Opinion statement
Rapid improvement in antineoplastic therapy is increasing not only cancer survivorship but also the incidence of end-stage heart failure among breast and childhood cancer survivors. Anthracyclines and newer targeted therapies, including trastuzumab and tyrosine kinase inhibitors, are important agents implemented in clinical practice that carry cardiotoxic risk. While acute heart failure is often self-limited and reversible, delayed-onset heart failure significantly reduces survival. Extremes of age, renal dysfunction, pre-existing coronary artery disease, HER2 positivity, and multi-drug therapy are predictors of irreversible heart failure after chemotherapy. Left ventricular assist device (LVAD) implantation and cardiac transplantation can be performed safely in patients with end-stage heart failure (HF) from chemotherapy. However, co-existing right ventricular dysfunction, hepatic congestion, and increased risk of bleeding make LVAD therapy challenging and dependent on careful patient selection. Cardiac transplantation in patients with chemotherapy-induced heart failure can be performed with good 10-year survival, but requires 5 years of cancer freedom and post-transplant infections remain a problem. Improvements in LVAD therapy and the expanding role of the total artificial heart and other durable biventricular support devices will likely provide more reliable surgical options for the management of end-stage HF after chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Options for the treatment of patients with end-stage heart failure (HF) have rapidly increased over the past decade and include automatic implantable defibrillators, chronic resynchronization therapy, left ventricular assist devices (LVAD), and orthotopic heart transplantation (OHT). Of these, the increased durability of LVADs has made the largest recent impact on survival of end-stage HF patients not amenable to or waiting for transplant [1].
Cancer survivors may develop end-stage HF due to chemotherapy-induced cardiomyopathy (CCMP) [2••, 3••, 4]. Although CCMP represents a small subset of the overall population of patients with end-stage HF, these patients have important differences in pathology, clinical characteristics, and demographics [3••].
This review will focus on the role of LVAD therapy and OHT in patients with end-stage HF secondary to cancer therapies.
Overview of cardio-toxicity
The problem
Improved treatment options have dramatically reduced cancer mortality [5]; in the USA alone, 1,340,400 deaths have been avoided over the past 5 years [6]. Unfortunately, a significant number of therapeutic agents responsible for this success are cardiotoxic. Anthracyclines (doxorubicin, epirubicin, and idarubicin), alkylating agents (cyclophosphamide, iphosphamide), monclonal antibodies against HER2/neu receptors, and tyrosine kinase inhibitors are known to cause left ventricular dysfunction and HF [7]. Apart from these well-studied agents, others such as proteasome inhibitors and anti-microtubule drugs (either alone or in combination) have also been implicated in left ventricular dysfunction [8••]. Breast and childhood cancer survivors have been found to be particularly prone to develop CCMP [9, 10]. Higher cumulative doses of anthracyclines and direct radiation to the chest are important predictors of HF after childhood hematologic cancer therapy and breast cancer [10]. Because these therapies remain the cornerstone of treatment for these types of malignancies, the problem of end-stage HF from CCMP is likely to continue to increase in the future.
Mechanisms
The most accepted mechanism of anthracycline-induced cardiotoxicity is via binding of topoisomerase 2-beta myocardial receptors releasing oxygen-free radicals that lead to progressive myocardial destruction [11]. Histopathologic examination of endomyocardial biopsies shows myofibrillar dropout, decreased cardiomyocyte density, and sarcoplasmic vacuolization [12]. While cardiotoxicity with HER2 antagonists has been reported to be mostly reversible [13], recent clinical studies have shown that patients treated with adriamycin and sequential trastuzumab may progress to permanent heart failure, thus emphasizing the potentiation effect of multiple cardiotoxic agents [14]. HER2 antagonists cause myocardial dysfunction by inhibiting ErbB2 receptors, which are essential for myocyte survival, making them resistant to apoptosis, growth, and hypertrophy [15]. Other studies have suggested that chemotherapeutic agents may deplete myocardial progenitor cells responsible for myocyte recovery [16, 17]. Radiation, usually given in conjunction or in sequence with chemotherapy, may also potentiate the cardiotoxic effects of chemotherapy by inducing an inflammatory myocarditis within the myocardial vascular bed, thus worsening ventricular dysfunction.
