Abstract
Purpose of Review
Poor physical fitness is a common finding in patients with cirrhosis and is associated with increased morbidity and mortality. This review aims to summarize the existing literature on the impact of exercise interventions in cirrhosis and guiding the healthcare providers in determining the optimal exercise program in this population.
Recent Findings
Exercise interventions including aerobic and resistance training have benefits on markers of sarcopenia, cardiorespiratory fitness and quality of life, and are safe, even in the decompensated stage.
Summary
Poor physical fitness in cirrhosis is multifactorial. The goal of exercise interventions in cirrhosis is to improve outcomes by increasing muscle mass and function, preventing further skeletal muscle breakdown, and improving cardiovascular fitness. Exercise programs combining aerobic and resistance training at a moderate intensity and for at least 8 to 12 weeks, in both site-based and home-based settings, have benefits on sarcopenia and aerobic capacity, as well as on quality of life. Efforts need to be made to improve the adherence to exercise interventions, especially home-based programs, in order to maximize their benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with cirrhosis have an overall lower level of physical activity than patients with other chronic diseases. Multiple factors contribute to this poor physical fitness, which particularly affects patients in the decompensated stage: energy and protein malnutrition with associated sarcopenia (low muscle mass, strength and function), physical limitations from ascites and lower limb edema, need for repeated hospitalizations for decompensation events, hepatic encephalopathy and depression, among others. This leads to frailty, a state of decreased physiological reserve associated with a low quality of life, poor clinical outcome and mortality, including on the liver transplantation (LT) waiting list, irrespective of the Model for End-stage Liver Disease (MELD) score [1]. Exercise has well-recognized beneficial effects on health. The goal of exercise interventions in cirrhosis is to improve muscle mass and function and to prevent further skeletal muscle breakdown, as well as to improve cardiovascular fitness, helping patients in maintaining their autonomy in the daily life. Additionally, exercise may have benefits on clinical outcomes, although this has until now never been specifically addressed. Despite these anticipated benefits, current guidelines on the management of chronic liver diseases do not offer specific recommendations on exercise, contrary to other chronic diseases. In recent years, multiple groups have looked at the feasibility and impact of exercise interventions in cirrhosis, testing various types of training (resistance and/or aerobic), frequency, duration, intensity, and setting (supervised vs. home-based). It is clear that patients with cirrhosis should exercise, but the optimal exercise intervention remains unknown, and how to maximize the adherence to such an intervention is a challenging question. This review provides an update on the existing literature evaluating exercise interventions in cirrhosis. Table 1 summarizes prospective studies published in this field.
Endpoints in exercise interventions in cirrhosis
Endpoints measuring changes in physical fitness can be classified into two categories: those focusing on muscle mass, strength and function and those evaluating cardiorespiratory fitness, with frailty indices reflecting both of these components. A more detailed discussion of the validated tools for the assessment of sarcopenia, frailty and cardiorespiratory fitness in cirrhosis and their prognostic value is beyond the scope of this review and can be found elsewhere [20]. Most studies evaluating exercise interventions in cirrhosis included a combination of these endpoints, which vary in their complexity, need for trained personnel, costs and inter-observer variability (Table 1). Some studies also reported the hepatic venous pressure gradient (HVPG) and quality of life through validated questionnaires, and one study reported liver and spleen stiffness [11].
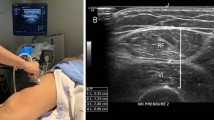
The current gold standard for the assessment of muscle mass, the skeletal muscle index (SMI, in cm2/m2, calculated by dividing the skeletal muscle area on computed tomography (CT) at a specific vertebra level, by the height of the patient), was reported in only one of the presented study (together with the psoas muscle index) [13]. The effect of exercise on muscle composition (myosteatosis), which can be assessed by CT, has never been specifically addressed. One study reported the cross-sectional area of the quadriceps (from magnetic resonance imaging) [2]. Thigh muscle thickness measured by ultrasound was also reported in a few studies. Other reported validated methods were the fat-free mass on whole-body dual-energy X-ray absorptiometry (DXA) and bioelectrical impedance analysis (BIA) with phase angle (PhA), but were not the methods of choice in studies including patients with decompensated cirrhosis since they are affected by fluid retention. Anthropometric measurements such as the mid-arm muscle circumference (MAMC), mid-arm muscular area (MAMA), and triceps skinfold (TSF) were reported in some studies. The handgrip strength and the quadriceps strength were the most frequent tools used to measure muscle strength and function.
