Abstract
Background
More than 15,000 primary hip resurfacing arthroplasties have been recorded by the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) with 884 primary procedures requiring revision for reasons other than infection, a cumulative percent revision rate at 12 years of 11%. However, few studies have reported the survivorship of these revision procedures.
Questions/purposes
(1) What is the cumulative percent rerevision rate for revision procedures for failed hip resurfacings? (2) Is there a difference in rerevision rate among different types of revision or bearing surfaces?
Methods
The AOANJRR collects data on all primary and revision hip joint arthroplasties performed in Australia and after verification against health department data, checking of unmatched procedures, and subsequent retrieval of unreported procedures is able to obtain an almost complete data set relating to hip arthroplasty in Australia. Revision procedures are linked to the known primary hip arthroplasty. There were 15,360 primary resurfacing hip arthroplasties recorded of which 884 had undergone revision and this was the cohort available to study. The types of revisions were acetabular only, femoral only, or revision of both acetabular and femoral components. With the exception of the acetabular-only revisions, all revisions converted hip resurfacing arthroplasties to conventional (stemmed) total hip arthroplasties (THAs). All initial revisions for infection were excluded. The survivorship of the different types of revisions and that of the different bearing surfaces used were estimated using the Kaplan-Meier method and compared using Cox proportional hazard models. Cumulative percent revision was calculated by determining the complement of the Kaplan-Meier survivorship function at that time multiplied by 100.
Results
Of the 884 revisions recorded, 102 underwent further revision, a cumulative percent rerevision at 10 years of 26% (95% confidence interval, 19.6–33.5). There was no difference in the rate of rerevision between acetabular revision and combined femoral and acetabular revision (hazard ratio [HR], 1.06 [0.47–2], p = 0.888), femoral revision and combined femoral and acetabular revision (HR, 1.00 [0.65–2], p = 0.987), and acetabular revision and femoral revision (HR, 1.06 [0.47–2], p = 0.893). There was no difference in the rate of rerevision when comparing different bearing surfaces (metal-on-metal versus ceramic-on-ceramic HR, 0.46 [0.16–1.29], p = 0.141; metal-on-metal versus ceramic-on-crosslinked polyethylene HR, 0.51 [0.15–1.76], p = 0.285; metal-on-metal versus metal-on-crosslinked polyethylene HR, 0.62 [0.20–1.89], p = 0.399; and metal-on-metal versus oxinium-on-crosslinked polyethylene HR, 0.53 [0.14–2.05], p = 0.356).
Conclusions
Revision of a primary hip resurfacing arthroplasty is associated with a high risk of rerevision. This study may help surgeons guide their patients about the outcomes in the longer term after the first revision of hip resurfacing arthroplasty.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Hip resurfacing arthroplasty was introduced as a result of the theoretical advantages, particularly in younger patients, of bone conservation, restoration of proximal femoral anatomy, reduced wear, and ease of future revision. In 2005, resurfacings represented 9% of all primary THAs performed in Australia [1]. Higher than expected rates of revision for hip resurfacing arthroplasty were first reported in the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) Annual Report in 2007 [2]. Subsequent reports have confirmed this [7, 8, 10, 12]. In Australia, the proportion of hip resurfacing arthroplasty as a percentage of all primary THAs has declined to 2% and most procedures are performed on men younger than 65 years of age [4]. There were some early fractures of the femoral neck with the Birmingham HRA (Smith & Nephew, Bromsgrove, UK) and this led to the development of a conventional large-head metal-on-metal (MoM) THA prosthesis that could be used for revision of these fractures. Many other manufacturers introduced large-head MoM conventional THAs and higher rates of revision have been reported for this bearing surface [6–8, 13].
A previous report detailed the early outcome of revised hip resurfacing arthroplasty [5]. In light of recent data confirming a high rate of revision for large-diameter MoM THAs, the aims of this study were to review the outcome of revision procedures for failed hip resurfacings and to determine if there were differences depending on the type of bearing surface used at the time of revision.
