Abstract
Boden et al. suggested syndesmosis fixation was not necessary in distal pronation external rotation (PER) ankle fractures if rigid bimalleolar fracture fixation is achieved and was not necessary with deltoid ligament injury if the fibular fracture is no higher than 4.5 cm of the tibiotalar joint. We asked whether height of the fibular fracture with or without medial stability predicted syndesmotic instability as compared with intraoperative hook testing in these fractures. We reviewed 62 patients (35 male, 27 female) with a mean age of 45.6 years (range, 19–80 years). Using a bone hook applied to the distal fibula with lateral force to the distal fibula in the coronal plane, we fluoroscopically assessed the degree of syndesmosis diastasis in all patients. The mean height of the fibular fracture in patients with a positive hook test was higher than in patients with a negative hook test (54.2 mm; standard deviation [SD], 29.3 versus 34.8 mm; SD, 21.4, respectively). The height of the fibular fracture showed a positive predictive value of 0.93 and a negative predictive value of 0.53 in predicting syndesmotic instability; specificity of the criteria of Boden et al. was high (0.96). However, sensitivity was low (0.39) using the hook test as the gold standard. The criteria of Boden et al. may be helpful in planning, but may have some limitations as a predictor of syndesmotic instability in distal PER ankle fractures.
Level of Evidence: Level III, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle fractures are among the most common injuries treated by orthopaedic surgeons. Some ankle fractures are associated with syndesmotic injury and an interosseous membrane rupture. The distal tibiofibular syndesmosis consists of a complex of ligaments that provide stability to the distal tibiofibular joint. The anterior and posterior tibiofibular ligaments, together with the interosseous ligament form the syndesmosis, and the inferior transverse tibiofibular ligament is sometimes considered a fourth ligament, but this is a continuation of the posterior tibiofibular ligament. The interosseous membrane and the medial deltoid ligament add further stability to the ankle mortise [10].
The need for distal tibiofibular syndesmotic fixation after ankle fractures remains controversial despite the abundance of literature concerning the treatment of ankle fractures [23]. We believe syndesmotic stability should be restored in such combined injuries [14]. Many surgeons do not perform an open reduction and internal fixation of fractures in the proximal third of the fibula, but rather place one or two syndesmotic screws instead because of the risk of peroneal nerve injury [8, 21, 23]. The published guidelines for use of a syndesmotic screw in more distal fractures (Weber C fracture of the medial malleolus or deltoid ligament rupture associated with anterior tibiofibular ligament disruption and fibular fracture above the joint) are both conflicting and vague [3, 15, 18]. The syndesmotic screw or other stabilizing techniques all effectively stabilize the distal tibiofibular syndesmosis to allow ligamentous healing or fibrous union [24]. Placement of a syndesmotic screw is not without complications and requires an additional operation for removal of the screw. Therefore, it is important to clearly identify which patients will benefit from distal tibiofibular syndesmotic fixation.
The clinical diagnosis of syndesmosis disruption is insensitive and nonspecific in acute ankle fractures because many patients cannot localize the tender spot at the syndesmosis. Radiographic measurements such as tibiofibular overlap and medial and superior clear space are of little value in detecting syndesmotic injury [1]; even additional quantitative measurement of all syndesmotic parameters with repeated radiographs of the ankle are of little value [1, 17]. Boden et al. developed radiographic criteria to predict the need for syndesmotic fixation based on cadaveric ankles [2]. They suggested when rigid medial fixation is achieved, no syndesmotic stabilization is required in the absence of rigid medial fixation if the height of the fibular fracture of more than 4.5 cm above the joint line requires syndesmotic stabilization. These criteria, depending on the proximity of the fibular fracture, suggest a limited rather than routine use of supplemental syndesmotic fixation [15]. These criteria have been confirmed by Yamaguchi et al. [26] and Chissell and Jones [5] in clinical studies of Weber C fractures. Yamaguchi et al. [26] evaluated patients treated according to the criteria of Boden et al. [2] and evaluated syndesmotic stability after 1 to 3 years in those not receiving syndesmotic fixation; their data suggested use of the Boden criteria resulted in no late syndesmotic instability. Chissel and Jones [5] reviewed patients treated by an intraoperative decision and compared that decision with one using the criteria of Boden et al.; they reported 1.6 times more syndesmotic screws were placed based on intraoperative decision than would have been used using the criteria of Boden et al. [2]. Both authors suggested the criteria of Boden et al. are the “gold standard,” although their data could be interpreted to suggest otherwise since the decision on which syndesmotic stabilization is performed is not clarified: they were merely testing whether their decision-making conformed with the Boden criteria and not the validity of the Boden criteria [2]. Currently, then, the recommendations for syndesmotic fixation based on the level of the fibular fracture have been based on one cadaveric study and two small clinical series (Table 1) [2, 5, 26].
