Opinion statement
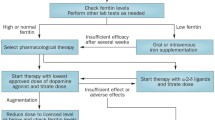
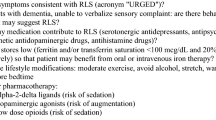
Restless legs syndrome (RLS) is a common, sensorimotor, circadian sleep disorder characterized by the urge to move the legs, particularly at nighttime. It is important to differentiate primary and secondary RLS from other conditions, which can mimic the symptoms of RLS, in particular neuropathy and cramps. Despite considerable advances, the understanding of RLS pathophysiology remains incomplete. Many hypotheses focus on central nervous system structures, although there is increasing evidence that peripheral structures may also be important. There is insufficient evidence at the moment to recommend changes in lifestyle, nutritional supplements and any specific nonpharmacologic treatments. The first-line drugs continue to be dopaminergic medications, including pramipexole, ropinirole, rotigotine transdermal patch and levodopa. However, the phenomenon of RLS augmentation, a paradoxical worsening of symptoms by dopaminergic treatment remains as major problem in treatment of RLS, and prevention of augmentation is one of the main goals in the management of RLS. RLS requires treatment only if it has a significant impact on the patient’s nighttime sleep or daily activities. Doses of dopamine agonists should be kept to the minimum required for acceptable symptom reduction. Augmentation may require treatment withdrawal, with prescription of alternate medication. Alternative or additional pharmacologic treatment with a lower level of overall quality of evidence includes opioids (codeine, tramadol, and oxycodone) and anticonvulsants (gabapentin, gabapentin enacarbil, and pregabalin). The choice of the medication should be based on the severity of RLS and the effectiveness of medication for the short-term or long-term treatment of RLS. Iron deficiency must be identified at diagnosis; treatment may improve RLS symptoms and potentially may lower risk of augmentation. There is no clear evidence for treatment of secondary RLS, but agents used in primary RLS should be tried. Comparative long-term trials are required to assess differences in efficacy and augmentation rates between medications used for treatment of RLS.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance•• Of major importance
Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19.
Bjorvatn B, Leissner L, Ulfberg J, et al. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. 2005;6:307–12.
Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Arch Intern Med. 2004;164:196–202.
Zucconi M, Ferini-Strambi L. Epidemiology and clinical findings of restless legs syndrome. Sleep Med. 2004;5:293–9.
Trenkwalder C, Paulus W. Restless legs syndrome: pathophysiology, clinical presentation and management. Nat Rev Neurol. 2010;6:337–46.
Winkelmann J, Muller-Myhsok B, Wittchen HU, et al. Complex segregation analysis of restless legs syndrome provides evidence for an autosomal dominant mode of inheritance in early age at onset families. Ann Neurol. 2002;52:297–302.
Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med. 2000;1:11–9.
Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology. 2009;72:955–60.
Hening WA, Walters AS, Wagner M, et al. Circadian rhythm of motor restlessness and sensory symptoms in the idiopathic restless legs syndrome. Sleep. 1999;22:901–12.
Trenkwalder C, Hening WA, Walters AS, et al. Circadian rhythm of periodic limb movements and sensory symptoms of restless legs syndrome. Mov Disord. 1999;14:102–10.
Michaud M, Dumont M, Selmaoui B, et al. Circadian rhythm of restless legs syndrome: relationship with biological markers. Ann Neurol. 2004;55:372–80.
Garcia-Borreguero D, Allen RP, Benes H, et al. Augmentation as a treatment complication of restless legs syndrome: concept and management. Mov Disord. 2007;22 Suppl 18:S476–84.
Allen R. Dopamine and iron in the pathophysiology of restless legs syndrome (RLS). Sleep Med. 2004;5:385–91.
Connor JR, Boyer PJ, Menzies SL, et al. Neuropathological examination suggests impaired brain iron acquisition in restless legs syndrome. Neurology. 2003;61:304–9.