We therefore asked: (1) What is the cumulative percent rerevision rate for revision procedures for failed hip resurfacings? (2) Is there a difference in rerevision rate among different types of revision or bearing surfaces?
Materials and Methods
The AOANJRR started data collection in September 1999 and achieved full national coverage in 2002. All hospitals in Australia provide data on primary and revision joint arthroplasty through forms filled out at the time of surgery. Procedures reported to the registry are crossvalidated with independently collected state health department data in a sequential multilevel matching process, which enables almost 100% data collection. Data are also matched biannually with the Department of Health and Aging’s National Death Index to obtain information on the date of death.
Data were collected on all revision procedures performed for primary hip resurfacing arthroplasty and repeat revision procedures performed on those hips between September 1, 1999, and December 31, 2012. For the analysis, only primary hip resurfacing arthroplasties performed with a diagnosis of osteoarthritis were included. The registry records reasons for revision of both the primary and revision arthroplasty. Revisions that the surgeon recorded as being related to issues with reaction to metal were initially recorded as metal sensitivity and changed in 2012 to metal-related pathology. All initial revisions for infection were excluded. Revision procedures were classified as acetabular only, femoral only, and combined acetabular and femoral. With the exception of the acetabular-only revisions, all revisions converted failed hip resurfacing arthroplasty to conventional (stemmed) THAs. The outcomes of the bearing surface listed in the latter group were also analyzed.
The registry uses Kaplan-Meier estimates of survivorship to describe the time to the first revision of an arthroplasty with censoring at the time of death or closure of the database at the time of analysis. The unadjusted cumulative percent revision at the end of each of the first 10 years after the revision arthroplasty, with an accompanying 95% confidence interval (CI), was calculated with use of unadjusted pointwise Greenwood estimates. Cumulative percent revision was calculated by determining the complement of the Kaplan-Meier survivorship function at that time multiplied by 100. Hazard ratios were calculated using Cox proportional hazards models adjusting for age and sex and were used to compare the rate of revision between groups. The assumption of proportional hazards was checked analytically for each model; if the interaction between the predictor and the log of the postoperative time was significant in the standard Cox model, then a time-varying model was used. All tests were two-tailed at the 5% of level of significance. Statistical analysis was performed using SAS Version 9.3 software (SAS Institute Inc, Cary, NC, USA).
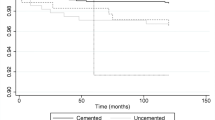
Between September 1, 1999, and December 31, 2012, 15,360 primary resurfacing hip arthroplasties were reported to the AOANJRR with a cumulative percent revision at 12 years of 11% (Fig. 1). The DePuy ASR (Warsaw, IN, USA) was not excluded, with 1167 recorded, 8% of all primary hip resurfacing arthroplasties. Of these 15,360 hip resurfacing arthroplasties, 1050 have been revised. After excluding revisions for infection and revisions in which the primary diagnosis for resurfacing was not osteoarthritis, 884 revision procedures remained for analysis for this study. For these 884 hip resurfacing arthroplasty revision procedures, the most common reasons for the initial revision were loosening and/or osteolysis, metal-related pathology, and fracture (Table 1). Of the 884 revision procedures (in 850 patients), 12 patients have died (1.4%).
The most common type of revision involved replacement of both the acetabular and femoral components (61%) followed by femoral only (35%) and acetabular only (4%). A wide variety of cemented and cementless revision prostheses was used. With the exception of the acetabular-only revisions, all revisions converted hip resurfacing arthroplasties to conventional (stemmed) THAs. All acetabular-only revisions were revised to a hip resurfacing arthroplasty.
The registry recorded 537 femoral/acetabular revisions. These revisions used 98 different stem/cup prosthesis combinations. The most common reason for revision was loosening and/or osteolysis (40%) followed by metal-related pathology (35%) (Table 1). The most commonly used bearing surface was ceramic-on-ceramic, used in 286 revision procedures, 48 with a ceramic head size 40 mm or larger. Ninety-five revision procedures used ceramic-on-crosslinked polyethylene, nine of which used a head size greater than 40 mm, and 82 used metal-on-crosslinked polyethylene, of which five had a head size greater than 40 mm. Fourteen revision procedures continued to use a MoM articulation, seven with a head size greater than 40 mm.