The main endpoint in studies using cardiopulmonary exercise testing (CPET) was the peak VO2, which is the gold standard for the assessment of aerobic capacity and represents the maximum oxygen uptake during peak aerobic exercise. Several studies reported the 6-min walk test (6MWT), a simple test reflecting the aerobic endurance.
Frailty was an endpoint in two studies and was measured through the Liver Frailty Index (LFI, https://liverfrailtyindex.ucsf.edu/) [12], or the timed Up&Go [6].
Type, intensity and schedule of exercises
Each type of exercise has an effect on the two major components of physical fitness: aerobic exercises improve the aerobic capacity and cardiorespiratory fitness, while resistance exercises improve muscle mass, strength and function. In site-based studies, aerobic exercises were performed periodically with the use of a treadmill or cycle ergometer. One home-based study also used a cycle ergometer, which was delivered and set up at the patient’s home [15]. Other home-based programs aimed for a more continuous aerobic exercise using a wearable activity tracker with daily target steps and weekly increments, usually by 500 steps per day. Resistance training exercises were performed in most studies with the use of elastic bands or weights, but also without equipment and only against gravity. Some studies included stretching, coordination and balance exercises as well [6, 7].
Most studies targeted a moderate activity, i.e. 60–80% of HRmax or of baseline peak VO2, or 12–14/20 points (or 5–6/10) on the Borg Rating of Perceived Exertion Scale. Interestingly, Chen et al. used cadence, or per-minute step count using wearable activity tracker, to monitor and define the intensity of exercise, with moderate and vigorous intensity defined as 80–130 and > 130 steps/minute, respectively [21]. Most studies also recommended patients to stay active during the daily routine to increase the non-exercise activity thermogenesis.
All studies agree that, to be able to see beneficial effects from exercise, the minimal program duration should be 8–12 weeks, with longer programs having a more durable effect. The frequency of exercise sessions was variable, from daily to once weekly, with an average of thrice weekly.
As most studies published in the last 5 years evaluating exercise interventions in cirrhosis have included both categories of exercise (Table 1), it is challenging to isolate the effects of each type of exercise on each clinical endpoint. Moreover, pure aerobic or resistance training does not exist, and while some measured endpoints reflect more aerobic capacity (CPET, 6MWT) or muscle mass, strength and function (SMI, fat-free mass through BIA or DXA, handgrip strength), both types of exercise probably have mixed effects on overall physical fitness. For instance, a recent study in LT candidates showed an improvement in handgrip strength after an exclusively aerobic training program using a static bike, showing that handgrip strength does not only depend on upper extremity muscle strength but also on systemic factors [3].
Overall, aerobic and resistance training seem to have beneficial effects in cirrhosis (Table 1). Resistance training improved endpoints reflecting muscle mass (through cross-sectional or ultrasound evaluation, or estimation through BIA or DXA) and strength/function (handgrip and quadriceps strength) in most studies, in comparison to baseline and in some cases compared with the control group. Chen et al. did not observe an improvement in the SMI in the exercise group compared to baseline and to the control group; however, the sample size was small (N = 20) and not calculated to detect statistically significant changes. Moreover, the main intervention was walking and the adherence to the resistance exercises might have been insufficient to improve the SMI (the psoas muscle index did improve in the exercise group). Sirisunhirun et al. observed a non-significant improvement in the thigh muscle mass in the exercise group, while it decreased in the control group [11].
Aerobic training was associated in most studies with an improvement in CPET parameters such as the peak VO2 and 6MWT compared to baseline and in some studies compared with the control group. A recent RCT did not show a significant improvement in the 6MWT after a 12-week home-based training program consisting of both resistance and aerobic exercises [11]. This absence of significant change might be explained by the fact that patients were already quite fit at baseline (all with compensated cirrhosis, CTP score A) and that the 6MWT may not be sensitive enough to detect aerobic capacity improvements in this context. In this study, liver and spleen stiffness were chosen as surrogates of portal hypertension and no significant changes were observed between groups. Although exercise has been associated with improvement in HVPG [5, 7], liver and spleen stiffness are not able to accurately reflect small changes in portal pressure. Some studies showed a worsening of the peak VO2 or the 6MWT in the control group, showing how an exercise intervention may prevent the inevitable deterioration observed with disease progression.