We therefore had two objectives: (1) to compare the height of the fibular fractures in ankles with distal tibiofibular syndesmotic instability with the height of the fibular fracture of the ankles with a stable syndesmosis; and (2) to determine the sensitivity and specificity of the criteria of Boden et al. [2] using the hook test as the gold standard for assessing instability [11] in distal pronation external rotation (PER) ankle fractures.
Materials and Methods
Using our comprehensive prospective database, we retrospectively identified 219 skeletally mature patients who had surgery for an ankle fracture between August 2004 and May 2008. We excluded patients with multiple and high-energy trauma. With these exclusions, from the 219 patients, we identified 62 (62 ankles) who had a distal pronation external rotation ankle fracture [13] (within 150 mm of the tibiotalar joint) and all were included in the study. The mean age of the patients was 45.6 years (range, 19–80 years). The study population included 35 men and 27 women. Approval of this study by the Institutional Review Board was not necessary because this was a retrospective study.
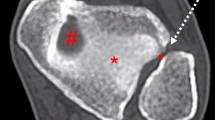
Patients were treated by attending orthopaedic surgeons and trauma surgeons experienced with the AO/ASIF principles of anatomic reduction and internal fixation [25]. The deltoid ligament was not repaired; in case of medial interposition prohibiting adequate reposition, medial exploration was performed. Syndesmotic instability probably occurs in the coronal, sagittal, rotational, and axial planes, but only the coronal and rotational plane instabilities are routinely addressed clinically. To examine for instability under fluoroscopic control, we performed the hook test (Cotton test) first described by Frederic J. Cotton in 1910 [7] (Fig. 1). With intraoperative anteroposterior stress radiography and using a bone hook applied to the distal fibula and applying lateral force to the distal fibula in the coronal plane, the degree of syndesmosis diastases can be assessed by using an image intensifier. Lateral movement of the fibula or widening of the mortise on intraoperative radiographs were considered a positive finding. Both for lateral movement and widening of the mortise, there is no consensus; the judgment whether it is unstable or stable is to be made by the surgeon. This test suggests if there is widening in the coronal plane in a mortise view, instability of the syndesmosis is present [20].
We used conventional stainless cortical syndesmotic screws. The screws were inserted in a neutral or slightly dorsiflexed position of the ankle. There was no uniform protocol regarding the fixation technique because of the lack of evidence for selecting screw diameter, one versus two screws, fixation with three versus four cortices, distance between screw and tibiotalar joint, fixation with a dorsiflexed ankle, time of removal of the screw, and weightbearing regime [22]. Thirty-six of the 62 ankles had syndesmotic fixation after hook testing [11]. In 26 ankles, one screw was inserted; in 10, two screws; in 25, three cortex fixation was performed and in 11, four cortex fixation. We removed all syndesmotic screws before unprotected weightbearing at 6 to 12 weeks. A medial malleolar fracture occurred in 24 of 62 patients. All patients had anatomic reduction and fixation of this fracture with two screws or one screw and a Kirschner wire. Of the 24 patients with medial malleolar fractures, four had only a fracture of the anterior part of the medial malleolus with a ruptured (posterior) deep posterior part of the deltoid ligament. In these patients, an open reduction and internal fixation of the fracture was performed and according to the hook test, syndesmotic stabilization was performed. In 11 of the 24 patients with a medial malleolar fracture, we stabilized the syndesmosis. Seventeen patients had a posterior malleolar fracture; nine of these fractures were fixed. Five patients had a fixed posterior malleolar fracture in the hook test stable group and four patients in the hook test unstable group. One patient had a fibular fracture (greater than 45 mm above the joint), a deltoid ligament injury, a fixed posterior malleolar fracture, and a negative hook test.
Two of us (MB, DH) measured the height of the fibular fracture using a digital radiograph displayer. The height was defined as the distance from the most distal part of the fracture to the tibiotalar joint line. During the operation, the stability of the syndesmosis was evaluated using the hook test after fixation of the malleolar fractures (Fig. 1).
Boden et al. [2] performed a cadaveric study investigating the biomechanical considerations for the need for syndesmotic fixation. They studied 35 cadaveric ankles with pronation-external rotation (Weber C) ankle fractures. They assumed the interosseous membrane is disrupted to the level of the fibular fracture. They concluded either an intact deltoid ligament or an intact interosseous membrane provided enough stability to the syndesmosis once rigid medial malleolar and fibular fixation was achieved to prevent distal tibiofibular diastasis. They further concluded syndesmotic fixation in ankle fractures was not necessary if rigid bimalleolar fracture fixation was achieved, and finally no syndesmotic stabilization was needed in case of fibular fracture fixation without a medial malleolar fracture (only deltoid ligament injury) if the fibular fracture was within 45 mm of the tibiotalar joint.
