Abstract
Purpose of review
With the evolution in digital medicine to identify and monitor cardiac electrophysiological (EP) conditions, increased access to cardiac implantable electronic devices (CIEDs), and reimbursements for non-face-to-face care, remote patient monitoring (RPM) is becoming a key part of the EP service line. RPM of cardiac electrophysiological conditions including the use of CIEDs has improved the quality of care and high patient satisfaction and proved to be cost-effective. The focus of this review is literature on RPM in EP, evidence from randomized trials, and observational studies including those of Apple Watch and future of CIEDs.
Recent findings
RPM has progressed to use implantable devices and wearable technologies like sensors embedded in smartphones and apps. American College of Cardiology recently launched a digital transformation network to support digital navigation and RPM across different cardiovascular diseases.
Summary
The information presented here can inform healthcare providers of the most widely implemented and effective forms of RPM for patients with chronic EP conditions.
Similar content being viewed by others
Introduction
The term “remote patient monitoring” (RPM) and sometimes known as “remote patient management” means monitoring of patients outside the traditional hospital or doctor office settings. Remote patient monitoring uses digital technologies to collect medical and other forms of health data from individuals in one location and electronically transmit that information securely to healthcare providers in a different location for assessment and recommendations. This type of service allows a provider to continuously track healthcare data of a patient once released to home or a care facility that needs continuous monitoring [1].
RPM devices can collect a variety of important individualised data, such as blood sugar, blood pressure, blood oxygen saturation level, heart rhythm/rate, etc. [1]. This seclusive data is then transmitted to health professionals in facilities such as monitoring centers in primary care settings, hospitals and intensive care units, skilled nursing facilities, and centralized off-site case management programs. Health professionals monitor each patient remotely and act on the information received as part of the treatment plan.
The advantages of RPM of patients include early and real-time detection of illnesses, prevention of worsening of illnesses, decrease in cost by reduction in hospitalizations, and monitoring efficacy through accurate readings while permitting usual daily activities for patients and improve efficiency in healthcare services by utilizing communication technology [2]. As the US population ages, the number of people suffering from chronic diseases such as diabetes, heart conditions, or neurodegenerative diseases will increase. The chronic nature of their conditions means that a lapse of attention or knowledge could result in their condition suddenly worsening, accompanied by a trip to the hospital emergency room. This is especially true in patients with cardiac diseases, where RPM could improve outcomes by more timely identification of new or worsening medical conditions (such as arrhythmia or heart failure (HF)) and the detection of device-related problems [3] and also decrease in the cost in the management of these patients [4, 5].
With increased smartphone use and advancement in mobile health technologies and sensors, as well as new codes designed to reimburse chronic care management and monitoring, RPM can become a major driver in health-care quality improvement and also additional source of revenue for EP practitioners. The purpose of this review is to increase awareness about the latest technology trends and share evidence so RPM can be adequately utilized for relevant procedures and conditions.
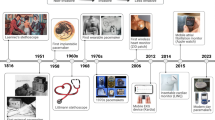
Digital medicine and evolution of RPM
With the evolution in technology, RPM has transitioned from capturing remote data through telephonic conversations, video conference, or where the patient enters his own health record into a secure website or smart phone to utilizing automated devices (e.g., biosensors devices) which focus on patients with chronic diseases who need continuous care and monitoring [6]. The digital technology available today has given the opportunity to choose from a variety of options that use cellular, satellite networks to communicate and follow up the patients with CIEDs. There is an ever-improving capability to remotely monitor the patient’s health, device function, or check battery life without disturbing the routine of the patient [7]. Wireless capabilities with home transmitters that communicate automatically and relay data to the physician are offered by most major companies, which lead to an easier monitoring and follow-up of the patient.