Exercise may improve frailty. Roman et al. showed an improvement in the timed Up&Go test compared to baseline [6]. The intervention proposed by Lai et al. was not feasible due to lack of adherence, which prevents conclusions on its effect on frailty [12]. This underlines how one must be careful when interpreting data from studies on exercise interventions in cirrhosis. Most studies were small, had poor adherence, and some were pilot trials where the sample size was determined empirically and not calculated to detect statistically significant differences in the main endpoints. Moreover, when comparing each patient’s performance to baseline, the absence of an improvement of an endpoint may in fact indicate that the intervention prevented a deterioration, and concluding to an absence of benefit of the intervention would be misleading. Larger, properly sized studies are an unmet need in hepatology.
Setting of the exercise training program and impact on adherence
Both site-based exercise interventions and home-based programs have been evaluated and have demonstrated benefits on sarcopenia and aerobic capacity (Table 1). The earlier studies involved mostly well-structured on-site training in a training facility usually involving gym machines with direct supervision from an exercise specialist. The advantage of this setting is the degree of supervision that can be offered, which might allow reaching higher degrees of intensity of the training, as well as access to specialized equipment. However, it is not clear if this would be maintained with longer duration programs or in the “real-life” setting. Additionally, site-based programs require significant financial and personnel resources, and the need for patients to travel to the hospital or exercise facility, which can be unpractical, costly, and limit adherence on the long term.
In recent years, several studies have evaluated home-based programs to overcome the barriers associated with site-based training programs. These programs usually involved an initial evaluation with an exercise specialist to explain the program in details and to tailor it to individual patients. The resistance training exercises were performed at home with the support of exercise worksheets or videos (online or DVD). The aerobic component was usually performed using a wearable activity tracker and daily target steps.
One of the main difference between site-based exercise interventions and home-based programs, beyond the setting where the exercises are performed, was the supervision and the frequency and type of follow-up, which has a major influence on adherence. The definition of adherence varied among studies, varying from full compliance to the exercise intervention vs. any time participation. Although the adherence to the exercise intervention was good to excellent in all studies, it was overall superior in site-based programs in comparison to home-based programs. The presence of an exercise-specific infrastructure with direct supervision and continuous, personalized counselling are some of the factors explaining this finding.
In both site-based and home-based studies, most programs included educational sessions (Fig. 1). Some also included a health coach or motivational interviews by the research personnel, which we believe are key interventions in order to elicit behavioral change in patients and identify potential barriers to exercise. The involvement of a psychologist may also be considered. Health engagement questions, together with financial incentives, had a positive impact on physical activity after kidney and liver transplantation in a recent pilot study. Approaches using behavioral economics may provide new tools to improve adherence to lifestyle interventions [22].
To maintain adherence, most programs involved regular phone calls (usually weekly to biweekly, but as frequent as daily if needed). However, the efficacy of an intensive remote follow-up in home-based studies has not been so far convincing. For instance, in the STRIVE trial, the largest trial so far published evaluating a home-based program, despite the involvement of a health coach and regular phone calls, adherence was extremely poor (13%) [12]. In the study by Williams et al., adherence decreased dramatically as soon as weekly phone calls were stopped (after week 6) [14]. In a study combining a 12-month home-based exercise program with BCAA supplementation (not shown in Table 1), scheduling monthly group sessions might have allowed the persistence of benefits observed at the end of the intervention [16].
A barrier to adherence to exercise programs is their complexity. In our experience, the sicker the patients are, the simpler the intervention should be. Use of technology such as wearable activity trackers is promising, but might represent an additional challenge in patients with encephalopathy or very severe liver disease and the help of a caregiver may be necessary in this population to assist patients in using them.
Severity of liver disease and safety
Most studies evaluating exercise interventions in cirrhosis included patients in the compensated stage. One of the reasons is the concern for safety in patients with decompensated cirrhosis and the potential risk of an exercise-induced rise in the portal pressure. Indeed, an early study published in 1996 observed a rise in portal pressure in eight patients with cirrhosis and portal hypertension (not on beta-blockers) performing cycle ergometry (at 50% of peak workload), quickly returning to baseline after stopping exercise, concluding to a possible increased risk of variceal bleeding during exercise [23]. Nevertheless, out of the two site-based [3, 4] and three home-based exercise program studies [12,13,14] focusing on patients with decompensated cirrhosis referred for or awaiting LT (in the study by Lai et al. inclusion criteria was MELD ≥ 12; 53% were Child–Pugh B/C), none reported episodes of variceal bleeding during exercise. We do recommend that patients receive appropriate beta-blockade before entering an exercise program and that those with severe portal hypertension avoid abdominal crunch since this acutely increases abdominal pressure.