Winkelmann J, Schormair B, Lichtner P, et al. Genome-wide association study of restless legs syndrome identifies common variants in three genomic regions. Nat Genet. 2007;39:1000–6.
Trenkwalder C, Paulus W. Why do restless legs occur at rest? Pathophysiology of neuronal structures in RLS. Neurophysiology of RLS (part 2). Clin Neurophysiol. 2004;115:1975–88.
Paulus W, Trenkwalder C. Less is more: pathophysiology of dopaminergic-therapy-related augmentation in restless legs syndrome. Lancet Neurol. 2006;5:878–86.
Gemignani F, Brindani F, Vitetta F, Marbini A, Calzetti S. Restless legs syndrome in diabetic neuropathy: a frequent manifestation of small fiber neuropathy. J Peripher Nerv Syst. 2007;12:50–3.
Polydefkis M, Allen RP, Hauer P, et al. Subclinical sensory neuropathy in late-onset restless legs syndrome. Neurology. 2000;55:1115–21.
Rios Romenets S, Dauvilliers Y, Cochen De Cock V, et al. Restless legs syndrome outside the blood-brain barrier - exacerbation by domperidone in Parkinson's disease. Parkinsonism Relat Disord. 2013;19:92–4.
O'Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200–3.
Aurora RN, Kristo DA, Bista SR, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults-an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses: an American Academy of Sleep Medicine Clinical Practice Guideline. Sleep. 2012;35:1039–62. This article provides an update of previous review of American Academy of Sleep Medicine in the treatments of RLS using a systematic literature review and meta-analyses.
Garcia-Borreguero D, Ferini-Strambi L, Kohnen R, et al. European guidelines on management of restless legs syndrome: report of a joint task force by the European Federation of Neurological Societies, the European Neurological Society and the European Sleep Research Society. Eur J Neurol. 2012;19:1385–96. This article is the European guidelines, which provides recently revised evidence-based recommendations for the treatment for RLS.
Cornelius JR, Tippmann-Peikert M, Slocumb NL, Frerichs CF, Silber MH. Impulse control disorders with the use of dopaminergic agents in restless legs syndrome: a case-control study. Sleep. 2010;33:81–7.
Ondo WG, Lai D. Predictors of impulsivity and reward seeking behavior with dopamine agonists. Parkinsonism Relat Disord. 2008;14:28–32.
Driver-Dunckley ED, Noble BN, Hentz JG, et al. Gambling and increased sexual desire with dopaminergic medications in restless legs syndrome. Clin Neuropharmacol. 2007;30:249–55.
O'Sullivan SS, Evans AH, Lees AJ. Dopamine dysregulation syndrome: an overview of its epidemiology, mechanisms and management. CNS Drugs. 2009;23:157–70.
Tippmann-Peikert M, Park JG, Boeve BF, Shepard JW, Silber MH. Pathologic gambling in patients with restless legs syndrome treated with dopaminergic agonists. Neurology. 2007;68:301–3.
Quickfall J, Suchowersky O. Pathological gambling associated with dopamine agonist use in restless legs syndrome. Parkinsonism Relat Disord. 2007;13:535–6.
Williams AM, Garcia-Borreguero D. Management of restless legs syndrome augmentation. Curr Treat Options Neurol. 2009;11:327–32.
Hogl B, Garcia-Borreguero D, Kohnen R, et al. Progressive development of augmentation during long-term treatment with levodopa in restless legs syndrome: results of a prospective multi-center study. J Neurol. 2010;257:230–7.
Collado-Seidel V, Kazenwadel J, Wetter TC, et al. A controlled study of additional sr-L-dopa in L-dopa-responsive restless legs syndrome with late-night symptoms. Neurology. 1999;52:285–90.
Hogl B, Garcia-Borreguero D, Trenkwalder C, et al. Efficacy and augmentation during 6 months of double-blind pramipexole for restless legs syndrome. Sleep Med. 2011;12:351–60.