Digital medicine (including apps, telemedicine, ePROs, machine learning) is now seen as an important tool to bridge gaps in healthcare delivery and to provide continuous engagement for patients with chronic diseases [8,9,10]. Since the majority of patients with chronic conditions spend less than a few hours per year face-to-face with their provider(s), digital resources that enable home-based monitoring and engagement can provide proactive care, reduce emergency department (ED) visits, and provide higher quality care [10, 11]. There is emerging evidence that a higher quality of care is delivered when traditional healthcare is augmented by ePROs and digital therapeutic interventions directly at patients’ homes [12,13,14,15,16]. A recently published meta-analysis of 13 remote monitoring studies in heart failure reported a significant reduction in mortality (risk ratio of 0.76; 95% confidence interval [CI] of 0.62–0.93) as compared to conventional care [15]. Similarly, a meta-analysis on ten randomized controlled trials on COPD patients found a significant reduction in emergency department visits (OR = 0.27; 95% CI = 0.11 to 0.66) [16]. With the approval of reimbursement codes for telemedicine and RPM, disease and symptom monitoring (and not just device-based monitoring) are likely to become a central part of clinical practice (Fig. 1). With the passion for more research and making the uncompromising development a continuous process, alot more can be learned with respect to delivery science and scaling of ePROs, mobile health, and the RPM of populations that are especially relevant to EP practitioners [10, 17]. See Table 1 for list of common EP-specific disease conditions best suited for RPM.
Remote monitoring in cardiac electrophysiology
Frequent RPM has improved the quality of patient’s life with multiple positive outcomes, including early detection of atrial fibrillation (AF) and reduction in inappropriate shocks from ICD which further lead to a decrease in mortality. The number of outpatient follow-ups and hospitalization is operatively reduced among RPM users which promoted decrease in health resource utilization and significant increase in cost savings. RPM users with early and high transmission rates have exceptional outcomes [18]. Early detection of atrial fibrillation or ventricular arrhythmias could lead to early intervention and potential prevention of stroke and heart failure exacerbation. The feasibility and benefits of RPM of CIEDs have been shown in several clinically significant concerns/events. RPM improves patient outcomes and can be especially beneficial to pediatric and congenital heart disease patients [19]. We have reviewed some of the common conditions in EP which are a good fit for RPM services (Table 1). Advances in cloud technology and widespread smartphone access have allowed patients with newer devices to transmit data directly using wireless technologies as well as receive instant notification and guidance, enabling an efficient RPM ecosystem (Fig. 1).
Atrial fibrillation
In the current medical practice, AF has been the most commonly encountered arrhythmia [20]. About 6–12 million in the USA by 2050 and 17.9 million in Europe by 2060 are predicted to be affected by atrial fibrillation [20,21,22]. Medical expenses are about $8705 higher per year in people with AFib than for those people who do not have AFib, and overall it costs the USA about $6 billion per annum [23, 24].
RPM has been an invaluable tool in the diagnosis and in the management of atrial fibrillation. The ability to monitor important physiologic parameters gives a great opportunity for healthcare professionals to reform the way they care for AF patients. RPM has the potential to reduce persistent or permanent AF through early identification and treatment of paroxysmal AF episodes. The efficacy of antiarrhythmic drug therapy, rate control, and catheter ablation procedures can be monitored by real-time RPM. Risk of stroke can be reduced through rapid initiation of anticoagulant therapy. It not only meliorates the quality of patient care but also reduces the healthcare costs associated with AF [25].
A 2016 study done by Cantillon et al. attempted to evaluate outcomes associated with an off-site central monitoring unit (CMU) applying standardized cardiac telemetry indications using electronic order entry. The CMU received electronic telemetry orders for 99,048 patients and provided 410534 notifications (48% arrhythmia/hemodynamic). About 3243 patients triggered the Emergency Response Team (ERT) activation, with rhythm/rate changes occurring 1 hr or less prior to the ERT activation in 979 patients (30%). The CMU detected and provided accurate notification for 772 (79%) of those events. This study concluded that among non–critically ill patients, use of standardized cardiac telemetry with an off-site central monitoring unit was associated with detection and notification of cardiac rhythm and rate changes within 1 hr prior to the majority of ERT activations and also with a reduction in the census of monitored patients, without an increase in cardiopulmonary arrest events [26].
Atrial fibrillation was detected more frequently by RM with implantable loop recorder in comparison to standard follow-up in patients with cryptogenic stroke in CRYSTAL-AF trial both at 6 and 12 months duration in comparison to standard follow-up (8.9% vs 1.4%, HR 6.4, 95% CI 1.9–21.7, p < 0.001 at 6 months; 12% vs 2%, HR 7.3, 95% CI 2.6–20.8, p < 0.001 at 12 months). The median time from randomization to detection of AF was 41 days with implantable loop recorders. This early identification of AF is important for prevention of recurrence of stroke in this high-risk population by early initiation of anticoagulation [7, 15].