Exercise training may in fact have long-term benefits on portal hypertension, as demonstrated by an open-label pilot RCT showing a reduction of 2.5 mm Hg in the portal pressure after a 14-week program of combined aerobic training and kinesiotherapy [7]. In this study, the authors observed an increase in the HVPG in the control group. A study in patients with compensated cirrhosis with overweight or obesity also showed a benefit of a 16-week exercise program and a hypocaloric diet on portal pressure. Although the weight loss was probably the major driving factor on the improvement of portal pressure in patients losing more than 5% weight, a higher amount of exercise was still associated with a more significant decrease in portal pressure in patients with minimal weight loss (< 5%), suggesting an independent benefit of exercise on portal hypertension [5]. The effects of exercise on portal pressure may be explained by a decrease in systemic inflammation and an improvement in endothelial function and intra-hepatic resistance. This may translate into benefits on clinical outcomes, since portal hypertension drives most cirrhosis-related complications, but none of the studies published so far have assessed this specifically.
Regarding other safety parameters, all studies reported that the exercise interventions were not associated with excess decompensation events or falls. In the case of home-based interventions, this may be however explained by the lower degree of intensity of the training. Individual tailoring of the exercise training by an exercise specialist and when possible, supervision by a caregiver, is key to ensure safety of the intervention, especially in the presence of ascites and hepatic encephalopathy.
Association of exercise with a nutritional intervention
Malnutrition is very frequent in cirrhosis, particularly in the decompensated stage, and nutritional interventions with specific calorie and protein intake targets have the potential of improving muscle mass and sarcopenia in cirrhosis. Most of the studies evaluating exercise interventions in cirrhosis included a nutritional intervention, which varied from standard nutritional advice to a more structured approach aiming for the recommended energy and protein targets in chronic liver diseases [1]. Importantly, the nutritional intervention was offered in the control group as well, to isolate the effect of the exercise from the effect of the nutritional intervention, although nutrition and exercise may have a synergistic effect on muscle mass. Several studies however did not comment on the adherence to these nutritional recommendations or reported the patients’ actual calorie and protein intake, which may influence the magnitude of the response to exercise.
Since the benefits of exercise training depend on adequate substrate reserves, some authors have suggested optimizing the nutritional status of patients prior to starting an exercise program. Moreover, a few studies included additional energy intake on exercise days (250–300 kcal or 30% kcal) to compensate for exercise-induced losses [7, 9, 11, 15]. This additional caloric intake should be taken into account in patients with overweight or obesity, in whom an overall reduction in caloric intake is recommended, for example by using body mass index (BMI)-specific daily caloric intake. One study, where a BMI ≥ 25 kg/m2 was an inclusion criteria, included a 500–1000 kcal calorie restriction [5]. More studies are needed to better define the appropriate energy and protein intake in patients with overweight or obesity undergoing an exercise training program, given the obesity pandemic and the high prevalence of sarcopenic obesity.
An adequate protein intake seems to allow maximum benefits from exercise training. Three RCT specifically included protein [11] or aminoacid [10, 13] supplementation in both groups in combination with exercise training, while Aamann et al. recommended the use of oral nutritional supplementation if protein intake was < 1.2 g/kg/d [2]. A pilot RCT showed that combining BCAA supplementation with a home-based exercise program improved 6MWT and psoas muscle index more than BCAA supplementation alone (both groups also had a daily protein target intake of 1.2–1.5 g/kg) [13].
Benefits of exercise interventions on quality of life
Beyond physical fitness, exercise intervention have been repetitively shown to have a positive effect on fatigue, depression, anxiety and on quality of life overall. Part of this effect is through the improvement in the physical fitness, which contributes in preserving the autonomy of patients and allow them to be able to perform activities of the daily living. Direct benefits of exercise on the brain may also be possible, through various mediators released in response to acute and/or chronic exercise (“exerkines”) [24].
