoperative Tegner Lysholm score was inversely related to the preoperative Kellgren-Lawrence OA grade (R2 = 0.292; F (1.20) = 9.645; p = 0.006). We found no relationship between outcome scores and age, sex, or BMI.
Conclusions
In a study that would have been expected to present a best-case analysis (short-term followup, loss to followup of patients with potentially unsatisfactory results, and use of invasive cotreatments including arthroscopic débridements), we found that percutaneous calcium phosphate injection in patients with symptomatic bone marrow edema lesions of the knee and advanced OA yielded poor results in a concerning proportion of our patients. Based on these results, we advise against the use of percutaneous calcium phosphate injections for patients with advanced osteoarthritic changes.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) of the knee is a common cause of disability among men and women in the United States. It affects approximately 25% of adults and has become an established public healthcare issue [2, 30]. While loss of articular cartilage is the hallmark of OA, there is evidence that damage to subchondral bone can lead to the subsequent deterioration of the overlying articular cartilage [20]. Although pain with OA most likely is multifactorial, subchondral bone, which is highly innervated, may be a major contributor [7–9, 12]. Fibrovascular replacement of adipose marrow tissue in the bone marrow edema lesion and growth factor expression may promote localized increase of nociceptive fibers [21, 29]. However, the molecular mechanisms that possibly drive pain in bone marrow edema lesions are not completely clear. Early evidence for subchondral bone injury is often seen on MR images as a bone marrow edema lesion. Although bone marrow edema lesions can also be found in the asymptomatic healthy population [13, 25], the prevalence of these lesions is greater in patients with increased Kellgren-Lawrence grade of knee OA [7, 9].
A percutaneous calcium phosphate injection (Subchondroplasty®; Zimmer Knee Creations, Inc, Exton, PA, USA) is a novel technique in which a bone substitute material composed of calcium phosphate is injected in the site of a bone marrow edema lesion under fluoroscopic guidance [6]. The injected calcium phosphate is theorized to improve the structural integrity and biomechanical strength of the pathologic subchondral bone while its highly porous osteoconductive nature allows for later ingrowth of new bone capable of bearing weightbearing loads [15]. However, little has been reported in the orthopaedic surgery literature regarding clinical efficacy of percutaneous calcium phosphate injection [23].
We therefore sought to determine (1) whether percutaneous calcium phosphate injection improves validated patient-reported outcome measures in patients with symptomatic bone marrow edema lesions of the knee, (2) what proportion of patients experience treatment failure (defined as a low score on the Tegner Lysholm Knee Scoring Scale), and (3) whether there is a relationship between outcome and age, sex, BMI, and preoperative OA grading?
Patients and Methods
Our study involved an institutional review board-approved retrospective chart review and a telephone interview to assess patients’ condition at a minimum of 6 months postoperatively. The validated patient-reported questionnaires, assessed preoperatively and at the postoperative interview, included the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Tegner Lysholm Knee Scoring Scale [26]. Patient outcomes also were graded as poor, fair, good, or excellent according to the Tegner Lysholm Knee Scoring Scale (Table 1) [17]. Excellent and good outcomes were considered successes and fair and poor outcomes were considered clinical failures. Patient demographics, indications for surgery, concomitant procedures performed, and surgical complications were collected from patient charts.
We identified 33 individuals at our sports medicine clinic who received percutaneous calcium phosphate injections as treatment for symptomatic bone marrow edema lesions between September 2012 and January 2014 by reviewing our senior surgeons’ logs. To be included in our study, patients had (1) at least one bone marrow edema lesion visible on T2 fat-suppressed MRI; (2) complete preoperative and postoperative patient-reported outcome questionnaires; (3) a minimum of 6 months between the initial percutaneous calcium phosphate injection and postoperative telephone interview; and (4) no additional surgical procedures on the affected knee between the time of the index procedure and the postoperative interview.
Our general indications for use of this procedure were the presence of subchondral bone marrow edema lesions observed on MR images involving weightbearing regions of the knee associated with localized pain on weightbearing and palpation; failure to respond to conservative therapy for at least 3 months, which included a period (4 weeks) of toe-touch weightbearing using crutches, NSAIDS, intraarticular corticosteroid injection, viscosupplementation, and physical therapy. Patients with pain secondary to extensive nondegenerative meniscal tears with a flipped displaced component at the level of the bone marrow edema lesion or with mechanical axis deviation greater than 8° were excluded. Other conditions such as ganglion or Baker’s cysts were ruled out as the primary source of pain. Large chondral defects, fractures, dislocations, and Kellgren-Lawrence grade greater than 3 were considered contraindications. It is likely that some patients meeting these indications were treated with other approaches as well.