Heart failure
Over the past several decades, the prevalence of HF has increased substantially. HF affects around 26 million people worldwide and thereby has been defined as a global pandemic [27]. HF was responsible for an estimated health expenditure of around $31 billion in 2012 that is more than 10% of the US total health expenditure for cardiovascular diseases [28]. A 127% increase in total costs is further expected between 2012 and 2030 [28]. There was a 13.5% decrease in age standardized death rate from heart failure between the years 2000 and 2009 [29]. But despite this, the risk of sudden cardiac arrest (SCD) has remained high among patients with HF which mostly results from arrhythmias and progressive pump failure [30]. The advent of cardiac implantable electronic devices (CIEDs) have opened the possibility for early detection of arrhythmias and estimate cardiac function in terms of cardiac indices such as stroke volume, ejection fraction, etc.
The new generation CIEDs can measure, store, and transmit data like thoracic impedance, heart rate, and patient activity. They are capable of predicting HF-related hospitalization days to weeks ahead [30]. CIEDs can give valuable information on the progression of the disease by monitoring patient’s physical activity [31]. A baseline reduction in intrathoracic impedance can specify possible decompensating HF and can predict it 10–14 days in advance by identifying increased fluid retention and left atrial wedge pressure. Compared to daily weight monitoring for predicting HF, intrathoracic impedance has shown to be superior. Fluid accumulation through pleural effusion or pneumonia in the pathway of intrathoracic impedance can limit its use [32,33]. Wireless pulmonary artery hemodynamic monitoring in chronic heart failure patients was done in a randomized single blinded controlled trial used to assess and support the assumption that implantable hemodynamic surveillance devices could decrease hospitalization rates in heart failure patients. In the treatment group, in addition to the standard of care versus standard of care alone in the control group, clinicians used daily measurement of pulmonary artery pressure. Over the next 6 months, 83 heart failure-related hospitalizations were reported in the treatment group (n = 270) compared to 120 in the control group (n = 280; 0·31 vs 0·44, 0·70, 95% CI 0·60–0·84, p < 0·0001). The treatment group had a 39% decrease in heart failure-related hospitalization compared to the control group over the entire follow-up (mean 15 months [SD 7]) (153 vs 253, HR 0·64, 95% CI 0·55–0·75; p < 0·0001). This demonstrated a substantial and significant reduction in hospitalization for NYHA Class III heart failure patients who were managed with a wireless hemodynamic monitoring scheme. Adding pulmonary artery pressure data to clinical signs and symptoms enables enhanced management of heart failure [34].
It is particularly important how RPM has affected heart failure patients with CIEDs. Since the past few decades, the number of CIED patients with heart failure has increased significantly. Using a single RPM platform, the implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME) study assessed if the outcome of heart failure patients would improve using RPM. A total of 664 patients were assigned randomly (716 enrolled) in which 333 to telemonitoring and 331 to control and monitored for a year. After 1 year, 63 (18·9%) of 333 telemonitor group patients versus 90 (27·2%) of 331 control group patients (p = 0·013) had a worsened composite score (0·63, 95% CI 0·43–0·90). Ten patients in the telemonitoring group versus 27 in the control group died during follow-up. Automatic, daily, implant-based, multiparameter telemonitoring for patients with heart failure can considerably enhance clinical results. The study demonstrated that implant-based telemonitoring resulted in significant improvement in composite clinical score and all-cause mortality compared to control population [34]. The CIED-based technologies available to monitor events specific to heart failure have improved, for example, many CIEDs can calculate transthoracic impedance, and the trends in these values can alert providers to an active or impending heart failure exacerbation, thus reducing risk of hospitalization and improving other clinical outcomes [35]. These device functions may be used in the comprehensive assessment of heart failure in a given patient rather than be used in isolation to diagnose and treat heart failure exacerbations [37].
In a Seamless User-Centered Proactive Provision of Risk-Stratified Treatment for Heart Failure (SUPPORT-HF) study which is a cohort study, Rahimi and colleagues presented an android-based easy-to-use monitoring system to lessen hospital readmissions and empower patients. The median age of this cohort was 77 years, and they had very little experience with devices. According to this study, the patients are very comfortable using this device and also described it as easy-to-use [35].