Clinical picture
Depending upon its onset, CCMP can be divided into (1) acute, (2) early, defined as within 1 year, and (3) late. Acute CCMP can occur in 11 % of patients after or during cancer therapy [18] presenting as arrhythmias, dyspnea on exertion, and fatigue, and is associated with recovery of left ventricular function in as many as 55 % of patients [19••]. Young age, small left atrial volume index, and lower B-natriuretic peptide have been shown to predict recovery in these patients [19••]. In contradistinction, late-onset CCMP (mostly associated with previous anthracycline therapy) progresses to end-stage HF in an irreversible way. Doxorubicin dose >550 mg/m2, bolus administration, male gender, age more than 65 years or less than 4 years, obesity, pre-existing renal dysfunction, and concurrent bleomycin therapy are all predictors of late-onset HF [20]. More recently, a positive HER-2 oncogene, type II diabetes, and coronary artery disease are additional important factors for progression of HF. While prognosis is poor for patients who develop CCMP, only 2.1 % undergoing anthracycline therapy will eventually have end-stage HF [21] [18].
Trastuzumab therapy for breast cancer leads to an absolute 14 % increase in HF over a 3-year period [21]. When both trastuzumab and anthracyclines are combined, almost one third of elderly patients will develop heart failure. Older age, pre-existing heart disease, and combination therapy are important predictors for end-stage HF [21].
Prevention and management
Recent studies have focused on pre-emptive measures and early treatment of cardiotoxicity to prevent progression to cardiomyopathy and heart failure. Echocardiographic techniques have been validated for early detection of cardiotoxicity. Strain imaging has been shown to precede reduction in left ventricular ejection fraction, and may be used as surrogate marker for cardiotoxicity [22].
Several studies have suggested the protective role of dexrazoxane, beta-blockers, statins, and ACE-inhibitors [23, 24]. Recent randomized controlled trial in 90 patients with malignant hemopathies showed that a combination of enalapril and carvedilol attenuated left ventricular systolic dysfunction [25]. As a result of these advances, many hospitals have started onco-cardiology surveillance programs to reduce the prevalence of cardiotoxicity in this patient group [23, 26].
Guideline-directed treatments for heart failure have not been fully validated in the CCMP population. Interestingly, in the INTERMACS database, patients with CCMP were more likely to receive ACE-inhibitors than patients with ischemic and non-ischemic cardiomyopathies (68 vs. 53 % (p = 0.02) and 51 % (p = 0.01)), while the use of beta-blockers was similar [3••].
Small case series of cardiac resynchronization therapies (CRT) and implantable cardiac defibrillators (ICDs) in CCMP have been reported [4]. In the largest study to date, Rickard et al. compared 18 patients with CCMP who received CRT and compared them to 189 patients with non-ischemic cardiomyopathy. CCMP group showed significant improvement in LV ejection fraction, LV diameters, and functional class, similar to other non-ischemic patients [27].
Advanced therapies
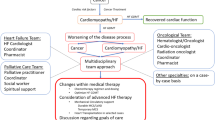
Mechanical circulatory support and OHT provide reliable options and improve long-term survival in patients with end-stage heart failure. We now present an overview of the present status of these therapies in the care of patients with CCMP.
Left ventricular assist device therapy
LVAD implant is now well established as a reliable medium-term option for end-stage HF [28]. The number of LVAD implants have increased exponentially since the approval of LVAD therapy as destination therapy, i.e., for patients ineligible for heart transplantation [29]. The INTERMACS (Inter-Agency Registry of Mechanical Circulatory Support) is a national database of patients undergoing mechanical circulatory support in the USA. They recently reported that almost half of LVADs are now implanted as “destination therapy” [30••]. The transition from pulsatile to continuous-flow devices has significantly increased 1-year survival from 66 to 81 % [30••]. Four-year survival is now estimated at 47 % in all patients implanted with a continuous-flow device during 2008–2013 [30••].
