Abstract
Purpose of review
The treatment of coronary artery disease (CAD) in cancer patients is an evolving landscape. Recent data emphasizes the importance of aggressive management of cardiovascular risk factors and diseases in improving cardiovascular health in this unique group of patients regardless of cancer type or stage.
Recent findings
Novel cancer therapeutics such as immune therapies and proteasome inhibitors have been associated with CAD. Recent stent technologies may safely allow for shorter duration (< 6 months) of dual antiplatelet therapy post-percutaneous coronary interventions. Intracoronary imaging may be useful in the decision making process in terms of stent positioning and healing.
Summary
Large registry studies have partially filled a gap left by the lack of randomized controlled trials in the treatment of CAD in cancer patients. Cardio-oncology is gaining traction as a major sub-specialty in the cardiology field given the release of the first European Society of Cardiology — Cardio-oncology guidelines in 2022.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the era of COVID-19, cardiovascular diseases and cancer remain the leading causes of mortality in the USA [1, 2]. Due to a combination of shared risk factors, improved life span, and advancement in cancer therapies, there is a growing number of cancer patients with coexisting coronary artery disease (CAD) [3]. Cancer and its treatment can be associated in selected cases with additional vascular aging [4]. Despite increased prevalence, cancer patients are still routinely excluded from major cardiovascular randomized control trials. In recent years, several observational studies have helped us understand the pathophysiology and treatment principles needed to tailor management in such a high-risk population. The purpose of this review is to provide recent updates about the management of CAD in cancer patients, with a focus on discussing optimal strategies for coronary revascularization (Fig. 1).
Recent updates in coronary revascularization in cancer patients. ICI, immune checkpoint inhibitors; ACS, acute coronary syndrome; TTE, transthoracic echocardiogram; STEMI, ST segment elevation myocardial infarction; NSTEMI, non-ST segment elevation myocardial infarction; DAPT, dual antiplatelet therapy; FFR, fractional flow reserve; iFR, instantaneous wave-free ratio; IVUS, intravascular ultrasound; OCT, optical coherence tomography; SADIT, single-access, dual-injection technique; SHiP, Single access for Hi-risk PCI; TEG, thromboelastogram; PCI, percutaneous coronary intervention.
Epidemiology of coronary artery disease in the setting of cancer
Coronary atherosclerosis is a precursor for CAD development and subsequent acute coronary syndromes (ACS) [5, 6]. Low-density lipoprotein (LDL), the major culprit in the atherosclerotic cascade, when oxidized, decreases endothelial nitric oxide synthase expression, leading to increased inflammatory cell recruitment and adhesion to the injured endothelium. Endothelial lipid accumulation is followed by plaque formation and rupture, causing the cascade of platelet activation and aggregation, finally resulting in acute thrombus formation with subsequent loss in coronary perfusion and myocardial ischemia [7, 8]. Recent evidence suggests that upregulation of the lectin-like oxidized LDL (LOX-1) receptor seen in atherosclerosis leads to an increased formation of reactive oxygen species (ROS) which induce vascular endothelial growth factor (VEGF) production and thereby stimulating angiogenesis and perhaps tumor growth [9, 10]. Inflammatory markers such as C-reactive protein and interleukin 1β have been identified as mediators in both cancer and atherosclerosis, suggesting that the pathogenesis of cancer and CAD is connected at a cellular level [11,12,13].
Cancer and CAD share numerous traditional cardiovascular risk factors. The incidence of both diseases increases with aging, with the median time of diagnosis for common cancers such as breast, lung, and colorectal cancer being 63–71 years. Obesity and diabetes, by virtue of their chronic inflammatory state, lead to the early occurrence of both CAD/ACS and cancer [14,15,16,17,18]. Tobacco use, a well-known risk factor for ACS, promotes oxidation of LDL and formation of ROS which in turn cause atherosclerosis and carcinogenesis [19, 20]. Although hypertension has multiple overlapping risk factors with CAD and in turn with cancer, studies are ongoing to establish a direct link between them [21].
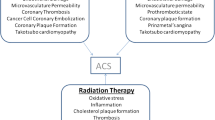
Certain chemotherapeutic agents have been well-established to cause accelerated coronary atherosclerosis and ACS. 5-Fluorouracil (5-FU) and its oral prodrug capecitabine are well-known to induce coronary vasospasm and precipitate ACS by activating protein kinase C and causing smooth muscle vasoconstriction [22,23,24,25,26]. Bevacizumab, a VEGF inhibitor, and tyrosine kinase inhibitors, such as sorafenib and sunitinib, are associated with an increased risk of arterial thrombosis [27,28,29,30]. Multiple cases of ACS secondary to rituximab, cisplatin, and taxols have been reported [31, 32]. Carfilzomib, a newly approved proteasome inhibitor used in the treatment of multiple myeloma, has been associated with an increased risk of heart failure, ischemic heart disease, and hypertension [33]. Hormonal therapies for breast cancer have been shown to increase the risk of cardiovascular events [34]. Interestingly, even patients who undergo hematopoietic stem cell transplants are at risk for cardiovascular toxicity, including CAD [35]. Immune checkpoint inhibitor (ICI) therapy-related cardiomyopathy and myocarditis have been well-established [36]. Recent data suggest a 3.3-fold increased risk for atherosclerotic cardiovascular events at 2 years after ICI therapy [37], although a direct causal mechanism is still under investigation. In a sub-analysis of that study, comparing atherosclerotic plaque volume in aortas using computed tomography (CT), an increase in plaque volume was noted with ICI therapy [37]. Interestingly, the concomitant use of statin and steroids had a moderating effect, showing the importance of optimizing cardiovascular risk factors during ICI therapy [37]. In a cohort study of nearly 700 patients, Laenens et al. found a 10% incidence of heart failure, ACS, and stroke in cancer patients within 1 year of initiating ICI therapy, almost double than those not on ICI therapy [38•].