Three hundred ten femoral-only revisions were reported. The majority (62%) was undertaken to treat a femoral neck fracture (Table 1). Over 50 different femoral stems were used. In the femoral-only revisions, seven used a ceramic head, producing a ceramic-on-metal articulation. The remainder of the femoral-only revisions used large metal heads on a conventional stemmed implant.
There were 37 acetabular-only revisions of failed primary hip resurfacing reported to the registry. All acetabular-only revisions were revisions to another hip resurfacing arthroplasty. Six different cups were used with the Birmingham Hip being the most frequently used. The majority of these revisions (22) were undertaken for loosening and/or osteolysis with a further eight for component malpositioning (Table 1).
Results
Rerevision Rate for Revisions of Failed Total Hip Resurfacing Arthroplasties
Of the 884 revision procedures, 102 have undergone a further revision. The cumulative percent rerevision at 10 years is 26% (95% CI, 20–34) (Fig. 1). The most common diagnoses for repeat revision surgery were loosening and/or osteolysis, metal-related pathology, infection, and prosthesis dislocation (Table 2).
Difference in Rerevision Rate Among Different Revision Types and Bearing Surfaces
With the numbers available, there was no difference in cumulative percent rerevision rate among the types of revision (femoral only, acetabular only, or combined acetabular and femoral) or the bearing surface used in the index revision arthroplasty (ceramic-on-ceramic, metal-on-crosslinked polyethylene, metal-on-metal).
Revision Type
There was no difference in the rate of rerevision between acetabular revision and combined femoral and acetabular revision (hazard ratio [HR], 1.06 [0.47–2], p = 0.888; femoral revision and combined femoral and acetabular revision, HR, 1.00 [0.65–2], p = 0.987; and acetabular revision and femoral revision HR, 1.06 [0.47–2], p = 0.893; Table 3).
Thirty-seven acetabular-only revisions of failed primary hip resurfacing were reported to the registry, of which seven underwent a further revision. Although these numbers are relatively small, they represent a cumulative percent rerevision at 10 years of 20% (95% CI, 10–38). Five patients underwent a further revision replacing both the acetabular component and adding a femoral stem, and two had the femoral components revised (Table 4).
The registry recorded 310 femoral-only revisions with 51 undergoing a further revision, a cumulative percent rerevision at 10 years of 25% (95% CI, 18–35). Of these patients, 30 underwent a further revision of the acetabular component, eight both femoral and acetabular components, and six femoral components only (Table 4).
Of the 537 combined femoral and acetabular revisions for failed resurfacings, 44 underwent a further revision with a cumulative percent rerevision at 10 years of 40% (95% CI, 21–66).
Bearing Surface
There was no difference in the rate of rerevision between metal-on-metal and other bearing surfaces used in the first revision (ceramic-on-ceramic HR, 0.46 [0.16–1.29], p = 0.141; ceramic-on-crosslinked polyethylene HR, 0.51 [0.15–1.76], p = 0.285; metal-on-crosslinked polyethylene HR, 0.62 [0.20–1.89], p = 0.399; and oxinium-on-crosslinked polyethylene HR, 0.53 [0.14–2.05], p = 0.356) (Table 5).
The most common bearing surface, ceramic-on-ceramic, had a 10-year cumulative percent rerevision rate of 14% (95% CI, 7–25). Of the 14 revisions using a MoM bearing surface, five have undergone a further revision, a cumulative percent rerevision at 10 years of 67% (95% CI, 25–98). Four of these five rerevisions were performed for metal-related pathology, whereas there were no revisions performed for this diagnosis with other bearing surfaces.