Bloodless, blood test
Variations in blood potassium levels can cause arrhythmias and death. Diagnosing hyperkalemia outside a hospital setting can be a challenge because of the absence of symptoms. The KardiaK Software Platform can screen for elevated blood potassium levels without requiring a blood sample from the patient. This software uses data from electrocardiogram (ECG) and detects hyperkalemia through artificial intelligence (AI) algorithm. Using AliveCor patients can record an ECG and check for hyperkalemia using KardiaK at home. KardiaK software was granted “Break through device” designation by the FDA while waiting for the approval [36,37].
Apple Watch EKG
New fitness trackers and smart watches are released to the consumer market every year. In addition to functioning as a timekeeping device, the initial smart watches kept track of a person’s movement, count of their daily steps and also detect a person’s heart rate during rest and workout. With the advances in technology, now these smart watches with special sensors can record tracing of a heart’s electrical signature (electrocardiogram or ECG) and alert a patient if it detects an irregular rhythm.
Apple Inc. advanced into digital healthcare device space with the release of the Apple watch 4 series, which helps to detect heart arrhythmias such as atrial fibrillation. Apple Watch looks for arrhythmias using a photoplethysmograph-based algorithm, and the ECG app on Apple Watch Series 4, which is capable of generating an ECG similar to a lead I electrocardiogram [38]. This app also classifies an ECG as sinus rhythm (SR), atrial fibrillation (AF), or inconclusive and reports high or low heart rate. Apple Inc. along with the Stanford University conducted a clinical trial to know how well the Apple watch detects important heart rhythm changes [39]. In this study a total of 419,297 people self-enrolled in the study. To participate in the study, participants should not have been diagnosed with AF or are taking anticoagulants and were required to have an Apple Watch and compatible iPhone. They were given information about the study when they downloaded the Heart Study app. Detection of five of six repeat tachograms of an irregular pulse within a 48-hr period triggered a notification to be sent via the app. Participants receiving a notification were prompted to contact the study doctor through the app for a video consultation to determine if the participant should wear an ECG patch. The patch was worn for up to 7 days.
The primary endpoints were AF > 30 seconds on ECG patch and simultaneous AF on ECG patch and tachogram. A pulse notification was received by 2161 participants (0.52%). Notification rates were most frequent in participants over age 65 (slightly > 3.0%) and lowest among those under 40 (0.16%). Patches were sent to 658 participants, and 450 were returned and included in the analysis. AF was identified in 34% of those who received a notification and wore the ECG patch.
“AF” can be paroxysmal, particularly early on in the course of the disease. It’s not surprising for it to go undetected in subsequent ECG patch monitoring. The positive predictive value (PPV) for the tachogram was 71%, and the PPV for notification was 84% (meaning if the watch notified the user of AF, so did the patch). About half of participants receiving an irregular pulse notification contacted a study doctor. Subsequent surveys showed that 57% of participants who received an alert sought medical care outside of the study regardless of whether they had been seen virtually by a study doctor. Early results from the study of Apple Watch users show the wearable device appears to detect atrial fibrillation (AF) with a high degree of accuracy. However the study had several limitations. It was not a randomized controlled trial and relied on self-reported data from participants. Additionally, the target enrolment of 500,000 participants, with 75,000 aged 65 or older, was not reached. However the watch is not designed to replace traditional medical devices. But given the lack of standards for widespread screening for AF, the Apple Watch could potentially detect a problem in someone who had no other known risk factors [40]. In September 2018, this product was categorized as class II received US-FDA clearance for over the counter use [41].
New reimbursement models for RPM
One of the major upsides for practices implementing RPM is the reimbursement mechanism that the Centers for Medicare & Medicaid Services (CMS) has been pioneering for remote care and RPM through connected care program. Chronic care management (CCM) services are generally non-face-to-face services provided to Medicare beneficiaries who have two or more chronic conditions expected to last at least 12 months or until the death of the patient [45]. These services are reimbursed through specific CPT codes per member per month bases (PM PM) (see Table 2 for list of reimbursement methods) [46].
In addition, for procedures and acute clinical episodes, CMS through its innovation center has released a new voluntary bundled payment model called Bundled Payments for Care Improvement Advanced (BPCI Advanced). These include payment for AMI(Acute myocardial infarction), cardiac arrhythmia, cardiac defibrillator, cardiac valve, congestive heart failure, coronary artery bypass grafting, pacemaker, and percutaneous coronary intervention (PCI) [47]. Outside the BPCI advanced enrollment, there are significant upsides for practices to use digital medicine by avoiding no-shows, improve preparation before procedures, decrease readmission rates, and enhance patient satisfaction and outcomes through close monitoring post procedures. The American College of Cardiology (ACC) recently launched digital transformation network practices to support digital toolkits for PCI, heart failure, and EP procedures using evidence-based care pathways (https://rx.health/cardiology/).