We compared the mean height of the fibular fracture for a positive hook test with 95% confidence interval to the height of the fibular fracture of those not having syndesmotic stabilization using an analysis of variance test with an alpha level of 0.05. Sensitivity and specificity of the criteria of Boden et al. [2] were calculated. SPSS 16.0 for Windows software (SPSS Inc, Chicago, IL) was used for the analyses.
Results
The mean height of the fibular fracture in patients with a positive hook test was greater (p = 0.006) than of patients with a negative hook test (54.2 mm ± 29.3 mm versus 34.8 ± 21.4 mm, respectively) (Fig. 2).
Using the Boden criteria (fibular fracture of 4.5 cm above the joint line as the cutoff point in those without rigid medial fixation or those with rigid medial fixation) against the hook test as the “gold standard,” there were 25 true-negatives, 22 false-negatives, 14 true-positives, and one false-positive. This led to a sensitivity of 0.39, a specificity of 0.96, a negative predictive value of 0.53, and a positive predictive value of 0.93 for the criterion of Boden et al. [2].
Discussion
Boden et al. [2] stated syndesmotic fixation was not necessary in distal PER ankle fractures if rigid bimalleolar fracture fixation was achieved and not necessary with deltoid ligament injury if the fibular fracture was within 4.5 cm of the tibiotalar joint. Because height of the fibular fracture seems an important predictor for syndesmotic stability in distal PER fractures, we evaluated the height of the fibular fracture between stable and unstable syndesmotic injuries. The criteria of Boden et al. [2] were compared with the hook test we regard as the gold standard. The accuracy of these preoperative criteria in predicting the syndesmotic instability was evaluated.
Potential biases in this study include the interpretation of the intraoperative hook test. It is not clear how much displacement is required to detect instability, how much force should be applied to the fibula, and in which exact direction it should be pulled [4]. We performed only the hook test and used no external rotation testing to predict syndesmotic instability. Although there remains much to be standardized and investigated regarding syndesmotic instability and its quantification, we believe the Hook test is the gold standard, because it is nothing more than testing the stability by providing stress on the structure to be judged.
By judging the height of the fibular fracture, one assumes the interosseous membrane (an important stabilizer of the ankle syndesmosis, particularly in the presence of deltoid ligament insufficiency) is ruptured until height [2, 5, 6, 16]. Based on this assumption, Boden et al. [2] and Kennedy et al. [12] reported fractures 3 cm to 4.5 cm (Boden et al.) or 5 cm (Kennedy et al.) proximal to the ankle have syndesmotic instability. However, Nielson et al. compared the level of the fibular fracture with the integrity or extent of the interosseous membrane tears on MRI in 73 operative ankle fractures [18]. In one of three of the patients, the tears did not correlate with the level of the fractured fibula. Nielson et al. suggested one could not consistently estimate the integrity of the interosseous membrane and subsequent need for syndesmotic fixation based solely on the level of the fibular fracture [19], which could explain our outcome instability cannot be predicted from radiographic analysis (eg, using the Boden criteria).
When determining the accuracy of the Boden criteria, it is important to define when rigid medial fixation is achieved. This medial injury may be an osseous avulsion, leaving the deltoid intact on the displaced fragment, or it may be a combination of ligamentous and osseous injury with disruption of the deep portion of the deltoid ligament. Therefore, it is important to discriminate between these lesions, which we did in our study. There were 11 patients with a medial malleolar fracture; four of them had only a fracture of the anterior part in which an additional deltoid ligament could be expected and rigid medial fixation after open reduction and internal fixation (which all underwent) cannot be assumed.
Consistent with recent literature, we suggest general radiographic criteria for syndesmotic fixation are of low value compared with the intraoperative impression of the syndesmotic stability in all operated ankles [1, 9, 17]. Preoperative planning is essential but not sufficient to determine the necessity for syndesmotic fixation. We recommend the criteria of Boden et al. [2] be used only as a guide in the diagnosis and management of syndesmotic instability associated with ankle fractures and not solely relied on for treatment decisions. Factors influencing the choice of fixation include the presence of posterior malleolus fractures, deltoid ligament injuries, and subluxation of the fibula [10]. Whenever the surgeon is in doubt about syndesmotic instability, we believe fixation of the distal tibiofibular joint should be performed [23].
References
Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, Swierstra BA. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;423:227–234.
Boden SD, Labropoulos PA, McCowin P, Lestini WF, Hurwitz SR. Mechanical considerations for the syndesmosis screw. A cadaver study. J Bone Joint Surg Am. 1989;71:1548–1555.