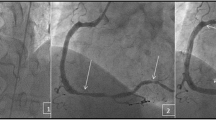
Ionizing radiation affects both cancerous and non-cancerous cells, especially the rapidly proliferating endothelial and bone marrow cells. The pathogenesis of radiation-induced vascular disease starts with oxidative stress, ROS formation, endothelial inflammation, and dysfunction with increased vascular permeability, finally leading to damage to the vasa vasorum [39]. Chest radiotherapy can accelerate the progression of pre-existing CAD. The typical pattern of radiation-induced coronary artery disease (RICAD) is ostial stenosis with severe left main disease, along with ostial right coronary artery and left anterior descending artery stenoses. RI-CAD with ostial and multivessel stenosis is usually seen after extensive mantle radiation in Hodgkin’s lymphoma, breast cancer, and esophageal cancer [40]. While majority get standard of care treatment, patients with refractory to treatment, radiation-induced heart disease have been reported [41].
Approach to coronary artery disease diagnosis and management
The clinical presentation of CAD and ACS can be atypical, confounded by cancer and its treatment, or due the advanced age of these patients and their co-morbidities, warranting a higher degree of suspicion. Accurate diagnosis involves a thorough history including assessment of risk factors, cancer type, and treatment, followed by a 12-lead electrocardiogram (ECG) and serial measurements of serum high-sensitivity cardiac troponin (Hs-cTn) [42••]. The 2022 European Society of Cardiology (ESC) Cardio-oncology guidelines suggest obtaining early echocardiography to improve the diagnostic precision and monitor for early systolic dysfunction in patients with atypical anginal symptoms [42••, 43]. Echocardiogram is useful in identifying regional wall motion abnormalities versus the near-global hypokinesis noted in Takotsubo syndrome, common in cancer patients [44,45,46,47]. Multimodality imaging with coronary computed tomography angiography and cardiac magnetic resonance imaging can also be used to help diagnose CAD and systolic dysfunction caused by ischemia, and differentiate it from other types of chemotherapy-related cardiotoxicities, such as myocarditis.
Cancer patients are subject to numerous imaging tests as part of their diagnosis, staging, and surveillance. Incidental findings of coronary artery calcium (CAC) in patients who have a non-cardiac chest computed tomography (CT) scan are rarely acted upon but can be useful in the prevention and treatment of CAD. In a retrospective study involving 164 lung cancer patients, who underwent non-contrast non-gated chest CT (NGCCT), CAC was noted in over 69% of patients without known pre-existing atherosclerotic CV disease (ASCVD), and an overwhelming majority was not started on guideline-directed medical therapy (GDMT) including aspirin and statin [48]. Coronary CT angiography (CTA) has a very high negative predictive value for the exclusion of obstructive CAD and can be used as an accurate first-line non-invasive imaging test in cancer patients who are at low to intermediate risk for CAD [49]. Cardiac CT may also have a role in the evaluation of CAD in ACS-like conditions such as 5-fluorouracil-induced vasospasm and ICI cardiotoxicity [50].
Risk stratification of CAD and ACS in cancer patients
ACS are associated with significantly higher mortality and morbidity rates in cancer patients than in their non-cancer counterparts [51]. Yousif et al., in their prospective study, reported a higher all-cause mortality rate at 12 months, 30.3% in cancer vs. 11.9% in non-cancer patients, p < 0.0001, along with a higher incidence of net adverse clinical events, 33.9% in cancer patients vs. 19.8% in non-cancer patients, p < 0.001 [52]. Mrtozek et al. showed that troponin-positive ACS (HR 2.365 [1.162–4.817], p = 0.018) was most predictive of mortality in cancer patients presenting with ACS. They also reported a 1-year all-cause mortality rate of 46% vs. 8% in non-cancer patients [53]. Patients with active cancer who develop ACS have longer lengths of hospital stay (7.9 days vs. 5.6 days, p < 0.001), higher costs of care ($86,576 vs. $79,916, p < 0.001), and increased mortality (15.4% vs. 7.5%, p < 0.001) when compared to patients without cancer [54]. The cardiovascular mortality risk is highest in the first-year post-diagnosis for all cancer types, with endometrial, laryngeal, bladder cancer, and prostate cancer having the highest risk of mortality [55]. Finally, patients with metastases have worse outcomes post-acute myocardial infarction [56].
Invasive management of CAD in cancer
In patients with CAD and cancer, numerous studies have shown that coronary revascularization improves the safety of further oncologic treatment and thereby increases long-term survival [42••, 57,58,59, 60••]. Cancer should not prohibit evaluation with coronary angiography and possible PCI in a patient presenting with ACS. Multiple studies have shown that patients with cancer are less likely to receive PCI when compared to those without cancer, despite otherwise having an indication for revascularization [53, 56]. A retrospective study by Balanescu et al. comprising over 200 patients with cancer and ACS suggested a survival benefit at 1 year, when coronary angiography was performed within 72 h of presentation (HR = 0.327, p < 0.0001) [59]. Another study showed that a conservative strategy with medical management for ACS had worse outcomes at 1 year [61].
Type 2 myocardial infarction, a mismatch between myocardial oxygen supply demand, is likely the most frequent cause of ACS in cancer patients, often presenting with symptoms ranging from dyspnea, atypical chest pain, and hypotension [62, 63]. NSTEMI patients presenting with symptoms of shock, heart failure, refractory angina, or sustained ventricular arrhythmias need an early invasive approach as opposed to medical management [64].