Limitations and continued challenges
Although there are significant benefits with RPM, there are some potential downsides. Expanding indications for ICD(Implantable Cardioverter-Defibrillator) and CRT(Cardiac Resynchronization Therapy) therapy leads to an unsustainable burden on device clinics [42]. There can be challenges in developing an efficient workflow for remote monitoring, as it requires review of multiple websites each day, according to how many device companies are utilized. In addition, these transmissions include a large amount of data that take significant time to review and process. There is potential for increased burden due to false alarms as well. Calling back and triaging patients are often required. Finally, there are no reprogramming capabilities remotely; therefore, patients do require an in-office evaluation if reprogramming is needed [43]. In patient with older generation CIEDs, the majority of visits involve data collection without reprogramming or change in patient medications or investigations (“nonactionable”). More significantly, patient or device events (lead malfunction or tachyarrhythmia therapy) may remain undetected for a prolonged period between device interrogations [42]. Fortunately, there are now many service providers that can be contracted for RPM-related services to offset the additional work and logistics required to run an effective RPM program.
Although the technology has many proven successes, certain RPM services still rely on patients to take an active role in their own health. Wireless technologies are also not suitable for some rural areas, and some older patients may not know how to use modern technologies like apps [44]. Any collected health information also needs to be encrypted and protected from hackers, and some RPM technologies are very expensive. The shift of accountability associated with RPM brings up liability issues. There are no clear guidelines in respect to whether clinicians have to intervene every time they receive an alert regardless of the urgency. The continuous flow of patient data requires a dedicated team to handle the information, which may, in fact, increase the workload. Although technology is introduced with the intent to increase efficiency, it can become a barrier to some healthcare providers that are not technological. Using service providers, which provide RPM as well as support reimbursement, can help address some of these challenges.
RPM incurs additional issues, including defining responsibilities (e.g., defining an acceptable amount of time for notifying a patient after identifying a possible problem), potential liability to health professionals if information provided by the device is not documented, maintaining patient confidentiality, and licensing issues with physicians who are monitoring patients in states in which they are not licensed to practice. Currently, manufacturers maintain remote follow-up data repositories and information regarding specific patients which can be accessed by designated providers through a password system. Database vulnerability remains a concern, and best practices in security and privacy need to be ensured to mitigate the risk [21]. Engagement with service providers and digital transformation networks (such as with ACC) allows personal training, pooled resources, indemnification support, and legal and reimbursement guidance for a network of multiple practices and health systems, enabling a more efficient and responsive care.
Conclusions
Patient care using RPM had added a new dimension in managing patients with procedures and chronic cardiac conditions. Even though there are multiple significant benefits to RPM for both patients and practices, it has remained underutilized. EP practitioners can now use evidence-based care developed for RPM to provide more effective care, improve outcomes, and enhance revenue for a variety of procedures and disease conditions ranging from arrhythmia screening, device-based monitoring, anticoagulation management to symptom, and ePRO monitoring. Participation in national society-led digital transformation networks can fast-track adoption, sharing of implementation science, and generation of rigorous evidence.
References and Recommended Reading
Dias D, Paulo Silva Cunha J. Wearable health devices—vital sign monitoring, systems and technologies. Sensors [Internet]. 2018 Jul 25 [cited 2019 Jun 26];18(8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6111409/
Malasinghe LP, Ramzan N, Dahal K. Remote patient monitoring: a comprehensive study. J Ambient Intell Humaniz Comput. 2019;10(1):57–76.
Afolabi BA, Kusumoto FM. Remote monitoring of patients with implanted cardiac devices - a review. J - Remote Monit Patients Implant Card Devices - Rev [Internet]. 2012 5 [cited 2019 Jun 27]; Available from: https://www.ecrjournal.com/articles/remote-monitoring-patients-ICD
Guédon-Moreau L, Lacroix D, Sadoul N, Clémenty J, Kouakam C, Hermida J-S, et al. Costs of remote monitoring vs. ambulatory follow-ups of implanted cardioverter defibrillators in the randomized ECOST study. Eur Eur Pacing Arrhythm Card Electrophysiol J Work Groups Card Pacing Arrhythm Card Cell Electrophysiol Eur Soc Cardiol. 2014;16(8):1181–8.