Walters AS, Ondo WG, Dreykluft T, et al. Ropinirole is effective in the treatment of restless legs syndrome. TREAT RLS 2: a 12-week, double-blind, randomized, parallel-group, placebo-controlled study. Mov Disord. 2004;19:1414–23.
Trenkwalder C, Garcia-Borreguero D, Montagna P, et al. Ropinirole in the treatment of restless legs syndrome: results from the TREAT RLS 1 study, a 12 week, randomized, placebo controlled study in 10 European countries. J Neurol Neurosurg Psychiatry. 2004;75:92–7.
Garcia-Borreguero D, Grunstein R, Sridhar G, et al. A 52-week open-label study of the long-term safety of ropinirole in patients with restless legs syndrome. Sleep Med. 2007;8:742–52.
Oertel W, Trenkwalder C, Benes H, et al. Long-term safety and efficacy of rotigotine transdermal patch for moderate-to-severe idiopathic restless legs syndrome: a 5-year open-label extension study. Lancet Neurol. 2011;10:710–20. This is standard large and recent clinical trial, which test new option for treatment of moderate to severe primary RLS.
Davis BJ, Rajput A, Rajput ML, Aul EA, Eichhorn GR. A randomized, double-blind placebo-controlled trial of iron in restless legs syndrome. Eur Neurol. 2000;43:70–5.
Trenkwalder C, Hogl B, Benes H, Kohnen R. Augmentation in restless legs syndrome is associated with low ferritin. Sleep Med. 2008;9:572–4.
Allen RP, Adler CH, Du W, et al. Clinical efficacy and safety of IV ferric carboxymaltose (FCM) treatment of RLS: a multi-centered, placebo-controlled preliminary clinical trial. Sleep Med. 2011;12:906–13. This is a big, standard large and recent RCT's, which provides new option of treatment of RLS with intravenous iron salt.
Earley CJ, Heckler D, Allen RP. The treatment of restless legs syndrome with intravenous iron dextran. Sleep Med. 2004;5:231–5.
Ondo WG. Intravenous iron dextran for severe refractory restless legs syndrome. Sleep Med. 2010;11:494–6.
Auerbach M, Al TK. Low-molecular weight iron dextran and iron sucrose have similar comparative safety profiles in chronic kidney disease. Kidney Int. 2008;73:528–30.
Horiguchi J, Yamashita H, Mizuno S, et al. Nocturnal eating/drinking syndrome and neuroleptic-induced restless legs syndrome. Int Clin Psychopharmacol. 1999;14:33–6.
Pinninti NR, Mago R, Townsend J, Doghramji K. Periodic restless legs syndrome associated with quetiapine use: a case report. J Clin Psychopharmacol. 2005;25:617–8.
Kang SG, Park YM, Choi JE, et al. Association study between antipsychotic-induced restless legs syndrome and polymorphisms of monoamine oxidase genes in schizophrenia. Hum Psychopharmacol. 2010;25:397–403.
Kang SG, Lee HJ, Jung SW, et al. Characteristics and clinical correlates of restless legs syndrome in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1078–83.
Aurora RN, Morgenthaler TI. On the goodness of recommendations: the changing face of practice parameters. Sleep. 2010;10:1273–6.
Acknowledgments
This study was funded by the Canadian Institutes of Health Research and the Fonds de la Recherche en Santé du Québec.
Conflict of Interest
Silvia Rios Romenets declares that she has no conflict of interest.
Ronald B. Postuma received compensation for travel and speaker fees from Novartis Canada and Teva Neurosciences and is funded by grants from the Fonds de la Recherche en Santé du Québec, the Parkinson Society of Canada, the Webster Foundation, and by the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rios Romenets, S., Postuma, R.B. Treatment of Restless Legs Syndrome. Curr Treat Options Neurol 15, 396–409 (2013). https://doi.org/10.1007/s11940-013-0241-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-013-0241-x