Numerous factors such as the presence of active cancer, current oncologic treatment, and cancer-related co-morbidities (frailty, anemia, thrombocytopenia, nutritional/performance status) require the clinician to personalize the management plan with the help of a multidisciplinary team comprising of a cardiologist, interventional cardiologist, and an oncologist.
Medical therapy for CAD and ACS
Aspirin should be given to all patients presenting with ACS and it has been shown to reduce non-fatal reinfarction and mortality [65]. In a study involving 456 cancer patients with ACS, aspirin use improved 1-year survival (34% vs. 18%, p < 0.001) [63]. In the same study, it was noted that only 46% of patients were given aspirin (due to thrombocytopenia, allergies, and recent major bleed) and STEMI patients were more likely to be prescribed aspirin compared to those with NSTEMI (66% vs. 43%, p < 0.004). Sarkiss et al. showed that aspirin improved overall survival in cancer patients with ACS and thrombocytopenia (platelet count < 100,000/mm3), with a 1-week survival rate close to 90% vs. 6% in patients who did not receive it [66]. The Society of Coronary Angiography and Intervention (SCAI) consensus guidelines suggest using aspirin in all patients with platelet counts > 10,000/mm3 [60••].
Beta-blockers, first-line agents in ACS, are contraindicated in the presence of cardiogenic shock or conduction abnormalities [5], which were found by Yusuf et al. to improve overall 1-year survival in cancer patients presenting with ACS, with about a 36% reduction in mortality (HR 0.64; 95% CI 0.51–0.81, p < 0.0002) [63]. Statins help control LDL, prevent the progression of atherosclerosis, and therefore are part of the standard of care for ACS and CAD [67, 68]. Studies have reported a wide range of utilization of statin (20.6–90.9%) in cancer patients presenting with ACS [63, 69]. Statin use has been associated with higher overall survival in cancer patients with ACS (0.39 vs. 0.22, p < 0.001) [63].
Current guidelines recommend dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (preferably prasugrel or ticagrelor) for at least 1 year in patients presenting with ACS undergoing PCI [70]. Clopidogrel is generally recommended as a second agent in patients with a higher bleeding risk, including cancer patients [70, 71]. Moreover, the SCAI expert consensus statement recommends against ticagrelor or prasugrel if the platelet count is < 50,000/mm3 [60••]. Platelet counts less than 30,000/mm3 need a risk/benefit analysis of preventing ischemia with the high risk of bleeding. Guo et al. performed a propensity-matched analysis comparing the occurrence of ischemic and bleeding events between 416 patients with 768 patients without active or prior cancer. The authors calculated the DAPT score in patients with and without cancer and found that patients with a DAPT score ≥ 2 had a higher risk of MI, stent thrombosis, and revascularization than those with DAPT < 2 [72]. Although cancer patients were excluded from the DAPT trial, the hazard ratios for the outcome measures were similar, suggesting that the DAPT score can be applied to cancer patients.
In a recent study by Mehran et al., among high bleeding risk patients (about 35% of patients had ACS) undergoing PCI with cobalt-chromium everolimus-eluting stents, DAPT (aspirin and predominantly clopidogrel) for 1 or 3 months was non-inferior to 6 or 12 months of DAPT for ischemic outcomes and may be associated with less major bleeding and a low incidence of stent thrombosis [73]. Similarly, Valgimigli et al. also proved non-inferiority with 1 month of DAPT compared to 3 months of DAPT. Their study involved 4434 patients with high bleeding risk undergoing PCI with a sirolimus-eluting coronary stent. About 49% of the patients had an ACS presentation, with over 15.2% of randomized patients having a history of cancer [94]. They reported similar net clinical adverse events in both the 1-month (7.5%) and 3-month (7.7%) groups, p < 0.0001 for non-inferiority, and there was less significant bleeding in the 1-month group vs. the 3-month group, 6.5% vs. 9.4, p < 0.001 for superiority [74]. Using DAPT for a month, followed by a single agent after PCI would be the ideal scenario for cancer patients with a high risk of bleeding. In a study aimed to assess the safety of starting or resuming cancer treatment within 6 months of DES placement, abbreviated aspirin and P2Y12 inhibitor treatment, and advanced cancer were significantly associated with OS, while DAPT discontinuation < 6 months after PCI was not associated with stent thrombosis or in-stent restenosis [75••].
Cancer patients have a higher propensity for thrombosis and atrial fibrillation and there is an increased need for anticoagulation. Triple therapy further increases the risk of bleeding, may delay cancer treatment, and is generally avoided in the setting of significant thrombocytopenia [76,77,78]. Overall, if there are no contraindications, optimal medical therapy should be in place as there are worse outcomes if patients with ACS are undertreated with beta-blockers, anticoagulants, angiotensin-converting enzyme inhibitors, and statins [51, 79]. Cancer therapy should be held in the acute situation. Rechallenging the patient with the same chemotherapy or a different agent is a complex decision that often requires a team-based approach.
Percutaneous coronary intervention considerations
Although PCI remains the gold standard revascularization therapy in cancer patients, it is still underutilized. Compared to non-cancer patients, patients with cancer are less likely to receive PCI for STEMI (54.2–70.6% vs. 82.3%) [80]. PCI in cancer patients with CAD poses unique and challenging concerns, in terms of frailty, increased bleeding/thrombotic risk, and need for subsequent cancer treatment [43]. PCI also significantly reduces mortality in cancer patients with ACS compared to medical management alone [81]. Predictors of poor long-term mortality outcomes in patients admitted for STEMI include a recent diagnosis of cancer (< 1 year) and the presence of metastatic disease [82]. If a patient is not considered a candidate for DAPT or an urgent non-cardiac procedure is planned, then balloon angioplasty may be considered [60••]. Kim et al. showed that utilization of fractional flow reserve (FFR) along with quantitative coronary angiography (QCA) lead to reduced number of unnecessary revascularizations and medical therapy [83••]. Adopting an FFR cutoff of < 0.75, they reclassified severe stenotic lesions (QCA > 70%) that needed treatment.