Zanaboni P, Landolina M, Marzegalli M, Lunati M, Perego GB, Guenzati G, et al. Cost-utility analysis of the EVOLVO study on remote monitoring for heart failure patients with implantable defibrillators: randomized controlled trial. J Med Internet Res. 2013;15(5):e106.
Vegesna A, Tran M, Angelaccio M, Arcona S. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed E-Health. 2017;23(1):3–17.
Remote monitoring of cardiac implantable electronic devices (CIED)Emily P. Zeitler, MD and Jonathan P. Piccini, MD MHS.
Elenko E, Underwood L, Zohar D. Defining digital medicine. Nature biotechnology. 2015;33(5):456–61.
Digital therapeutics: combining technology and evidence-based medicine to transform personalized patient care. https://www.dtxalliance.org. Accessed June 5, 2019.
Bhavnani SP, Parakh K, Atreja A, Druz R, Graham GN, Hayek SS, et al. 2017 Roadmap for innovation—ACC health policy statement on healthcare transformation in the era of digital health, big data, and precision health: a report of the American College of Cardiology Task Force on Health Policy Statements and Systems of Care. Journal of the American College of Cardiology. 2017;70(21):2696–718.
Atreja A. Smarter care for patients with inflammatory bowel disease: a necessity for IBD home, value based health care and treat to target strategies. Inflamm Bowel Dis. 2018;24(7):146 1461.
Riaz MS, Atreja A. Personalized technologies in chronic GI disorders: self-monitoring and remote sensor technologies. Clin Gastroenterol Hepatol. 2016;16:S1542 3565.
McInnes DK, Li AE, Hogan TP. Opportunities for engaging low income, vulnerable populations in health care: a systematic review of homeless persons’ access to and use of information technologies. Am J Public Health. 2013;103(Suppl 2):e11 24.
Quinn CC, Shardell MD, Terrin ML. Cluster randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934–42.
Nakamura N, Koga T, Iseki H. A meta-analysis of remote patient monitoring for chronic heart failure patients. J. Telemed Telecare. 2014;20:11.
McLean S, Nurmatov U, Liu JL. Telehealthcare for chronic obstructive pulmonary disease: Cochrane review and meta-analysis. Br J Gen Pract. 2012;62:e739.
Atreja A, Otobo E, Ramireddy K, Deorocki A. Remote patient monitoring in IBD: current state and future directions. Current gastroenterology reports. 2018;20(2):6.
Ganeshan R, et al. “Remote monitoring of implantable cardiac devices: current state and future directions.” Current Neurology and Neuroscience Reports., U.S. National Library of Medicine, Jan. 2018, www.ncbi.nlm.nih.gov/pubmed/29059076.
AliveCor. n.d.. Retrieved from https://www.alivecor.com/press/press_release/fda-designates-alivecors-bloodless-hyperkalemia-test-a-breakthrough-device/.
Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837–47 [PMC free article] [PubMed].
Krijthe BP, Kunst A, Benjamin EJ, et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur Heart J. 2013;34:2746–51 [PMC free article] [PubMed].
Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25 [PubMed].
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J Am Coll Cardiol. 2014;64(21):2246–80.
Engel G, Mead RH. “Remote monitoring for atrial fibrillation.” Current Neurology and Neuroscience Reports., U.S. National Library of Medicine. 2008. www.ncbi.nlm.nih.gov/pubmed/19891291.
Cantillon DJ. Off-site cardiac telemetry monitoring in non–critically ill patients. JAMA, American Medical Association. 2016; jamanetwork.com/journals/jama/fullarticle/2540401?linkid=27216896.
Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Heart Failure. 2014;1:4–25. https://doi.org/10.1002/ehf2.12005.
Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update: A report from the American Heart Association. Circulation. 2016;133:e38–e360. https://doi.org/10.1161/CIR.0000000000000350.
Barr DA. Geography as disparity: the shifting burden of heart disease. Circulation. 2016;133:1151–4.
Mozaffarian D, Anker SD, Anand I, et al. Prediction of mode of death in heart failure: the Seattle heart failure model. Circulation. 2007;116(4):392–8.