Of the initially identified 33 patients who received percutaneous calcium phosphate injection, 25 satisfied our inclusion criteria. A total of 22 individuals (88%) were available for a postoperative telephone interview at a minimum of 6 months (median, 12 months; range, 6–24 months) and were included in the analysis (Table 2). Two patients had severe back problems and thought the majority of their limitations were attributable to their back pain. This being a confounding factor, they were excluded. One patient could not be contacted.
Median age of the 13 men and nine women was 53.5 years (range, 38–70 years). Fifteen percutaneous calcium phosphate injections were performed on the medial tibial condyle, five on the medial femoral condyle, and two on the lateral femoral condyle. Concomitant partial medial and lateral meniscectomy were performed in 16 patients and two underwent partial medial meniscectomy only (Table 3). The mean preoperative ROM was 0° to 128° (range, 0°–120° to 0°–145°).
Operative Technique
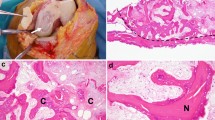
Four fellowship-trained, attending orthopaedic surgeons (LJ, TY, RHG, AJF) at our institution performed all surgical procedures with the patients under general anesthesia. We used standard medial and lateral arthroscopic portals. When necessary, we performed partial meniscectomy or chondral débridement to stable margins using standard techniques, followed by the percutaneous calcium phosphate injection. We performed fluoroscopy in the AP and lateral planes and then secured a reference frame on the femur or tibia, depending on the location of the bone marrow edema lesion (Fig. 1). We used preoperative MRI to establish the exact location of the bone marrow edema lesion and select the optimal trajectory. Under image intensification fluoroscopy, we localized the bone marrow edema lesion and passed a guide pin through the reference frame and a percutaneous incision to the center of the lesion (Fig. 2). The Subchondroplasty® fenestrated cannula then was inserted over the guide pin, with subsequent removal of the guide pin.
(A) A coronal view shows preoperative subchondral bone marrow edema lesion on fat-suppressed proton density-weighted MRI (TR/TE = 4490/32) involving the medial tibial plateau of a 54-year-old man with osteoarthritis of the left knee. (B) An intraoperative fluoroscopic image of the same knee shows the tip of the fenestrated cannula in the center of the bone marrow edema lesion.
As recommended by the manufacturer, the standardized amount (5 cc) of calcium phosphate was used for all patients. The cannula served as a guide for injection of the calcium phosphate and was rotated in 90° intervals to ensure proper filling of the lesion. This was confirmed by image intensification fluoroscopy. After the injection, the Subchondroplasty® trocar was inserted in the cannula to push the remaining calcium phosphate out of the cannula and kept in place for 5 minutes to allow for an appropriate set time. The arthroscope then was reinserted in the knee to confirm that no extravasation into the intraarticular space occurred. Final images confirmed that the calcium phosphate was injected into the site of the bone marrow edema lesion. The cannula was removed. Portals were injected extraarticularly with 20 cc of 0.25% bupivacaine hydrochloride and closed with Number 3-0 nylon sutures; then a sterile dressing was applied to the knee.
The median operative time was 45 minutes (range, 30–68 minutes) and estimated blood loss was minimal. No intra- or postoperative complications related to the percutaneous calcium phosphate injection were observed.
As recommended by the manufacturer, all our patients were limited to partial weightbearing using crutches for the first 2 postoperative weeks. Thereafter, gradual progression to full weightbearing was permitted. Physical therapy was prescribed to regain full ROM of the knee. Selected patients also received intraarticular viscosupplementation and pain medication as needed (Table 3). Patients visited the clinic for their last postoperative followup at a median of 1.8 months (range, 10 days–20 months). No swelling or drainage was noted at the injection site and ROM was at preoperative values.
Statistical analyses were performed using SPSS® 22.0 (2013, IBM Corp; Armonk, NY, USA). Median or mean and SD are reported as descriptive statistics. A two-tailed paired t-test was used to investigate the difference between pre- and postoperative patient-reported outcome scores. Stepwise regression analyses were performed to test the relationship between the postoperative Tegner Lysholm score and sex, age, BMI, and preoperative Kellgren-Lawrence OA grade. Data were considered significant at a p less than 0.05.