Stent choice
Although bare metal stents (BMS) were once preferred in cancer patients, due to their higher bleeding risk and perceived need for a shorter course of DAPT, currently third-generation drug-eluting stents (DES) are preferred due to their lower risk of restenosis and in-stent thrombosis [84]. Ahmed et al. compared the use of BMS vs. DES in cancer patients undergoing PCI, with a focus on all-cause mortality and the number of revascularizations. Their study showed that there was no significant difference in both endpoints between the two types of stents [85••].
A retrospective study including 75 cancer patients conducted by Balanescu et al. compared outcomes of various new generation DES (Synergy, Resolute, Integrity, Xience, Ion, or Promus) after PCI and found no significant differences in survivorship [75••]. No in-stent thrombosis (IST) was noted, and only one patient had 95% in-stent restenosis (ISR), despite being on DAPT for > 1 year, which was attributed to radiation therapy-induced heart disease. Only 2 out of these 51 patients resumed treatment after 6 months, with the median time of resumption being 14 days for chemotherapy and 10 days for radiation therapy. Although retrospective data is inherently limited, evidence shows that newer generation DES may tolerate a shorter duration of DAPT (< 6 months) and it may be safer to restart cancer treatment quickly (< 6 months, but as early as 2 weeks). The newer generation DES possesses a reduced stent strut thickness and a unique drug fast-release profile that results in less powerful inhibition of intimal hyperplasia and rapid endothelialization, thereby reducing the risk of thrombosis.
A single-center prospective study in cancer patients with a recently placed DES (within 1–12 months), who needed early discontinuation of their DAPT, showed that optical coherence tomography (OCT) imaging can be used to identify those at low risk for discontinuation and can thus proceed with their cancer-related surgery or procedures [86]. A similar study using OCT to evaluate stent healing after DES placement showed adequate stent healing in cancer patients, despite a short course of DAPT (< 6 months) in over 61% of patients [87].
Routine use of intracoronary imaging such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) leads to superior outcomes, especially when shorter durations of DAPT are required [88,89,90]. Such an approach can avoid stent under-sizing and malapposition and residual untreated complications such as edge dissections. It also helps avoid bifurcation and overlapping stents, which can increase the risk of stent thrombosis, which cancer patients are at a specifically high risk for [60••, 72]. It is critical to reemphasize that intracoronary imaging is of paramount importance for cancer patients, where it could additionally assist with management decisions in terms of whether it is safe to discontinue DAPT early (in patients who need procedures or surgical treatment) or to resume chemotherapy.
Special considerations
Chronic thrombocytopenia
Thrombocytopenia (TP) is a major concern prior to cardiac catheterization in more than 10–25% of cancer patients (especially those with hematological malignancies, breast, ovarian, and germ cell tumors) and remains a relative contraindication for the procedure [91]. Approximately 10% of these patients have platelet counts less than 100,000/mm3. TP does not reduce ischemic events, but rather increases the incidence of thrombus formation, suggesting that platelet function is a more important determinant for assessing procedural risk than the count [92, 93]. Various platelet thresholds have been suggested by the SCAI and ESC guidelines [42••, 60••]. Transfusion is indicated by the oncology teams usually when platelet counts are < 10,000/mm3 or when associated with active bleeding. In genitourinary and gastrointestinal tumors, the threshold for transfusion is < 20,000/mm3, given their propensity for intracavitary bleeding [94]. Most invasive procedures can be performed when the platelet count is > 50,000/mm3 and PCI with good hemostatic technique and minimal bleeding risk can be performed at counts > 30,000/mm3 [95]. Coronary artery bypass grafting like most general surgical procedures requires a threshold of > 50,000/mm3.
Thromboelastography (TEG) is a hemostatic test which measures the clotting efficacy of blood and can provide dynamic measures of the kinetics, strength, and stability of the fibrin clot [96, 97]. In a study including 70 cancer patients who underwent TEG prior to cardiac catheterization, Agha et al. found that a platelet count of < 50,000/mm3 was significantly associated with risk of hypocoagulability on TEG (p < 0.0001) along with worse overall survival at 24 months compared with platelet count > 100,000/mm3. Despite a perceived higher risk of bleeding, these patients did not have any substantial bleeding complications, suggesting that TP should not be a hindering factor for coronary revascularization when indicated [98••]. Although all the patients with a platelet count < 20,000/mm3 were hypocoagulable, about 75% of the patients with a platelet count between 20 and 49,000/mm3 and 21.1% of the patients with a platelet count between 50 and 99,999/mm3 were hypocoagulable, questioning the utility of routine TEG prior to catheterization. TEG may play a more important role in hematological malignancies such as acute leukemia or multiple myeloma where platelet function is expected to be deranged. The authors suggest performing a TEG when the platelet count is < 50,000/mm3 and in liquid tumors, where a normal TEG can embolden the operator to perform more invasive procedures. In patients with an abnormal TEG, appropriate products can be transfused to reduce bleeding risk.
Vascular access
High-risk PCI along with the Impella CP usually necessitates two arterial vascular accesses if diagnostic or interventional procedures are needed. Marmagkiolis et al. have developed the single-access, dual-injection technique (SADIT), wherein after the Impella CP has been inserted in the left ventricle, subsequent 6F and 4F sheaths are placed at the “10 o clock” and “5 o clock” positions [99]. The Single access for Hi-risk PCI (SHiP), described by Wollmuth et al., involves placing up to a 7F sheath within the 14 French Impella sheath [100]. These techniques eliminate unnecessary bleeding complications from extra access sites, especially in cancer patients, who are at high risk for bleeding.