Burwell HN, Charnley AD. The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement. J Bone Joint Surg Br. 1965;47:634–660.
Candal-Couto JJ, Burrow D, Bromage S, Briggs PJ. Instability of the tibiofibular syndesmosis: have we been pulling in the wrong direction? Injury. 2004;35:814–818.
Chissell HR, Jones J. The influence of a diastasis screw on the outcome of Weber type-C ankle fractures. J Bone Joint Surg Br. 1995;77:435–438.
Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am. 1956;38:761–781.
Cotton FJ. Fractures and Joint Dislocations. Philadelphia, PA: WB Saunders; 1910:549.
Duchesneau S, Fallat LM. The Maisonneuve fracture. J Foot Ankle Surg. 1995;34:422–428.
Ebraheim NA, Elgafy H, Padanilam T. Syndesmotic disruption in low fibular fractures associated with deltoid ligament injury. Clin Orthop Relat Res. 2003;409:260–267.
Ebraheim NA, Taser F, Shafiq Q, Yeasting RA. Anatomical evaluation and clinical importance of the tibiofibular syndesmosis ligaments. Surg Radiol Anat. 2006;28:142–149.
Jenkinson RJ, Sanders DW, Macleod MD, Domonkos A, Lydestadt J. Intraoperative diagnosis of syndesmosis injuries in external rotation ankle fractures. J Orthop Trauma. 2005;19:604–609.
Kennedy JG, Soffe KE, Dalla Vedova P, Stephens MM, O’Brien T, Walsh MG, McManus F. Evaluation of the syndesmotic screw in low Weber C ankle fractures. J Orthop Trauma. 2000;14:359–366.
Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60:957–985.
Leeds HC, Ehrlich MG. Instability of the distal tibiofibular syndesmosis after bimalleolar and trimalleolar ankle fractures. J Bone Joint Surg Am. 1984;66:490–503.
Lindsjö U. Operative treatment of ankle fractures. Acta Orthop Scand Suppl. 1981;189:1–131.
Minns RJ, Hunter JAA. The mechanical and structural characteristics of the tibiofibular interosseous membrane. Acta Orthop Scand. 1976;47:236–240.
Nielson JH, Gardner MJ, Peterson MG, Sallis JG, Potter HG, Helfet DL, Lorich DG. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;436:216–221.
Nielson JH, Sallis JG, Potter H, Helfet DL, Lorich DG. Correlation of interosseous membrane tears to the level of fibular fracture. J Orthop Trauma. 2004;18:68–74.
Purvis GD. Displaced unstable ankle fractures: classification, incidence and management of a consecutive series. Clin Orthop Relat Res. 1982;165:91–98.
Solomon L, Warwick DJ, Nayagam S. Apley’s System of Orthopaedics and Fractures. 8th Ed. London, UK: Arnold; 2001.
Sproule JA, Khalid M, O’Sullivan M, McCabe JP. Outcome after surgery for Maisonneuve fracture of the fibula. Injury. 2004;35:791–798.
Van den Bekerom MP, Hogervorst M, Bolhuis HW, van Dijk CN. Operative aspects of the syndesmotic screw: review of current concepts. Injury. 2008;39:491–498.
Van den Bekerom MPJ, Lamme B, Hogervorst M, Bolhuis HW. Which ankle fractures require syndesmotic stabilization? J Foot Ankle Surg. 2007;46:456–463.
Van den Bekerom MPJ, Raven EEJ. Current concepts review: operative techniques for stabilizing the distal tibiofibular syndesmosis. Foot Ankle Int. 2007;28:1302–1308.
BG, Colton Ch. Malleolar fractures. In: Müller ME, Allgöwer M, Schneider R, Willenegger H, Perren SM, eds. Manual of Internal Fixation: Techniques Recommended by the AO/ASIF Group. Berlin, Germany: Springer-Verlag; 1991:595–612.
Yamaguchi K, Martin CH, Boden SD, Labropoulos PA. Operative treatment of syndesmotic disruptions without use of a syndesmotic screw: a prospective clinical study. Foot Ankle Int. 1994;15:407–414.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) might pose a conflict of interest in connection with the submitted article.
Each author certifies his or her institution has approved the human protocol for this investigation, all investigations were conducted in conformity with ethical principles of research, and informed consent for participation in the study was obtained.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
van den Bekerom, M.P.J., Haverkamp, D., Kerkhoffs, G.M.M.J. et al. Syndesmotic Stabilization in Pronation External Rotation Ankle Fractures. Clin Orthop Relat Res 468, 991–995 (2010). https://doi.org/10.1007/s11999-009-0823-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-0823-9