Demographics characteristics of CCMP patients receiving LVADs
Between 2006 and 2011, there were 75 patients with CCMP who received durable LVADs registered in INTERMACS database [3••]. This report has demonstrated important demographic and clinical differences between patients with CCMP, ischemic, and non-ischemic cardiomyopathies who received mechanical circulatory support devices. CCMP patients (mean age of 53 years) are typically much younger than those with ICMP (60 years; p < 0.001) at the time of LVAD implant. The CCMP cohort is predominantly made up of females (72 %) while both NICMP (76 %; p < 0.0001) and ICMP (87 %; p < 0.0001) are predominantly males. CCMP patients were also less likely to be white than ICMP patients (64 vs. 80 %, p = 0.0006).
Patients with CCMP had lower BMIs than both NICMP and ICMP (26.0 vs. 28.9 [p < 0.0001] vs. 28.0 [p = 0.0019]) and were overall healthier, with less diabetes than ICMP (25 % vs. 46 %, p = 0.0004), less smoking than NICMP and ICMP (1 % vs. 12 % [p = 0.01] vs. 15 % [p = 0.0016]), and less likely to have history of alcohol abuse (5 % vs. 16 % [p = 0.01], vs. 18 % [p = 0.01]) or coronary artery disease (0 % vs. 16 % [p < 0.0001], vs. 100 [p < 0.0001]). However there was no difference in NYHA class or INTERMACS profile between the groups. Taken together, it seems that patients with advanced CCMP are mostly young females without other comorbid conditions.
Other differences were that the CCMP group was more likely to receive ACE inhibitors (68 %) than NICMP (53 %, p = 0.02) and ICMP (51, p = 0.01), less ICD use than NICMP and ICMP (66 vs. 77 vs. 77 %, p = 0.03). However, there were no differences in preimplantation use of inotropes, intraaortic balloon pump, or ventilatory support. Significantly more CCMP patients were implanted as destination therapy (33 %) than NICMP (14 %, p < 0.0001) and ICMP (23 %, p = 0.03).
Right ventricular dysfunction
Right ventricular (RV) biopsy has long been utilized in the diagnosis of cardiotoxicity [31], thus demonstrating the involvement of the RV in CCMP. This was demonstrated to have clinical implications in patients receiving isolated left ventricular mechanical support in the INTERMACS series. Pre-operative assessments of surrogate markers of RV function, such as alanine and aspartate amiontransferases, were twice to three times higher in CCMP group than ICMP and NICMP, possibly suggesting more severe congestive hepatopathy. In addition, pulmonary systolic pressure was significantly lower in CCMP (43.9 mmHg) than in NICMP (49.4, p = 0.0015) and ICMP (51.2, p < 0.0001), which may reflect the inadequacy of RV to mount higher systolic pulmonary pressures. Moderate to severe tricuspid regurgitation was more common in CCMP (62 %) than NICMP (43 %, p = 0.0037) and ICMP (49 %, p = 0.04) suggesting worse RV dilatation. Central venous pressure to pulmonary capillary pressure, a marker of RV dysfunction, was significantly higher in CCMP (0.68) than NICMP (0.54, p < 0.0001) and ICMP (0.51, p < 0.0001).
Given these preoperative findings, it is not surprising that right ventricular failure was much more frequent among CCMP patients treated with LVADs than among those with other cardiomyopathies. In fact, almost one fifth of CCMP patients needed subsequent or concomitant right ventricular assist device (RVAD) support, in contrast to NICMP and ICMP (19 vs. 11 vs. 6 %, p = 0.006) (Fig. 1). Post-LVAD RV failure was associated with significantly poorer outcomes as 33 % of patients with RVADs died in the early post-operative period.
This pattern of right ventricular failure in CCMP was also reported in patients bridged to transplantation with MCSDs. In the ISHLT cardiac transplantation registry (2000–2008), 19.6 % of CCMP patients were bridged with LVADs and 5.6 % were bridged with RVADs [2••]. While LVAD utilization was similar to other non-ischemic cardiomyopathies, RVAD was more than twice as common in patients with CCMP (5.6 vs. 2.3 %, p = 0.002).