Coronary artery bypass grafting
Coronary artery bypass grafting (CABG) is generally indicated in patients with critical left main disease, triple vessel disease, or those with complex coronary anatomy, whose expected survival is > 12 months [101•]. The 5-year post-operative survival rate was > 50% in patients with solid tumors and concomitant CAD undergoing CABG, thereby reinstating that cardiac surgery is still an option, at least in patients with early-stage cancers [102]. Cancers involving the lung and esophagus may allow simultaneous CABG and tumor resection thereby lowering costs and reoperation trauma, but with a slightly longer operating time [103, 104]. Zhang et al. showed in their study that patients undergoing CABG and staged tumor surgery within 1–3 months had good outcomes in terms of no in-hospital deaths and cardiovascular adverse events [101•]. However, complications from CABG arise by the use of pre-operative chemotherapy (e.g., anthracyclines) which lead to a drop in cardiac function, or the use of radiation which leads to pericarditis, myocardial/valve, and lung injury [101•]. Bottom line, the timing of the surgery (simultaneous vs. staged) should be based on factors such as the tumor extent, prognosis, and pre-operative cardiac risk of cancer therapy [102].
Radiation-induced coronary artery disease
Medical therapy for RICAD should be based on traditional atherosclerotic CAD including aspirin, and risk factor control such as lowering LDL, blood pressure, and blood sugar levels. PCI with DES may play a role in flow limiting RICAD; however, there are few studies reporting outcomes [39]. Undergoing research is trying to answer questions regarding stent healing and optimize PCI outcomes using intravascular imaging. CABG may be difficult after chest radiotherapy due to scarring of both the mediastinum and the internal mammary artery [105].
Conclusion
The number of cancer survivors has grown substantially in the last two decades, as has their life expectancy. Individualizing coronary care in cancer patients with the help of a multidisciplinary approach is needed to improve outcomes. A cancer diagnosis should not automatically prevent these patients from receiving optimal medical therapy and PCI, if otherwise indicated, as both have been shown to improve outcomes in these patients. However, a multidisciplinary approach to CAD treatment is warranted in patients with cancer. Studies utilizing artificial intelligence on large national and community as well as tertiary-center registries could help fill the gap derived from the paucity of robust prospective randomized clinical trials in the realm of cardio-oncology [81, 106•, 107•, 108•].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Murphy SL, Kochanek KD, Xu JA, Arias E, National Center for Health Statistics (U.S.). Division of vital statistics. Mortality in the United States, 2020. Published Date: 12/22/2021. Series: NCHS data brief no. 427. URL: https://stacks.cdc.gov/view/cdc/112079
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–71.
Koene RJ, et al. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133(11):1104–14.
Giza DE, et al. Cancer as a risk factor for cardiovascular disease. Curr Oncol Rep. 2017;19(6):39.
Amsterdam EA, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139–228.
Balanescu DV, et al. A cancer paradox: machine-learning backed propensity-score analysis of coronary angiography findings in cardio-oncology. J Invasive Cardiol. 2019;31(1):21–6.
Falk E. Pathogenesis of atherosclerosis. J Am Coll Cardiol. 2006;47(8 Suppl):C7-12.
Steinberg D. Low density lipoprotein oxidation and its pathobiological significance. J Biol Chem. 1997;272(34):20963–6.
Balzan S, Lubrano V. LOX-1 receptor: a potential link in atherosclerosis and cancer. Life Sci. 2018;198:79–86.
Kim YW, Byzova TV. Oxidative stress in angiogenesis and vascular disease. Blood. 2014;123(5):625–31.
Ridker PM, et al. Effect of interleukin-1β inhibition with canakinumab on incident lung cancer in patients with atherosclerosis: exploratory results from a randomised, double-blind, placebo-controlled trial. Lancet. 2017;390(10105):1833–42.
Ridker PM, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342(12):836–43.
Voronov E, et al. IL-1 is required for tumor invasiveness and angiogenesis. Proc Natl Acad Sci U S A. 2003;100(5):2645–50.
Renehan AG, Zwahlen M, Egger M. Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer. 2015;15(8):484–98.
Lukanova A, et al. Risk of ovarian cancer in relation to prediagnostic levels of C-peptide, insulin-like growth factor binding proteins-1 and -2 (USA, Sweden, Italy). Cancer Causes Control. 2003;14(3):285–92.
Giovannucci E, et al. Diabetes and cancer: a consensus report. CA Cancer J Clin. 2010;60(4):207–21.
Kim DS, Scherer PE. Obesity, diabetes, and increased cancer progression. Diabetes Metab J. 2021;45(6):799–812.
Ramos-Garcia P, et al. Diabetes mellitus and oral cancer/oral potentially malignant disorders: a systematic review and meta-analysis. Oral Dis. 2021;27(3):404–21.
Yokode M, et al. Cholesteryl ester accumulation in macrophages incubated with low density lipoprotein pretreated with cigarette smoke extract. Proc Natl Acad Sci U S A. 1988;85(7):2344–8.
Valavanidis A, Vlachogianni T, Fiotakis K. Tobacco smoke: involvement of reactive oxygen species and stable free radicals in mechanisms of oxidative damage, carcinogenesis and synergistic effects with other respirable particles. Int J Environ Res Public Health. 2009;6(2):445–62.
Yue W, et al. The hypertension related gene G-protein coupled receptor kinase 4 contributes to breast cancer proliferation. Breast Cancer (Auckl). 2021;15:11782234211015752.