Preoperative physical examination findings in 13 patients prompted assessing mechanical axis deviation with bilateral, standing, full-length AP plain radiographs. We verified that mechanical varus and valgus malalignment did not exceed the recommended maximum of 8° for the percutaneous calcium phosphate injection without simultaneous joint alignment correction [6]. Eleven of the 13 patients had a mean preoperative mechanical varus alignment of 4.4° ± 2.1° (range, 2°–8°). Two patients had 8° and 7° mechanical valgus alignment, respectively (Table 2).
Results
In the patients available for followup, the average outcome scores improved after treatment (Table 2). The KOOS improved from a mean of 39.5 ± 21.8 to 71.3 ± 23 (95% CI, 18.6–45.2; p < 0.001) and the Tegner Lysholm score from 48 ± 15.1 to 77.5 ± 20.6 (95% CI, 18.8–40.2; p < 0.001).
However, according to the Tegner Lysholm Knee Scoring Scale, seven of the 22 patients had poor results, three had fair results, five had good results, and seven had excellent results.
Of the 22 patients who were evaluated via postoperative telephone interview, only 12 (55%) had outcomes considered a clinical success and 10 (45%) had outcomes that were considered a clinical failure.
Linear regression established that preoperative Kellgren-Lawrence grade had a moderate and inverse relationship with postoperative Tegner Lysholm score (R2 = 0.292, F (1.20) = 9.645; p = 0.006).
No relationship was observed between postoperative Tegner Lysholm score and sex, age, and BMI.
Discussion
The natural history of bone marrow edema lesions in patients with OA does not seem to show a linear pattern [5]. They can produce regression or resolution, but also can enlarge or newly appear [11]. Compared with transient bone marrow edema lesions associated with ACL injuries, bone marrow edema lesions associated with OA seem less likely to resolve, but also have been positively correlated with accelerated progression of OA [16, 27].
Core decompression for treatment of early avascular necrosis of the knee is an accepted method [18, 19]. However, its use with bone marrow edema lesions of the knee is not well documented. Only a few cases of successful core decompression with bone marrow edema syndrome of the knee have been reported [3, 4, 22].
Direct injection of polymethylmethacrylate into bone marrow edema lesions associated with vertebral compression fractures or sacral insufficiency fractures have been performed more frequently [10, 28]. However, to our knowledge, the Subchondroplasty® procedure is the first to use direct injection of calcium phosphate into bone marrow edema lesions associated with knee OA. Introduction of calcium phosphate into the affected area has been proposed as a possible treatment modality and prevention of progression. Subchondroplasty, first described by Sharkey et al. [24], involves the injection of a proprietary mixture of calcium phosphate into selected lesions. This mixture uses a combination of macroporous calcium phosphate, with a pore size of 150 to 500 µm optimized for bone ingrowth, and a microporous preparation (pore size < 5 µm) optimized for easy biodegradability. However, there is little reported in the orthopaedic surgery literature regarding clinical efficacy of percutaneous calcium phosphate injections [23].
Our study has several important limitations, most of which would be expected to increase the apparent benefits of the treatment studied. First, three of our 25 patients were lost to followup. Second, although Cohen and Sharkey [6] stated that pain reduction and return to full activity might take 2 to 3 months, our followup was short. A minimum of 6 months may not be enough time to determine whether these lesions have stabilized. Patients might have recurring symptoms that would not have been detected in this short-term study. In addition, many of our patients had cotreatments (including invasive treatments such as arthroscopy and some have been using analgesics or antiinflammatory medications), which would be expected to improve the apparent observed benefits. Other study limitations include the small number of patients and their wide age range. This limits the power to detect meaningful relationships. In addition, full-leg weightbearing AP radiographs were available for only 13 patients. A larger number would have been helpful in analyzing mechanical axis deviation as a potential risk factor. However, to better understand our study cohort, we added an approximate mechanical axis based on the anatomic axis, as described by Kraus et al. [14]. Nearly all of these limitations suggest that our analysis represents a best-case scenario for percutaneous calcium phosphate injections, yet we had (based on a good or excellent Tegner Lysholm score in patients who followed up) treatment success in only 12 of 22 patients thus treated.
Only a couple case reports regarding calcium phosphate injections are available to date [1, 23]. In 2012 Sharkey et al. [23] reported the case of a 51-year-old woman (BMI, 36.7 kg/m2) with severe degenerative arthritis of the medial compartment, stress fracture, and a bone marrow edema lesion of the medial tibial plateau, but no meniscal disorder. They reported good results with percutaneous calcium phosphate injection at 31 months followup. The subchondral bone marrow edema lesion resolved and knee pain decreased to 1/10 on a VAS score [23]. Abrams et al. [1] treated a skeletally immature patient with lateral tibial plateau osteochondritis dissecans with subchondral injection of calcium phosphate. They showed that the percutaneous calcium phosphate injection could be performed without violating the physis; however, data for clinical outcome were not available.