Outcomes and survival
Patients with CCMP had more concomitant surgery (tricuspid repair, RVAD implant, atrial septal defect closure or others) compared with NICMP and ICMP (48 vs. 36 % [p = 0.03] and 36 % [0.04]) and had more failure to wean from cardiopulmonary bypass (5 vs. 1 % [p = 0.01] vs. 2 % [p = 0.04]), which may represent higher rate of RV failure.
Patients with CCMP had an increased risk of bleeding at 36-month follow-up (p = 0.0001), but there were no differences in rate of neurological events, device malfunction, infection, or RV failure events (Fig. 2).
Patients with CCMP had 1-, 2-, and 3- year survival of 73, 63, and 47 %, respectively. There were no differences in survival between bridge to transplantation (BTT) and destination therapy (DT) groups. Patients with BiVAD support had higher mortality than LVAD alone (p = 0.0007). CCMP patients had similar overall survival to ICMP and NICMP (Fig. 3).
Myocardial recovery
Anecdotal reports of left ventricular recovery in cancer survivors after LVAD implant are reported sporadically [18, 32, 33]. The INTERMACS database demonstrated only 1 % recovery among CCMP patients implanted during 2006–2012 [3••]. Various factors promoting recovery could be young age [18] [34], absence of significant myocyte dropout [18], or early-onset HF [32]. While our experience with LVAD therapy in this cohort is at present limited, progressive advances in LVAD design and reliability will promote more CCMP patients to opt for mechanical circulatory support.
Total artificial heart
With the bi-ventricular involvement typical in CCMP, the total artificial heart (TAH) could be an attractive option for these patients. As of 2013, 239 TAHs have been implanted in the USA during a 6-year period [30••, 35]. At present, TAH can be implanted only as a bridge to transplant, with patients needing five cancer-free years prior to listing for cardiac transplantation. However, the Food and Drug Administration has recently approved the TAH for destination therapy [36]. While the TAH does have issues related to anti-coagulation and stroke, more than 47 patients have survived for more than 1 year on support. The new drivers allow patients to ambulate freely both within and out of the hospital. Only one case of TAH implanted in CCMP was reported in the literature [37]. In the ISHLT (International Society of Heart and Lung Transplantation) and INTERMACS registries, none of the patients with CCMP had TAH [2••].
Cardiac transplantation
Cardiac transplantation remains the “gold standard” and only long-term solution for the definitive treatment of end-stage HF [28], with an expected 1-year survival of 90 and a 70 % 5-year survival [38]. Given the concerns of increased risk of cancer recurrence and new cancers post-transplantation, patients are currently required to be cancer free for 5 years before consideration for heart transplantation.
Historical overview
Isolated reports of transplantation in cancer survivors with end-stage HF have appeared in medical literature since 1987 [39–42]. Recent reports have challenged the 5-year rule and have demonstrated good survival if patients are transplanted earlier [43]. As a result of reassuring data, the number of heart transplantations for CCMP has tripled from 1987 to 2011 (Fig. 4). As of 2011, 453 patients with CCMP had received heart transplantations in the USA [44]. Recently, two large database reviews have provided more insight regarding this surgical strategy in CCMP patients [2••, 44].
Demographics and clinical characteristics
The International Society of Heart and Lung transplantation (ISHLT), a voluntary self-reported database identified 232 patients with CCMP undergoing transplant during 2000–2008 and compared their characteristics with 8890 patients with NICMP [2••]. Most common pre-transplant malignancies were leukemia and lymphomas (41.5 %), breast (38.9 %), and sarcomas (9.3 %).
Compared with NICMP, patients with CCMP were younger (mean 49.4 years vs. 45.5, p = 0.002), more likely to be females (24.8 vs. 63.8 %, p < 0.001), and had lower BMI (26.0 vs. 24.6, p < 0.001), less likely to have diabetes (18.1 vs. 12.8 %, p = 0.045) and hypertension (35.4 vs. 28.4 %, p = 0.039). This pattern is similar to that seen in patients implanted with LVADs discussed earlier. There were no differences in LVAD use, intraaortic balloon pump, extracoroporeal membrane oxygenation, or ventilator support between the groups. However, RVAD support was more common in CCMP than in NICMP (5.6 vs. 2.3 %, p = 0.002).
