Abstract
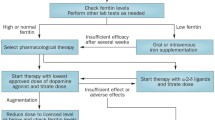
Restless legs syndrome (RLS) has a high prevalence in the elderly and can impact sleep quality and sleep quantity, reduce quality of life (QoL), and increase the risk of falls during episodes of night-time ambulation. In patients unable to verbalize their sensory symptoms, certain behavioral cues may help with the diagnosis. A state of brain iron deficiency could play a central role in the pathophysiology of RLS and be upstream to a series of dysfunctions that are not limited to the dopaminergic system. Management should initially emphasize lifestyle modifications and reduction of all possible iatrogenic contributors while maintaining a state of normal–high peripheral iron stores. Oral iron, in patients with ferritin levels < 75 μg/dL, appears to be effective, although iron infusions should be considered when more immediate benefit or oral iron have not been effective. When other attempts fail and patients continue to experience chronic RLS symptoms substantially interfering with QoL, pharmacological agents may present a favorable benefit versus risk profile. Such agents may include α-2-δ drugs or dopaminergic agents, after careful consideration of the risk of RLS augmentation with the latter class. In patients with established RLS augmentation from the use of dopaminergic drugs, the addition of α-2-δ agents or low-dose opioids, with subsequent slow tapering of dopaminergic agents, is recommended. With any of these agents, caution should be made with regard to the risk of drug–drug interactions and altered pharmacokinetics in this fragile population. Although showing excellent long-term safety data in non-elderly adults with RLS, studies are needed to ascertain that such treatments are effective and well tolerated in older adults.

Similar content being viewed by others
References
Garcia-Borreguero D, Egatz R, Winkelmann J, Berger K. Epidemiology of restless legs syndrome: the current status. Sleep Med Rev. 2006;10(3):153–67.
Ohayon MM, O’Hara R, Vitiello MV. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev. 2012;16(4):283–95.
Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165(11):1286–92.
Kuzniar TJ, Silber MH. Multiple skeletal injuries resulting from uncontrolled restless legs syndrome. J Clin Sleep Med. 2007;3(1):60–1.
Walters AS, Hickey K, Maltzman J, Verrico T, Joseph D, Hening W, et al. A questionnaire study of 138 patients with restless legs syndrome: the “night-walkers” survey. Neurology. 1996;46(1):92–5.
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria—history, rationale, description, and significance. Sleep Med. 2014;15(8):860–73.
Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997;12(1):61–5.
Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4(2):121–32.
Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4(2):101–19.
Bliwise DL. Periodic leg movements in sleep and restless legs syndrome: considerations in geriatrics. Sleep Med Clin. 2006;1(2):263–71.
Richards K, Shue VM, Beck CK, Lambert CW, Bliwise DL. Restless legs syndrome risk factors, behaviors, and diagnoses in persons with early to moderate dementia and sleep disturbance. Behav Sleep Med. 2010;8(1):48–61.
Yang Q, Li L, Chen Q, Foldvary-Schaefer N, Ondo WG, Wang QK. Association studies of variants in MEIS1, BTBD9, and MAP2K5/SKOR1 with restless legs syndrome in a US population. Sleep Med. 2011;12(8):800–4.
Schormair B, Zhao C, Bell S, Tilch E, Salminen AV, Pütz B, et al. Identification of novel risk loci for restless legs syndrome in genome-wide association studies in individuals of European ancestry: a meta-analysis. Lancet Neurol. 2017;16(11):898–907.
Earley CJ, Connor JR, Beard JL, Malecki EA, Epstein DK, Allen RP. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000;54(8):1698–700.
Li X, Allen RP, Earley CJ, Liu H, Cruz TE, Edden RAE, et al. Brain iron deficiency in idiopathic restless legs syndrome measured by quantitative magnetic susceptibility at 7 tesla. Sleep Med. 2016;22:75–82.
Dinkins ML, Lallemand P, Clemens S. Long-term treatment with dopamine D3 receptor agonists induces a behavioral switch that can be rescued by blocking the dopamine D1 receptor. Sleep Med. 2017;40:47–52.
Ferré S, Quiroz C, Guitart X, Rea W, Seyedian A, Moreno E, et al. Pivotal role of adenosine neurotransmission in Restless Legs Syndrome. Front Neurosci. 2018;11:722.
Rivera-Oliver M, Moreno E, Álvarez-Bagnarol Y, Ayala-Santiago C, Cruz-Reyes N, Molina-Castro GC, et al. Adenosine A1-dopamine D1 receptor heteromers control the excitability of the spinal motoneuron. Mol Neurobiol. 2019;56(2):797–811.
Walters AS, Ondo WG, Zhu W, Le W. Does the endogenous opiate system play a role in the Restless Legs Syndrome? A pilot post-mortem study. J Neurol Sci. 2009;279(1–2):62–5.