Mosseri M, et al. In vitro evidence that myocardial ischemia resulting from 5-fluorouracil chemotherapy is due to protein kinase C-mediated vasoconstriction of vascular smooth muscle. Cancer Res. 1993;53(13):3028–33.
Das SK, Das AK, William M. 5-Fluorouracil-induced acute coronary syndrome. Med J Aust. 2019;211(6):255-257.e1.
Chong JH, Ghosh AK. Coronary Artery vasospasm induced by 5-fluorouracil: proposed mechanisms, existing management options and future directions. Interv Cardiol. 2019;14(2):89–94.
Van Cutsem E, et al. Incidence of cardiotoxicity with the oral fluoropyrimidine capecitabine is typical of that reported with 5-fluorouracil. Ann Oncol. 2002;13(3):484–5.
Herrmann J, et al. Vascular toxicities of cancer therapies: the old and the new—an evolving avenue. Circulation. 2016;133(13):1272–89.
Scappaticci FA, et al. Arterial thromboembolic events in patients with metastatic carcinoma treated with chemotherapy and bevacizumab. J Natl Cancer Inst. 2007;99(16):1232–9.
Schutz FA, et al. Bevacizumab increases the risk of arterial ischemia: a large study in cancer patients with a focus on different subgroup outcomes. Ann Oncol. 2011;22(6):1404–12.
Choueiri TK, et al. Risk of arterial thromboembolic events with sunitinib and sorafenib: a systematic review and meta-analysis of clinical trials. J Clin Oncol. 2010;28(13):2280–5.
Caldemeyer L, et al. Long-term side effects of tyrosine kinase inhibitors in chronic myeloid leukemia. Curr Hematol Malig Rep. 2016;11(2):71–9.
Keswani AN, et al. Rituximab-induced acute ST elevation myocardial infarction. Ochsner J. 2015;15(2):187–90.
Hanchate LP, Sharma SR, Madyalkar S. Cisplatin induced acute myocardial infarction and dyslipidemia. J Clinical Diagn Res. 2017;11(6):OD05-OD07.
Méndez-Toro A, Díaz-Brochero C, Acosta-Gutiérrez E. Carfilzomib induced cardiotoxicity in a multiple myeloma patient. Cardio-Oncology. 2020;6(1):17.
Baum M, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet. 2002;359(9324):2131–9.
Oliveira GH, et al. Cardiovascular risk assessment and management of patients undergoing hematopoietic cell transplantation. Bone Marrow Transplant. 2021;56(3):544–51.
Palaskas N, et al. Immune checkpoint inhibitor myocarditis: pathophysiological characteristics, diagnosis, and treatment. J Am Heart Assoc. 2020;9(2): e013757.
Drobni ZD, et al. Association between immune checkpoint inhibitors with cardiovascular events and atherosclerotic plaque. Circulation. 2020;142(24):2299–311.
• Laenens D, et al. Incidence of cardiovascular events in patients treated with immune checkpoint inhibitors. J Clin Oncol 2022;40(29):3430–3438. This paper suggests the various long term side effects associated with ICIs.
Yang EH, et al. Radiation-induced vascular disease—a state-of-the-art review. Front Cardiovasc Med. 2021;8: 652761.
Plana JC, et al. Multi-modality imaging in the assessment of cardiovascular toxicity in the cancer patient. JACC Cardiovasc Imaging. 2018;11(8):1173–86.
Balanescu DV, et al. Refractory radiation-induced coronary artery disease: mapping the path and guiding treatment with optical coherence tomography. Int J Cardiovasc Imaging. 2019;35(5):759–60.
•• Lyon AR, et al. ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022;43(41):4229–4361. First official European Society of Cardiology guidelines on Cardio-oncology.
Gevaert SA, et al. Evaluation and management of cancer patients presenting with acute cardiovascular disease: a Consensus Document of the Acute CardioVascular Care (ACVC) association and the ESC council of Cardio-Oncology-Part 1: acute coronary syndromes and acute pericardial diseases. Eur Heart J Acute Cardiovasc Care. 2021;10(8):947–59.
Giza DE, et al. Stress-induced cardiomyopathy in cancer patients. Am J Cardiol. 2017;120(12):2284–8.
Abdelghany M, Liu K. Diagnosis and management of stress-induced cardiomyopathy in cancer patients. Am J Cardiol. 2018;121(8):1011.
Munoz E, et al. Takotsubo stress cardiomyopathy: “good news” in cancer patients? J Am Coll Cardiol. 2016;68(10):1143–4.
Lyon AR, et al. Pathophysiology of Takotsubo syndrome. J Am Coll Cardiol. 2021;77(7):902–21.
Cuddy S, et al. Incidental coronary artery calcification in cancer imaging. JACC: Cardio Oncol. 2019;1(1):135–137.
Lopez-Mattei JC, et al. Cardiac computed tomography in cardio-oncology: JACC: CardioOncology Primer. JACC CardioOncol. 2021;3(5):635–49.
Baldassarre LA, et al. Advances in multimodality imaging in cardio-oncology: JACC state-of-the-art review. J Am Coll Cardiol. 2022;80(16):1560–78.
Kurisu S, et al. Comparison of treatment and outcome of acute myocardial infarction between cancer patients and non-cancer patients. Int J Cardiol. 2013;167(5):2335–7.
Yousif N, et al. Impact of malignancy on clinical outcomes in patients with acute coronary syndromes. Int J Cardiol. 2021;328:8–13.
Mrotzek SM, et al. Assessment of coronary artery disease during hospitalization for cancer treatment. Clin Res Cardiol. 2021;110(2):200–10.