In another review of United Network for Organ Sharing (UNOS) database of all heart transplantation in the USA from 1987 to 2011 [44], 453 patients with CCMP were compared to 51,312 patients without CCMP (ischemic and non-ischemic cardiomyopathies). In addition to the differences reported in the ISHLT registry, this study showed that patients with CCMP were more likely to use pre-transplantation intravenous inotropic support (48 vs. 39 %, p < 0.001) and were more likely to be hospitalized in the intensive care unit (17 vs. 14 %, p = 0.012).
Outcomes and survival
The outcomes of CCMP patients treated with heart transplantations are overall favorable and comparable to that of other groups. Interestingly, 1 -year freedom from rejection was higher in CCMP than in NICMP patients (72 vs. 62 %, p = 0.03), likely representing an attenuated immune system in patients with CCMP as a result of chemotherapy-related toxicity. Another major finding was that the incidence of cancer recurrence was not significant among CCMP patients, dissipating a longstanding fear. Although the cumulative 1-year incidence of post-transplantation malignancy was higher in CCMP (5 vs. 2 %, p = 0.006), this was mainly due to non-melanoma skin cancer.
Survival at 1, 3, and 5 years was 86, 79, and 71 % for transplanted patients with CCMp. There was no significant difference in the survival between CCMP and NICMP (p = 0.19) (Fig. 5). The most common cause of death among CCMP group was graft failure (30 %), followed by allograft vasculopathy (20 %) and malignancy (15 %), similar to other HF etiologies. These results were further supported by findings from the UNOS database where survival was similar between CCMP and all other cardiomyopathies (p = 0.19) (52). Taken together, data from two large databases have confirmed the safety and excellent outcomes of orthotopic heart transplantation in patients with CCMP.
Future direction
More patients with chemotherapy-induced end-stage heart failure are being considered for surgical treatment as a result of accumulating favorable data. Cardiac transplantation is still the gold standard for patients with end-stage heart failure. However, sometimes, we are unable provide this therapy to patients in a timely manner. In these circumstances, LVAD and TAH therapy may be reliable solutions for cancer survivors with end-stage heart failure.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345(20):1435–43.
Oliveira GH, Hardaway BW, Kucheryavaya AY, Stehlik J, Edwards LB, Taylor DO. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. J Heart Lung Transplant : Off Pub Int Soc Heart Transplant. 2012;31(8):805–10. This article presents retrospective analysis of a prospective large database outlining the results of heart transplantation in patients with chemotherapy induced heart failure.
Oliveira GH, Dupont M, Naftel D, Myers SL, Yuan Y, Tang WH, et al. Increased need for right ventricular support in patients with chemotherapy-induced cardiomyopathy undergoing mechanical circulatory support: outcomes from the intermacs registry (interagency registry for mechanically assisted circulatory support). J Am Coll Cardiol. 2014;63(3):240–8. This is a retrospective review of the INTERMACS database, a prospectively collected national registry of patients undergoing mechanical circulatory support surgery in the USA. The article looks at pre-operative differences, early results, and late survival in CCMP patients undergoing LVAD implant.
Oliveira GH, Qattan MY, Al-Kindi S, Park SJ. Advanced heart failure therapies for patients with chemotherapy-induced cardiomyopathy. Circ Heart fail. 2014;7(6):1050–8.
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA: Cancer J Clin. 2010;60(5):277–300.
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA: Cancer J Clin. 2014;64(1):9–29.
Yeh ET, Tong AT, Lenihan DJ, Yusuf SW, Swafford J, Champion C, et al. Cardiovascular complications of cancer therapy: diagnosis, pathogenesis, and management. Circulation. 2004;109(25):3122–31.
Yu AF, Steingart RM, Fuster V: Cardiomyopathy associated with cancer therapy. Journal of cardiac failure (2014). This review presents the mechanism and etio-pathogenesis of heart failure in chemotherapy patients.