Silber MH, Becker PM, Buchfuhrer MJ, Earley CJ, Ondo WG, Walters AS, et al. The appropriate use of opioids in the treatment of refractory restless legs syndrome. Mayo Clin Proc. 2018;93(1):59–67.
Xu XM, Liu Y, Jia SY, Dong MX, Cao D, Wei YD. Complementary and alternative therapies for restless legs syndrome: an evidence-based systematic review. Sleep Med Rev. 2018;38:158–67.
Winkelman JW, Armstrong MJ, Allen RP, Chaudhuri KR, Ondo W, Trenkwalder C, et al. Practice guideline summary: treatment of restless legs syndrome in adults. Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2016;87(24):2585–93.
Lettieri CJ, Eliasson AH. Pneumatic compression devices are an effective therapy for restless legs syndrome: a prospective, randomized, double-blinded, sham-controlled trial. Chest. 2009;135(1):74–80.
Allen RP, Picchietti DL, Auerbach M, Cho YW, Connor JR, Earley CJ, et al. Evidence-based and consensus clinical practice guidelines for the iron treatment of restless legs syndrome/Willis-Ekbom disease in adults and children: an IRLSSG task force report. Sleep Med. 2018;41:27–44.
Silver N, Allen RP, Senerth J, Earley CJ. A 10-year, longitudinal assessment of dopamine agonists and methadone in the treatment of restless legs syndrome. Sleep Med. 2011;12(5):440–4.
Garcia-Borreguero D, Silber MH, Winkelman JW, Högl B, Bainbridge J, Buchfuhrer M, et al. Guidelines for the first-line treatment of restless legs syndrome/Willis-Ekbom disease, prevention and treatment of dopaminergic augmentation: a combined task force of the IRLSSG, EURLSSG, and the RLS-foundation. Sleep Med. 2016;21:1–11.
Allen R, Chen C, Garcia-Borreguero D, Polo O, DuBrava S, Miceli J, et al. Comparison of pregabalin with pramipexole for restless legs syndrome. N Engl J Med. 2014;370(7):621–31.
Garcia-Borreguero D, Patrick J, DuBrava S, Becker P, Lankford A, Chen C, et al. Pregabalin versus pramipexole: effects on sleep disturbance in restless legs syndrome. Sleep. 2014;37(4):635–43.
Iftikhar IH, Alghothani L, Trotti LM. Gabapentin enacarbil, pregabalin and rotigotine are equally effective in restless legs syndrome: a comparative meta-analysis. Eur J Neurol. 2017;24(12):1446–56.
Gibbons RD, Hur K, Brown CH, Mann JJ. Gabapentin and suicide attempts. Pharmacoepidemiol Drug Saf. 2010;19(12):1241–7.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 updated AGS beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
Walters AS, Wagner ML, Hening WA, Grasing K, Mills R, Chokroverty S, et al. Successful treatment of the idiopathic restless legs syndrome in a randomized double-blind trial of oxycodone versus placebo. Sleep. 1993;16(4):327–32.
Trenkwalder C, Beneš H, Grote L, García-Borreguero D, Högl B, Hopp M, et al. Prolonged release oxycodone-naloxone for treatment of severe restless legs syndrome after failure of previous treatment: a double-blind, randomised, placebo-controlled trial with an open-label extension. Lancet Neurol. 2013;12(12):1141–50.
Walters AS, Winkelmann J, Trenkwalder C, Fry JM, Kataria V, Wagner M, et al. Long-term follow-up on restless legs syndrome patients treated with opioids. Mov Disord. 2001;16(6):1105–9.
Aurora RN, Rosenberg RS, Kristo DA, Bista SR, Casey KR, Rowley JA, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults—an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses. Sleep. 2012;35(8):1039–62.
Howell MJ, Schenck CH. Restless nocturnal eating: a common feature of Willis-Ekbom Syndrome (RLS). J Clin Sleep Med. 2012;8(4):413–9.
Provini F, Antelmi E, Vignatelli L, Zaniboni A, Naldi G, Calandra-Buonaura G, et al. Association of restless legs syndrome with nocturnal eating: a case-control study. Mov Disord. 2009;24(6):871–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
John W. Winkelman reports research support from Merck, National Institute of Mental Health, the Restless Legs Syndrome Foundation, and American Regent, and was a consultant for, or received honoraria from, Merck, Advance Medical, and UpToDate. Emmanuel H. During reports no conflicts of interest in relation to this article.
Rights and permissions
About this article
Cite this article
During, E.H., Winkelman, J.W. Drug Treatment of Restless Legs Syndrome in Older Adults. Drugs Aging 36, 939–946 (2019). https://doi.org/10.1007/s40266-019-00698-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00698-1