All but one of our patients had improvement of clinical outcome scores from the preoperative baseline. However, using the Tegner Lysholm grading system (Table 1), we found that 10 of the 22 patients had an outcome considered a treatment failure. Percutaneous calcium phosphate injection has a theoretical potential to become a widely used treatment option for patients with subchondral bone marrow edema lesions which are considered a major source of pain in patients with OA [7–9, 12]. However, the 22 procedures performed at our institution showed only marginal success at short-term followup. Clinical success may be negatively skewed owing to high rates of coexisting osteochondral and meniscal disorders. However, there were several sources of bias in the design of a small retrospective study such as ours that would have been expected to inflate the apparent benefits of treatment. Future investigations of symptomatic bone marrow edema lesions might focus on patients with minimal osteochondral and meniscal damage to identify patients for whom this treatment may have a greater likelihood of success.
Compared with the asymptomatic population the prevalence of bone marrow edema lesions is greater in patients with increased Kellgren-Lawrence grade and subchondral bone may be a major contributor to OA pain [7–9, 12]. As expected, the preoperative Kellgren-Lawrence OA grade showed an inverse relationship to the postoperative Tegner Lysholm score. All but one of our patients with an outcome of clinical failure showed improvement in patient-reported outcome scores. Therefore, we do not believe that the injected material is the cause of clinical failure and progression of OA seems a more plausible explanation.
In our short-term review of outcomes after percutaneous calcium phosphate injection, we report a success rate of 55% at a median followup of 12 months postoperatively. In a study that would have been expected to present a best-case analysis (short-term followup, loss to followup of patients with potentially unfavorable outcomes, and use of invasive cotreatments including arthroscopic débridements), we found that percutaneous calcium phosphate injections in patients with advanced OA and symptomatic bone marrow edema lesions of the knee yielded unsatisfactory results in a concerning proportion of our patients. Therefore, we advise against the use of percutaneous calcium phosphate injections for patients with advanced osteoarthritic changes.
References
Abrams GD, Alentorn-Geli E, Harris JD, Cole BJ. Treatment of a lateral tibial plateau osteochondritis dissecans lesion with subchondral injection of calcium phosphate. Arthrosc Tech 2013;2:e271–274.
Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006;20:3–25.
Arjonilla A, Calvo E, Alvarez L, Fernandez Yruegas D. Transient bone marrow oedema of the knee. Knee. 2005;12:267–269.
Berger CE, Kroner AH, Kristen KH, Grabmeier GF, Kluger R, Minai-Pour MB, Leitha T, Engel A. Transient bone marrow edema syndrome of the knee: clinical and magnetic resonance imaging results at 5 years after core decompression. Arthroscopy 2006;22:866–871.
Brem MH, Schlechtweg PM, Bhagwat J, Genovese M, Dillingham MF, Yoshioka H, Lang P. Longitudinal evaluation of the occurrence of MRI-detectable bone marrow edema in osteoarthritis of the knee. Acta Radiol. 2008;49:1031–1037.
Cohen SB, Sharkey PF. Surgical treatment of osteoarthritis pain related to subchondral bone defects or bone marrow lesions: subchondroplasty. Tech Knee Surg. 2012;11:170–175.
Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, Kazis L, Gale DR. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–549.
Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, Torner J, Lewis CE, Nevitt MC. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–2992.
Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–456.
Gupta AC, Chandra RV, Yoo AJ, Leslie-Mazwi TM, Bell DL, Mehta BP, Vanderboom TL, Rabinov JD, Larvie M, Hirsch JA. Safety and effectiveness of sacroplasty: a large single-center experience. AJNR Am J Neuroradiol. 2014;35:2202–2206.
Hunter DJ, Zhang Y, Niu J, Goggins J, Amin S, LaValley MP, Guermazi A, Genant H, Gale D, Felson DT. Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum. 2006;54:1529–1535.
Koo KH, Ahn IO, Kim R, Song HR, Jeong ST, Na JB, Kim YS, Cho SH. Bone marrow edema and associated pain in early stage osteonecrosis of the femoral head: prospective study with serial MR images. Radiology. 1999;213:715–722.
Kornaat PR, Van de Velde SK. Bone marrow edema lesions in the professional runner. Am J Sports Med. 2014;42:1242–1246.
Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum. 2005;52:1730–1735.