Ezaz G, Long JB, Gross CP, Chen J. Risk prediction model for heart failure and cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Heart Assoc. 2014;3(1):e000472.
Chow EJ, Chen Y, Kremer LC, Breslow NE, Hudson MM, Armstrong GT, Border WL, Feijen EA, Green DM, Meacham LR, Meeske KA et al.: Individual prediction of heart failure among childhood cancer survivors. Journal of clinical oncology : official journal of the American Society of Clinical Oncology (2014).
Zhang S, Liu X, Bawa-Khalfe T, Lu LS, Lyu YL, Liu LF, et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med. 2012;18(11):1639–42.
Cooper Jr LT. Role of left ventricular biopsy in the management of heart disease. Circulation. 2013;128(14):1492–4.
Ewer MS, Vooletich MT, Durand JB, Woods ML, Davis JR, Valero V, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol : Off J Am Soc Clin Oncol. 2005;23(31):7820–6.
Telli ML, Hunt SA, Carlson RW, Guardino AE. Trastuzumab-related cardiotoxicity: calling into question the concept of reversibility. J Clin Oncol. 2007;25(23):3525–33.
Hervent AS, De Keulenaer GW. Molecular mechanisms of cardiotoxicity induced by erbb receptor inhibitor cancer therapeutics. Int J Mol Sci. 2012;13(10):12268–86.
Meinardi MT, van der Graaf WT, van Veldhuisen DJ, Gietema JA, de Vries EG, Sleijfer DT. Detection of anthracycline-induced cardiotoxicity. Cancer Treat Rev. 1999;25(4):237–47.
Shan K, Lincoff AM, Young JB. Anthracycline-induced cardiotoxicity. Ann Intern Med. 1996;125(1):47–58.
Khan N, Husain SA, Husain SI, Khalaf N, George J, Raissi F, et al. Remission of chronic anthracycline-induced heart failure with support from a continuous-flow left ventricular assist device. Texas Heart Inst J / Texas Heart Inst St Luke’s Episcopal Hosp, Texas Child Hosp. 2012;39(4):554–6.
Oliveira GH, Mukerji S, Hernandez AV, Qattan MY, Banchs J, Durand JB, et al. Incidence, predictors, and impact on survival of left ventricular systolic dysfunction and recovery in advanced cancer patients. Am J Cardiol. 2014;113(11):1893–8. This is a retrospective chart review of patients from a tertiary-level cancer center. The article presents data on patients who developed left ventricular dysfunction while on chemotherapy.
Praga C, Beretta G, Vigo PL, Lenaz GR, Pollini C, Bonadonna G, et al. Adriamycin cardiotoxicity: a survey of 1273 patients. Cancer Treat Rep. 1979;63(5):827–34.
Chen J, Long JB, Hurria A, Owusu C, Steingart RM, Gross CP. Incidence of heart failure or cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Coll Cardiol. 2012;60(24):2504–12.
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH: Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy—a systematic review. Journal of the American College of Cardiology (2014)
Al-Kindi S, Younes A, Qattan M, Oliveira G. Preemptive cardioprotective strategies in patients receiving chemotherapy. Curr Cardiovasc Risk Rep. 2014;8(11):1–14.
Kalam K, Marwick TH. Role of cardioprotective therapy for prevention of cardiotoxicity with chemotherapy: a systematic review and meta-analysis. Eur J Cancer. 2013;49(13):2900–9.
Bosch X, Rovira M, Sitges M, Domenech A, Ortiz-Perez JT, de Caralt TM, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the overcome trial (prevention of left ventricular dysfunction with enalapril and carvedilol in patients submitted to intensive chemotherapy for the treatment of malignant hemopathies). J Am Coll Cardiol. 2013;61(23):2355–62.
Yeh ET. Onco-cardiology: the time has come. Texas Heart Inst J / Texas Heart Inst St Luke’s Episcopal Hosp Texas Child Hosp. 2011;38(3):246–7.
Rickard J, Kumbhani DJ, Baranowski B, Martin DO, Tang WH, Wilkoff BL. Usefulness of cardiac resynchronization therapy in patients with adriamycin-induced cardiomyopathy. Am J Cardiol. 2010;105(4):522–6.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2013;128(16):e240–327.