Discussion
At the peak of their popularity, hip resurfacing arthroplasties represented 9% of all primary hip arthroplasties performed in Australia in 2005 [1] and 10% in England and Wales in 2006 [8]. In light of the higher-than-expected revision rates reported for hip resurfacing arthroplasty [2, 7, 8, 10, 12], these patients represent a substantial revision burden. In 2012 the AOANJRR reported the first-ever increase in the number of revision hips being performed in Australia, a rise caused by the revision burden of hip resurfacing arthroplasty and metal-on-metal THA [3]. There have been few articles reporting the survivorship of these procedures [9, 12, 13]. Our findings show a cumulative percent rerevision rate of 26% in revision procedures undertaken for failed hip resurfacing arthroplasty. We found no differences in survivorship across the types of revision or bearing surfaces used at revision.
This study has some limitations. Although reporting the findings of 884 revisions in over 15,000 hip resurfacing arthroplasties, there were no differences in survivorship observed with the numbers available across the different types of revision and bearing surfaces at 10 years. It is likely that even larger numbers of procedures are required to determine if there are any differences. We have also not reviewed survivorship of revisions based on surgical approach of the primary and revision procedure or based on the make of the primary resurfacing implant. Both could be the subject of further study. The revision diagnosis is recorded at the time of surgery and it is possible that infection is overrecorded as a result of the effusion and soft tissue problems associated with the MoM bearing surface. As a result, some revision procedures may have been unnecessarily excluded. Similarly, metal-related pathology may also be misinterpreted as loosening and/or osteolysis. We have therefore not reviewed survivorship of revisions based on indication for revision. Pseudotumors were recorded as the reason for revision in 14 of the 884 revisions, but the extent of soft tissue or bony destruction at the time of the revision procedure is not known. This would have had a bearing on what type of revision was performed and could influence the durability and rerevision rate of the procedure [6].
Our findings show a cumulative percent rerevision rate of 26% (95% CI, 20–34) at 10 years in revision procedures undertaken for failed hip resurfacing arthroplasty. In comparison the cumulative percent revision rate at 10 years for primary THA in the AOANJRR is 7% (95% CI, 6.6–7.0). Few other studies have investigated the long-term survivorship of revision for hip resurfacing arthroplasty. A previous study by the AOANJRR in 2010 [5] looked at the early rerevision rate of 397 revisions for reasons other than infection, finding a cumulative percent rerevision rate of 9% at 5 years. This current analysis has been performed on more than twice the number of revision procedures with a longer followup. We did confirm findings in this previous study that, although infection is an uncommon cause of the first revision of a hip resurfacing arthroplasty, it is the third most common cause for the rerevision accounting for 19 of the 102 revisions (19%). One of the theoretical advantages of a hip resurfacing arthroplasty is that retention of the proximal femur enables ease of revision. Although this may be technically correct with regard to the femoral component, there is no evidence that this leads to a better outcome. Revision of the acetabulum can be difficult. Previous series have shown that the acetabular components are rarely loose at revision and, if revised to avoid a further MoM bearing, may risk excessive acetabular bone loss [11].
Our findings did not show a difference among femoral only, acetabular only, and combined femoral and acetabular revision procedures. This was also studied by the previously mentioned AOANJRR paper [5], which reported that acetabular-only revision had a significantly higher risk of revision compared with femoral-only revision but not among the other groups (a 5-year cumulative percent revision rate of 20%, 7%, and 5%). Grammatopoulos et al. [6] identified 53 hips in 51 patients that had undergone revision surgery after hip resurfacing arthroplasty, of which 16 were revised for pseudotumor formation. This group found that revision for pseudotumor had poorer functional outcomes than matched primary hip arthroplasties with a higher incidence of major complications. Five of these 16 patients required further revision with three found to have recurrent pseudotumors. Pritchett [9] reported on a series of 90 single-component revisions of resurfacings failing as a result of adverse reactions to metal wear debris. This series of 76 acetabular-only and 14 femoral-only revisions demonstrated an improvement in Harris hip scores in all patients. Forty-three patients with a femoral head size greater than 46 mm underwent acetabular-only revisions using a MoM articulation, and 33 patients with smaller femoral heads were revised to metal-on-polyethylene using a 3.8-mm thick highly crosslinked polyethylene liner. Femoral-only revisions were performed using a dual mobility implant. The MoM acetabular-only revisions had three subsequent revisions after a mean followup of 65 months. No revisions were reported in the metal-on-polyethylene or the dual mobility group.