Giesen Z, Sullivan M, Gemignani A. Myocardial infarction in hospitalized patients with cancer. J Am College Cardiol. 2018;71(11_Supplement):A1306-A1306.
Sturgeon KM, et al. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur Heart J. 2019;40(48):3889–97.
Bharadwaj A, et al. Acute myocardial infarction treatments and outcomes in 6.5 million patients with a current or historical diagnosis of cancer in the USA. Eur Heart J. 2019.
Donisan T, et al. Cardiac interventional procedures in cardio-oncology patients. Cardiol Clin. 2019;37(4):469–86.
Pushparaji B, et al. State-of-the-art review: interventional onco-cardiology. Curr Treat Options Cardiovasc Med. 2020;22(5):11.
Balanescu DV, et al. Acute myocardial infarction in a high-risk cancer population: outcomes following conservative versus invasive management. Int J Cardiol. 2020;313:1–8.
•• Iliescu CA, et al. SCAI Expert consensus statement: evaluation, management, and special considerations of cardio-oncology patients in the cardiac catheterization laboratory (endorsed by the Cardiological Society of India, and Sociedad Latino Americana de Cardiologıa Intervencionista). Catheter Cardiovasc Interv. 2016;87(5):E202-E223.This is the first official set of guidelines put forth by SCAI in the realm of cario-oncology.
Styczkiewicz K, et al. Clinical presentation and treatment of acute coronary syndrome as well as 1-year survival of patients hospitalized due to cancer: a 7-year experience of a nonacademic center. Medicine (Baltimore). 2020;99(5): e18972.
Baron T, et al. Type 2 myocardial infarction in clinical practice. Heart. 2015;101(2):101–6.
Yusuf SW, et al. Treatment and outcomes of acute coronary syndrome in the cancer population. Clin Cardiol. 2012;35(7):443–50.
Patel MR, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2016 appropriate use criteria for coronary revascularization in patients with acute coronary syndromes: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2017;69(5):570–91.
ISIS-2 Collaborative Group. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction. ISIS-2. Lancet. 1988;49-360.
Sarkiss MG, et al. Impact of aspirin therapy in cancer patients with thrombocytopenia and acute coronary syndromes. Cancer. 2007;109(3):621-627.
Wilt TJ, et al. Effectiveness of statin therapy in adults with coronary heart disease. Arch Intern Med. 2004;164(13):1427-1436.
Sposito AC, Chapman MJ. Statin therapy in acute coronary syndromes: mechanistic insight into clinical benefit. Arterioscler Thromb Vasc Biol. 2002;22(10):1524–34.
Iannaccone M, et al. Prevalence and outcome of patients with cancer and acute coronary syndrome undergoing percutaneous coronary intervention: a BleeMACS substudy. Eur Heart J Acute Cardiovasc Care. 2018;7(7):631–8.
Collet JP, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289–367.
Wallentin L, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57.
Guo W, et al. Cancer patients have a higher risk of thrombotic and ischemic events after percutaneous coronary intervention. JACC: Cardiovasc Interv. 2021;14(10):1094–1105.
Mehran R, et al. 3- or 1-month DAPT in patients at high bleeding risk undergoing everolimus-eluting stent implantation. JACC Cardiovasc Interv. 2021;14(17):1870–83.
Valgimigli M, et al. Dual antiplatelet therapy after PCI in patients at high bleeding risk. N Engl J Med. 2021;385(18):1643–55.
•• Balanescu DV, et al. Cancer treatment resumption in patients with new-generation drug-eluting stents. Coron Artery Dis. 2021;32(4). Findings from this study that with outcomes are comparable with shorter duration of DAPT along with quicker cancer treatment resumption in patients who were recently stented.
Urban P, et al. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N Engl J Med. 2015;373(21):2038–47.
Kandzari DE, et al. One-month dual antiplatelet therapy following percutaneous coronary intervention with zotarolimus-eluting stents in high-bleeding-risk patients. Circ Cardiovasc Interv. 2020;13(11): e009565.
McCarthy CP, Steg G, Bhatt DL. The management of antiplatelet therapy in acute coronary syndrome patients with thrombocytopenia: a clinical conundrum. Eur Heart J. 2017;38(47):3488–92.
Park JY, et al. Acute coronary syndromes in patients with active hematologic malignancies — incidence, management, and outcomes. Int J Cardiol. 2019;275:6–12.
Kanenawa K, et al. Clinical outcomes after percutaneous coronary intervention in patients with cancer. Circ J. 2021;85(6):837–46.
Monlezun DJ, et al. Machine learning-augmented propensity score analysis of percutaneous coronary intervention in over 30 million cancer and non-cancer patients. Front Cardiovasc Med. 2021;8: 620857.
Takeuchi T, et al. The effect of a cancer history on patients with acute myocardial infarction after percutaneous coronary intervention insights from the OACIS registry. Int Heart J. 2021;62(2):238–45.
•• Kim JW, et al. Reclassification of treatment strategy with fractional flow reserve in cancer patients with coronary artery disease. Medicina (Kaunas). 202;58(7). Findings from this study suggest the use of FFR to efficiently use coronary interventions and minimize stenting.
Neupane S, et al. Meta-analysis of drug eluting stents compared with bare metal stents in high bleeding risk patients undergoing percutaneous coronary interventions. Catheter Cardiovasc Interv. 2019;94(1):98–104.
••Ahmed T, et al. Percutaneous coronary intervention in patients with cancer using bare metal stents compared to drug-eluting stents. Front Cardiovasc Med. 2022;9:901431. Findings from this study suggest the use of newer generation DES in cancer patients.