Stewart GC, Stevenson LW. Keeping left ventricular assist device acceleration on track. Circulation. 2011;123(14):1559–68.
Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED, et al. Sixth intermacs annual report: a 10,000-patient database. J Heart Lung Transplant : Off Pub Int Soc Heart Transplant. 2014;33(6):555–64. This study reports the overall results of LVAD and TAH implant in the United States.
Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation. 2007;116(19):2216–33.
Kurihara C, Nishimura T, Nawata K, Kinoshita O, Hisagi M, Motomura N, et al. Successful bridge to recovery with vad implantation for anthracycline-induced cardiomyopathy. J Artif Organs : Off J Jpn Soc Artif Organs. 2011;14(3):249–52.
Freilich M, Stub D, Esmore D, Negri J, Salamonsen R, Bergin P, et al. Recovery from anthracycline cardiomyopathy after long-term support with a continuous flow left ventricular assist device. J Heart Lung Transplant : Off Pub Int Soc Heart Transplant. 2009;28(1):101–3.
Cavigelli-Brunner A, Schweiger M, Knirsch W, Stiasny B, Klingel K, Kretschmar O, et al. Vad as bridge to recovery in anthracycline-induced cardiomyopathy and hhv6 myocarditis. Pediatrics. 2014;134(3):e894–9.
Copeland JG. Syncardia total artificial heart: update and future. Texas Heart Inst J / Texas Heart Inst St Luke’s Episcopal Hosp Texas Child Hosp. 2013;40(5):587–8.
Hayashi T, Inagaki H, Kimura S, Higuchi K, Kawabata M, Haraguchi G, Hachiya H, Hirao K, Isobe M: A case of adriamycin-induced cardiomyopathy implanted artificial heart after having the uncontrollable arrhythmia. Journal of cardiac failure 16(9):S147
Alraies MC, Eckman P. Adult heart transplant: indications and outcomes. J Thorac Dis. 2014;6(8):1120–8.
Arico M, Nespoli L, Pedroni E, Bonetti F, Vigano M, Burgio GR. Heart transplantation in a child with doxorubicin-induced cardiomyopathy. N Engl J Med. 1988;319(20):1353.
Arico M, Pedroni E, Nespoli L, Vigano M, Porta F, Burgio GR. Long term survival after heart transplantation for doxorubicin induced cardiomyopathy. Arch Dis Child. 1991;66(8):985–6.
Goenen M, Baele P, Lintermans J, Lecomte C, Col J, Ponlot R, et al. Orthotopic heart transplantation eleven years after left pneumonectomy. J Heart Transplant. 1988;7(4):309–11.
Grady KL, Jassak PF, Varricchio CG. Cardiac transplantation for doxorubicin cardiotoxicity. Prog Cardiovasc Nurs. 1987;2(2):66–70.
Ward KM, Binns H, Chin C, Webber SA, Canter CE, Pahl E. Pediatric heart transplantation for anthracycline cardiomyopathy: cancer recurrence is rare. J Heart Lung Transplant : Off Pub Int Soc Heart Transplant. 2004;23(9):1040–5.
Lenneman AJ, Wang L, Wigger M, Frangoul H, Harrell FE, Silverstein C, et al. Heart transplant survival outcomes for adriamycin-dilated cardiomyopathy. Am J Cardiol. 2013;111(4):609–12.
Compliance with Ethics Guidelines
Conflict of Interest
Salil V. Deo, Sadeer G. Al-Kindi, and Guilherme H. Oliveira each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardio-oncology
Rights and permissions
About this article
Cite this article
Deo, S.V., Al-Kindi, S.G. & Oliveira, G.H. Management of Advanced Heart Failure due to Cancer Therapy: the Present Role of Mechanical Circulatory Support and Cardiac Transplantation. Curr Treat Options Cardio Med 17, 28 (2015). https://doi.org/10.1007/s11936-015-0388-8
Published:
DOI: https://doi.org/10.1007/s11936-015-0388-8