Full chronological data on revisions of resurfacings in large numbers are only likely to be obtained from a national registry. The strength of this study is that the AOANJRR is uniquely placed because it records information on the known primary procedure and subsequent revision and rerevision procedures. This study is based on over 15,000 primary hip resurfacing arthroplasties with a subsequent 884 revision procedures available for analysis. The registry has a capture rate approaching 100% of all procedures and is able to validate revisions linked to the known primary. There is also longer-term followup of greater than 10 years. This study has not investigated variables such as approach, type of implant, or patient body mass index that may affect the results of revision surgery. The results of this study suggest that revision of a primary hip resurfacing arthroplasty is associated with a high risk of rerevision. There was no difference in the rate of revision comparing different types of the initial revision and comparing different bearing surfaces used for the first revision. However, we would caution against the use of another MoM bearing as a result of the potential for further metal-related pathology.
References
Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2006. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/75132/Annual%20Report%202006?version=1.1&t=1349406762263. Accessed March 10, 2014.
Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2007. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/42612/Annual%20Report%202007?version=1.1&t=1349406300550. Accessed March 10, 2014.
Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2008. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/42662/Annual%20Report%202008?version=1.1&t=1349406277970. Accessed March 10, 2014.
Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2013. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/127202/Annual%20Report%202013?version=1.2&t=1385685288617. Accessed May 14, 2014.
de Steiger RN, Miller LN, Graves SE, Davidson DC, Stanford TE. Poor outcome of revised resurfacing hip arthroplasty. Acta Orthop. 2010;81:72–76.
Grammatopoulos G, Pandit H, Kwon YM, Gundle R, McLardy-Smith P, Beard DJ, Murray DW, Gill HS. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009;91:1019–1024.
Graves SE, Rothwell A, Tucker K, Jacobs JJ, Sedrakyan A. A multinational assessment of metal-on-metal bearings in hip replacement. J Bone Joint Surg Am. 2011;93(Suppl 3):43–47.
National Joint Registry for England and Wales 7th Annual Report 2010. Available at: www.njrcentre.org.uk/NjrCentre/Portals/0/NJR%207th%20Annual%20Report%202010.pdf. Accessed March 10, 2014.
Pritchett JW. One-component revision of failed hip resurfacing from adverse reaction to metal wear debris. J Arthroplasty 2014; 29:219–224.
Prosser GH, Yates PJ, Wood DJ, Graves SE, de Steiger RN, and Miller LN. Outcome of primary resurfacing hip replacement: evaluation of risk factors for early revision. Acta Orthop. 2010;81:66–71.
Sandiford NA, Muirhead-Allwood SK, Skinner JA. Revision of failed hip resurfacing to total hip arthroplasty rapidly relieves pain and improves function in the early post operative period. J Orthop Surg Res. 2010;5:88.
Smith AJ, Dieppe P, Howard PW, Blom AW. Failure rates of metal-on-metal hip resurfacings: analysis of data from the National Joint Registry for England and Wales. Lancet. 2012;380:1759–1766.
Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379:1199–1204.
Acknowledgments
We thank the AOANJRR and the hospitals, orthopaedic surgeons, and patients whose data made this work possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
The Australian Government funds the AOA NJRR through the Department of Health and Aging.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
The human protocol for this investigation and ethical approval for the AOA NJRR, through which the research was carried out, was provided through the minister of Health and Ageing for the Commonwealth of Australia.
About this article
Cite this article
Wong, J.ML., Liu, YL., Graves, S. et al. What Is the Rerevision Rate After Revising a Hip Resurfacing Arthroplasty? Analysis From the AOANJRR. Clin Orthop Relat Res 473, 3458–3464 (2015). https://doi.org/10.1007/s11999-015-4215-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4215-z