Iliescu CA, et al. “Bringing on the light” in a complex clinical scenario: optical coherence tomography-guided discontinuation of antiplatelet therapy in cancer patients with coronary artery disease (PROTECT-OCT registry). Am Heart J. 2017;194:83–91.
Aziz MK, et al. Coronary stent healing in cancer patients—an optical coherence tomography perspective. Front Cardiovasc Med. 2021;8: 665303.
Kirtane AJ, et al. Primary results of the EVOLVE short DAPT study: evaluation of 3-month dual antiplatelet therapy in high bleeding risk patients treated with a bioabsorbable polymer-coated everolimus-eluting stent. Circ Cardiovasc Interv. 2021;14(3): e010144.
Shin DH, et al. Effects of intravascular ultrasound-guided versus angiography-guided new-generation drug-eluting stent implantation: meta-analysis with individual patient-level data from 2,345 randomized patients. JACC Cardiovasc Interv. 2016;9(21):2232–9.
Zhang J, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE trial. J Am Coll Cardiol. 2018;72(24):3126–37.
Elting LS, et al. Incidence, cost, and outcomes of bleeding and chemotherapy dose modification among solid tumor patients with chemotherapy-induced thrombocytopenia. J Clin Oncol. 2001;19(4):1137–46.
Luzzatto G, Schafer AI. The prethrombotic state in cancer. Semin Oncol. 1990;17(2):147–59.
Kroll MH, Feng S. Targeting shear stress-induced platelet activation: is lesion-specific antiplatelet therapy a realistic clinical goal? Expert Rev Cardiovasc Ther. 2005;3(5):941–51.
Giza DE, et al. Management of CAD in patients with active cancer: the interventional cardiologists’ perspective. Curr Cardiol Rep. 2017;19(6):56.
Iliescu C, Durand J-B, Kroll M. Cardiovascular interventions in thrombocytopenic cancer patients. Tex Heart Inst J. 2011;38(3):259–60.
Abdelfattah K, Cripps MW. Thromboelastography and rotational thromboelastometry use in trauma. Int J Surg. 2016;33(Pt B):196–201.
Khurana S, et al. Monitoring platelet glycoprotein IIb/IIIa-fibrin interaction with tissue factor-activated thromboelastography. J Lab Clin Med. 1997;130(4):401–11.
•• Agha AM, et al. Identifying hemostatic thresholds in cancer patients undergoing coronary angiography based on platelet count and thromboelastography. Front Cardiovasc Med. 2020;7(9). Study suggests the use of thromboelastogram as a way to objectively measure bleeding risk prior to PCI in thrombocytopenic cancer patients.
Marmagkiolis K, et al. Single-access dual-injection technique (SADIT) for high-risk PCI with Impella CP. Catheter Cardiovasc Interv. 2021;98(6):1138–40.
Wollmuth J, et al. The Single-access for Hi-risk PCI (SHiP) technique. Catheter Cardiovasc Interv. 2020;96(1):114–6.
• Zhang MK, et al. Coronary artery bypass grafting in patients with malignancy: a single-institute case series of eight patients. BMC Surg. 2022;22(1):359. Single center experience on timing of CABG in cancer patients.
Garatti A, et al. Coronary artery bypass grafting in patients with concomitant solid tumours: early and long-term results. Eur J Cardiothorac Surg. 2020;58(3):528–36.
Li Z, et al. Effect of simultaneous surgical treatment of severe coronary artery disease and lung cancer. J Int Med Res. 2018;47(2):591–9.
Zhang W, et al. Combined surgical treatment of esophageal cancer and coronary heart diseases in elderly patients. World Journal of Surgical Oncology. 2018;16(1):213.
Handa N, et al. Coronary artery bypass grafting in patients with previous mediastinal radiation therapy. J Thorac Cardiovasc Surg. 1999;117(6):1136–42.
• Monlezun DJ, et al. Artificial intelligence-augmented propensity score, cost effectiveness and computational ethical analysis of cardiac arrest and active cancer with novel mortality predictive score. Medicina. 2022;58(8):1039. This AI-guided empirical and ethical analytical study provides a novel demonstration of LHC mortality reductions in cardio-oncology cardiac arrest and related disparities.
• Chauhan S, et al. Fractional flow reserve cardio-oncology effects on inpatient mortality, length of stay, and cost based on malignancy type: machine learning supported nationally representative case-control study of 30 million hospitalizations. Medicina. 2022;58(7):859. This study suggest that FFR-guided PCI may be safely utilized in patients with cancer as it does not significantly increase inpatient mortality, complications, and LOS.
• Thomason N, et al. Percutaneous coronary intervention in patients with gynecological cancer: machine learning-augmented propensity score mortality and cost analysis for 383,760 patients. Front Cardiovasc Med. 2022;8. This large propensity score analysis suggests that PCI may cost inefficiently reduce mortality for gynecological cancer patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Bala Pushparaji declares that he has no conflict of interest. Teodora Donisan declares that she has no conflict of interest. Dinu Valentin Balanescu declares that he has no conflict of interest. Jong Kun Park declares that he has no conflict of interest. Dominique J. Monlezun declares that he has no conflict of interest. Abdelrahman Ali declares that he has no conflict of interest. Ibrahim Halil Inanc declares that he has no conflict of interest. Jaime Caballero declares that he has no conflict of interest. Mehmet Cilingiroglu declares that he has no conflict of interest. Konstantinos Marmagkiolis declares that he has no conflict of interest. Cezar Iliescu declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pushparaji, B., Donisan, T., Balanescu, D.V. et al. Coronary Revascularization in Patients With Cancer. Curr Treat Options Cardio Med 25, 143–158 (2023). https://doi.org/10.1007/s11936-023-00982-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11936-023-00982-9