Best strategies to implement exercise interventions in cirrhosis
Before starting an exercise program, patients should be screened for cardiopulmonary, orthopedic and other medical conditions that may require adjustments in the type and/or intensity of training. We also recommend systematically screening patients for malnutrition and frailty, and optimizing the nutritional status before or in parallel to the exercise intervention. Additional supplementation on exercise days should be considered. In patients with decompensated cirrhosis with ascites and hepatic encephalopathy, we strongly recommend to involve an exercise specialist to provide closer supervision and a safe, individualized intervention. A short motivational interview should be conducted in all patients prior to starting the intervention to elicit behavioral change and identify barriers to adherence. A baseline physical fitness assessment should be performed through validated tools and repeated during the exercise intervention to evaluate progress. The exercise intervention should include a combination of aerobic and resistance training, as well as balance and stretching exercises. Exercise should be prescribed with a specific frequency (at least four times per week and aiming for every day exercising), duration (starting with a few minutes in very deconditioned patients and increasing progressively to 40 min sessions, 150 min/week) and intensity (at least moderate). At least two sessions per week should include resistance training. Setting (site-based or home-based) should be defined depending on available resources and patient’s preference. In all cases, efforts should be made to maximize adherence during the intervention period, through regular contacts and potentially with the help of technologies such as wearable devices. Safety of the intervention should be reassessed regularly.
Conclusion
Exercise should be considered as a medical therapy for cirrhosis as it improves sarcopenia, aerobic capacity and quality of life, and potentially liver-related outcomes. We encourage healthcare providers to prescribe exercise including a combination of resistance and aerobic training with a specified frequency, duration and intensity [25]. Supervised exercise programs are effective but require many resources, while home-based exercise programs are feasible but adherence may be challenging. Some form of continuous support to guaranty long-term adherence would be ideal and further studies evaluating technologies, such as wearable devices and SMS- or applications including automated reinforcement strategies, are required. Moreover, trials assessing the effect of exercise interventions (combined with nutritional optimization) on strong clinical endpoints are needed.
References and Recommended Reading
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL clinical practice guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70(1):172–93.
Aamann L, Dam G, Borre M, Drljevic-Nielsen A, Overgaard K, Andersen H, et al. Resistance training increases muscle strength and muscle size in patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2020;18(5):1179-87 e6.
Morkane CM, Kearney O, Bruce DA, Melikian CN, Martin DS. An outpatient hospital-based exercise training program for patients with cirrhotic liver disease awaiting transplantation: a feasibility trial. Transplantation. 2020;104(1):97–103.
Wallen MP, Keating SE, Hall A, Hickman IJ, Pavey TG, Woodward AJ, et al. Exercise training is safe and feasible in patients awaiting liver transplantation: a pilot randomized controlled trial. Liver Transpl. 2019;25(10):1576–80.
Berzigotti A, Albillos A, Villanueva C, Genesca J, Ardevol A, Augustin S, et al. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: the SportDiet study. Hepatology. 2017;65(4):1293–305.
Roman E, Garcia-Galceran C, Torrades T, Herrera S, Marin A, Donate M, et al. Effects of an exercise programme on functional capacity, body composition and risk of falls in patients with cirrhosis: a randomized clinical trial. PLoS ONE. 2016;11(3): e0151652.
Macias-Rodriguez RU, Ilarraza-Lomeli H, Ruiz-Margain A, Ponce-de-Leon-Rosales S, Vargas-Vorackova F, Garcia-Flores O, et al. Changes in hepatic venous pressure gradient induced by physical exercise in cirrhosis: results of a pilot randomized open clinical trial. Clin Transl Gastroenterol. 2016;7(7): e180.
Debette-Gratien M, Tabouret T, Antonini MT, Dalmay F, Carrier P, Legros R, et al. Personalized adapted physical activity before liver transplantation: acceptability and results. Transplantation. 2015;99(1):145–50.
Zenith L, Meena N, Ramadi A, Yavari M, Harvey A, Carbonneau M, et al. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin Gastroenterol Hepatol. 2014;12(11):1920-6 e2.
Roman E, Torrades MT, Nadal MJ, Cardenas G, Nieto JC, Vidal S, et al. Randomized pilot study: effects of an exercise programme and leucine supplementation in patients with cirrhosis. Dig Dis Sci. 2014;59(8):1966–75.