LeGeros RZ. Properties of osteoconductive biomaterials: calcium phosphates. Clin Orthop Relat Res. 2002;395:81–98.
Li X, Ma BC, Bolbos RI, Stahl R, Lozano J, Zuo J, Lin K, Link TM, Safran M, Majumdar S. Quantitative assessment of bone marrow edema-like lesion and overlying cartilage in knees with osteoarthritis and anterior cruciate ligament tear using MR imaging and spectroscopic imaging at 3 Tesla. J Magn Reson Imaging. 2008;28:453–461.
Mitsou A, Vallianatos P, Piskopakis N, Maheras S. Anterior cruciate ligament reconstruction by over-the-top repair combined with popliteus tendon plasty. J Bone Joint Surg Br. 1990;72:398–404.
Mont MA, Baumgarten KM, Rifai A, Bluemke DA, Jones LC, Hungerford DS. Atraumatic osteonecrosis of the knee. J Bone Joint Surg Am. 2000;82:1279–1290.
Mont MA, Tomek IM, Hungerford DS. Core decompression for avascular necrosis of the distal femur: long term followup. Clin Orthop Relat Res. 1997;334:124–130.
Mrosek EH, Lahm A, Erggelet C, Uhl M, Kurz H, Eissner B, Schagemann JC. Subchondral bone trauma causes cartilage matrix degeneration: an immunohistochemical analysis in a canine model. Osteoarthritis Cartilage. 2006;14:171–178.
Nico B, Mangieri D, Benagiano V, Crivellato E, Ribatti D. Nerve growth factor as an angiogenic factor. Microvasc Res. 2008;75:135–141.
Papadopoulos EC, Papagelopoulos PJ, Kaseta M, Themistocleous GS, Korres DS. Bone marrow edema syndrome of the knee: a case report and review of the literature. Knee. 2003;10:295–302.
Sharkey PF, Cohen SB, Leinberry CF, Parvizi J. Subchondral bone marrow lesions associated with knee osteoarthritis. Am J Orthop. 2012;41:413–417.
Sharkey PF, Leinberry CF, Cohen SB, Bagga CS, Erbe EM. Subchondral treatment of joint pain. US patent application US 20110125157 A1. Available at: https://www.google.com/patents/US20110125157. Accessed March 31, 2015.
Sowers MF, Hayes C, Jamadar D, Capul D, Lachance L, Jannausch M, Welch G. Magnetic resonance-detected subchondral bone marrow and cartilage defect characteristics associated with pain and X-ray-defined knee osteoarthritis. Osteoarthritis Cartilage. 2003;11:387–393.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49.
Theologis AA, Kuo D, Cheng J, Bolbos RI, Carballido-Gamio J, Ma CB, Li X. Evaluation of bone bruises and associated cartilage in anterior cruciate ligament-injured and -reconstructed knees using quantitative t(1ρ) magnetic resonance imaging: 1-year cohort study. Arthroscopy. 2011;27:65–76.
Voormolen MH, van Rooij WJ, van der Graaf Y, Lohle PN, Lampmann LE, Juttmann JR, Sluzewski M. Bone marrow edema in osteoporotic vertebral compression fractures after percutaneous vertebroplasty and relation with clinical outcome. AJNR Am J Neuroradiol. 2006;27:983–988.
Walsh DA, McWilliams DF, Turley MJ, Dixon MR, Franses RE, Mapp PI, Wilson D. Angiogenesis and nerve growth factor at the osteochondral junction in rheumatoid arthritis and osteoarthritis. Rheumatology (Oxford). 2010;49:1852–1861.
Wluka AE, Wang Y, Davies-Tuck M, English DR, Giles GG, Cicuttini FM. Bone marrow lesions predict progression of cartilage defects and loss of cartilage volume in healthy middle-aged adults without knee pain over 2 yrs. Rheumatology (Oxford). 2008;47:1392–1396.
Acknowledgments
We thank Ramesh H. Gidumal MD and Andrew J. Feldman MD (Orthopaedic Surgery, Sports Division, NYU Langone Medical Center) for helping us build our patient cohort and Steven Shamah BA (Orthopaedic Surgery, Sports Division, NYU Langone Medical Center) for assistance in data gathering and analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Chatterjee, D., McGee, A., Strauss, E. et al. Subchondral Calcium Phosphate is Ineffective for Bone Marrow Edema Lesions in Adults With Advanced Osteoarthritis. Clin Orthop Relat Res 473, 2334–2342 (2015). https://doi.org/10.1007/s11999-015-4311-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4311-0