Adamson PB, Smith AL, Abraham WT, Kleckner KJ, Stadler RW, Shih A, et al. InSync III Model 8042 and Attain OTW Lead Model 4193 Clinical Trial Investigators. Continuous autonomic assessment in patients with symptomatic heart failure: prognostic value of heart rate variability measured by an implanted cardiac resynchronization device. Circulation. 2004;110:2389–94.
Conraads VM, Spruit MA, Braunschweig F, Cowie MR, Tavazzi L, Borggrefe M, et al. Physical activity measured with implanted devices predicts patient outcome in chronic heart failure. Circ Heart Fail. 2014;7:279–87.
Abraham WT, Compton S, Haas G, Foreman B, Canby RC, Fishel R, et al. Intrathoracic impedance vs daily weight monitoring for predicting worsening heart failure events: results of the Fluid Accumulation Status Trial (FAST). Congest Heart Fail. 2011;17:51–5.
Wang L. Fundamentals of intrathoracic impedance monitoring in heart failure. Am J Cardiol. 2007;99:3G–10G.
Abraham, W. T., Adamson, P. B., Bourge, R. C., Aaron, M. F., Costanzo, M. R., Stevenson, L. W., ... CHAMPION Trial Study Group. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. 2011. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21315441.
Rahimi K, Velardo C, Triantafyllidis A, Conrad N, Shah S, Chantler T, Mohseni H, Stoppani E, Moore F, Paton C, Emdin C, Ernst J, Tarassenko L on behalf of the SUPPORT-HF Investigators. A user-centred home monitoring and self-management system for patients with heart failure: a multicentre cohort study. Eur Heart J Qual Care Clin Outcomes 2015;1:66–71.
Mayo Clinic bloodless blood test submitted for FDA approval. 2018. Retrieved from https://ai-med.io/mayo-clinic-bloodless-blood-test-submitted-fda-approval/.
“Using Apple Watch for Arrhythmia Detection December 2018,” p. 11, 2018.
“Apple Heart Study: Assessment of Wristwatch-Based Photoplethysmography to Identify Cardiac Arrhythmias - Full Text View - ClinicalTrials.gov.” [Online]. Available: https://clinicaltrials.gov/ct2/show/NCT03335800. Accessed: 25-Jun-2019.
Turakhia MP, et al. Rationale and design of a large-scale, app-based study to identify cardiac arrhythmias using a smartwatch: The Apple Heart Study. Am. Heart J. Jan. 2019;207:66–75.
“US FDA Notification https://www.accessdata.fda.gov/cdrh_docs/pdf18/den180044.pdf.”
Chronic-care-management. 2019. Retrieved from https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/chronic-care-management.html
Chronic Care Management (CCM). 2019. Retrieved from https://www.aafp.org/practice-management/payment/coding/medicare-coordination-services/chronic-care.html
Maddox KE. What can we learn from voluntary bundled payment programs? JAMA Cardiol. 2018;3(8):766. https://doi.org/10.1001/jamacardio.2018.1734.
Cronin EM, Varma N. Remote monitoring of cardiovascular implanted electronic devices: a paradigm shift for the 21st century. Expert Rev Med Devices. 2012;9(4):367–76.
Olen MM, Dechert-Crooks B. Implantable cardiac devices: the utility of remote monitoring in a paediatric and CHD population. Cardiol Young. 2017;27(S1):S143–6.
Venkatesh T, Xu. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q. 2012;36(1):157.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ashish Atreja, Sandesh Francis, and Sravya Kurra each declare no potential conflicts of interest.
Rajesh Kabra has licensed technologies from Icahn School of Medicine at Mount Sinai to Rx. Health Digital Therapeutics Prescribing Platform. Dr. Kabra is the section editor of the Arrhythmia section of Current Treatment Options in Cardiovascular Medicine.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Arrhythmia
Rights and permissions
About this article
Cite this article
Atreja, A., Francis, S., Kurra, S. et al. Digital Medicine and Evolution of Remote Patient Monitoring in Cardiac Electrophysiology: A State-of-the-Art Perspective. Curr Treat Options Cardio Med 21, 92 (2019). https://doi.org/10.1007/s11936-019-0787-3
Published:
DOI: https://doi.org/10.1007/s11936-019-0787-3