Sirisunhirun P, Bandidniyamanon W, Jrerattakon Y, Muangsomboon K, Pramyothin P, Nimanong S, et al. Effect of a 12-week home-based exercise training program on aerobic capacity, muscle mass, liver and spleen stiffness, and quality of life in cirrhotic patients: a randomized controlled clinical trial. BMC Gastroenterol. 2022;22(1):66.
Lai JC, Dodge JL, Kappus MR, Wong R, Mohamad Y, Segev DL, et al. A multicenter pilot randomized clinical trial of a home-based exercise program for patients with cirrhosis: the strength training intervention (STRIVE). Am J Gastroenterol. 2021;116(4):717–22.
Chen HW, Ferrando A, White MG, Dennis RA, Xie J, Pauly M, et al. Home-based physical activity and diet intervention to improve physical function in advanced liver disease: a randomized pilot trial. Dig Dis Sci. 2020;65(11):3350–9.
Williams FR, Vallance A, Faulkner T, Towey J, Durman S, Kyte D, et al. Home-based exercise in patients awaiting liver transplantation: a feasibility study. Liver Transpl. 2019;25(7):995–1006.
Kruger C, McNeely ML, Bailey RJ, Yavari M, Abraldes JG, Carbonneau M, et al. Home exercise training improves exercise capacity in cirrhosis patients: role of exercise adherence. Sci Rep. 2018;8(1):99.
Nishida Y, Ide Y, Okada M, Otsuka T, Eguchi Y, Ozaki I, et al. Effects of home-based exercise and branched-chain amino acid supplementation on aerobic capacity and glycemic control in patients with cirrhosis. Hepatol Res. 2017;47(3):E193–200.
Hiraoka A, Michitaka K, Kiguchi D, Izumoto H, Ueki H, Kaneto M, et al. Efficacy of branched-chain amino acid supplementation and walking exercise for preventing sarcopenia in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 2017;29(12):1416–23.
Limongi V, dos Santos DC, da Silva AM, Ataide EC, Mei MF, Udo EY, et al. Effects of a respiratory physiotherapeutic program in liver transplantation candidates. Transplant Proc. 2014;46(6):1775–7.
Limongi V, Dos Santos DC, de Oliveira da Silva AM, Boin Ide F, Stucchi RS. Exercise manual for liver disease patients. World J Transplant. 2016;6(2):429–36.
Lai JC, Tandon P, Bernal W, Tapper EB, Ekong U, Dasarathy S, et al. Malnutrition, frailty, and sarcopenia in patients with cirrhosis: 2021 practice guidance by the American Association for the study of liver diseases. Hepatology. 2021;74(3):1611–44.
Chen HW, Ferrando AA, Dunn MA, Kim WR, Duarte-Rojo A. Cadence from physical activity trackers for monitoring of home-based exercise intensity in advanced liver disease. Liver Transpl. 2020;26(5):718–21.
Serper M, Barankay I, Chadha S, Shults J, Jones LS, Olthoff KM, et al. A randomized, controlled, behavioral intervention to promote walking after abdominal organ transplantation: results from the LIFT study. Transpl Int. 2020;33(6):632–43.
Garcia-Pagan JC, Santos C, Barbera JA, Luca A, Roca J, Rodriguez-Roisin R, et al. Physical exercise increases portal pressure in patients with cirrhosis and portal hypertension. Gastroenterology. 1996;111(5):1300–6.
Chow LS, Gerszten RE, Taylor JM, Pedersen BK, van Praag H, Trappe S, et al. Exerkines in health, resilience and disease. Nat Rev Endocrinol. 2022;18(5):273–89.
Tandon P, Ismond KP, Riess K, Duarte-Rojo A, Al-Judaibi B, Dunn MA, et al. Exercise in cirrhosis: translating evidence and experience to practice. J Hepatol. 2018;69(5):1164–77.
Funding
Open access funding provided by University of Bern
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Élise Vuille-Lessard declares that she has no conflict of interest.
Annalisa Berzigotti declares that she has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Liver
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vuille-Lessard, É., Berzigotti, A. Exercise Interventions for Cirrhosis. Curr Treat Options Gastro 20, 336–350 (2022). https://doi.org/10.1007/s11938-022-00393-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-022-00393-y