Abstract
Purpose of Review
Renal masses in the kidney graft pose an important clinical dilemma, balancing graft function against the need for cancer control.
Recent Findings
Donor origin cancers in the renal graft can be classified as ‘donor transmitted’ or ‘donor derived’. The landmark TracerX Renal changed our understanding of renal cell carcinoma oncogenesis, demonstrating that key mutations in childhood lead to clinically apparent tumours in later life. Identified pre-operatively, contemporary evidence suggests that masses excised prior to transplantation result in acceptable oncologic safety and graft function. Identified post-operatively management mirrors that for a mass in a solitary kidney in the non-transplant population, with focus on a nephron-sparing approach.
Summary
With growing number of kidney transplants each year, ageing donors, and increasing graft survival, masses in the renal graft are likely to become a more prevalent clinical conundrum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last 10 years, a trend toward organ donation in the UK has seen a 64% increase in the number of kidneys transplanted from deceased donors [1]. With this trend, the demographic of organ donors has also shifted. In the past decade, the proportion of donors over the age of 60 years increased from 20 to 36%, while the proportion of those over 70 years has similarly increased from 5 to 14% [1]. Older donors are at increased risk of occult malignancy and therefore represent an increased risk of cancer transmission to organ recipients.
The most recent data from the UK Transplant Registry suggests a 0.06% risk of transmission of donor origin cancer (DOC) with renal transplantation [2]. DOC can be defined as donor-transmitted cancer (DTC) when a malignancy is transmitted at the time of transplantation (0.05% risk) or donor-derived cancer (DDC) when de novo tumours develop from donor tissue (0.01% risk). This recently reported DOC was higher than the 0.017% in the previous decade [3], which may partly be due to improved reporting but may also reflect the rising age of the donor population and increasing graft survival. Along with higher absolute numbers of renal transplants taking place, urologists and transplant surgeons are likely to face a growing number of patients presenting with the complex clinical scenario of a mass in the kidney allograft.
Identification of Renal Graft Masses
The opportunity to identify masses within the transplant graft presents itself at different points in the patient pathway of renal transplantation. Living donors undergo rigorous work-up to assess suitability for donation including imaging of the renal vascular anatomy and assessment of the renal parenchyma [4].
For deceased donors, pre-morbid imaging is not routinely performed, except in France where all donors undergo ultrasound or CT screening for renal masses [5, 6]. Therefore, in most nations, the opportunity to identify renal masses prior to transplantation is limited to organ retrieval and during back bench preparation of the organ, when small endophytic masses may not be readily apparent. Post-transplant, time-zero or surveillance biopsy may reveal unexpected histology. Close postoperative follow-up and low threshold for ultrasound imaging of the renal graft [7, 8] offer further opportunity for incidental detection of renal masses. Alternatively, recipients may develop symptoms of haematuria, pain, or constitutional symptoms triggering investigation for suspected renal malignancy. There is a lack of strong evidence for the use of routine radiological cancer screening in the renal graft, resulting in conflicting guidelines by national and international societies of nephrology and transplantation (Table 1).
The UK Advisory Committee on the Safety of Blood, Tissues and Organs (SaBTO), and the US Disease Transmission Advisory Committee (DTAC) acknowledge that limitations in deceased donor assessment mean that the risk of donor-transmitted cancer can be minimised but not abolished [15, 16].
Identification Pre-transplant
A mass identified in the potential renal graft prior to implantation is not necessarily a contraindication to its utilisation. Careful investigation to determine the aetiology of the mass coupled with careful donor and recipient counselling is critical in deciding its suitability for subsequent implantation.
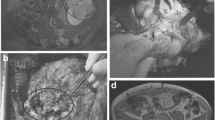
In an effort to address the shortage of organs available for transplantation, a number of institutions actively sought out nephrectomy specimens performed for the management of small renal masses (SRMs). Instead of discarding the otherwise well-functioning kidney surrounding the SRM, it was ‘restored’ by performing ex vivo partial nephrectomy and renorrhaphy for subsequent transplantation in carefully selected and counselled recipients [17,18,19]. A systematic review of 109 such cases from 19 studies [20•] demonstrated only one with suspected local recurrent disease 9 years following transplantation, managed successfully with active surveillance [17, 21]. However, the recent move to partial nephrectomy over radical nephrectomy as the standard of care for T1 renal tumours [22] means that fewer such nephrectomy specimens are likely to be available for restoration.
The Organ Procurement and Transplantation Network/United Network for Organ Sharing (OPTN/UNOS) have published advice on the utilisation of organs for transplantation from donors with malignant disease [16]. Expert opinion consensus generated clinical risk strata for small renal masses, suggesting they portend a minimal (< 0.1%), low (0.1–1%), intermediate (1–10%), or high risk (> 10%) of transmission, for completely resected Fuhrman grade 1–2 tumours of < 1-cm, 1–2.5-cm, 4–7-cm, and > 7-cm diameter respectively [16]. This suggests that carefully selected SRMs can be excised and the kidney safely offered for transplantation.
In the setting of a mass in a deceased donor kidney, adequate assessment to ascertain its nature must be performed while attempting to maintain an acceptable cold ischaemic time. In this setting, appropriate histology should be available to determine tumour grade and confirm clear resection margins prior to implantation [20•] to ascertain the transmission risk. High grade (> Fuhrman grade 2) tumours would be deemed intermediate or high risk for recurrence and therefore less suitable for transplantation. In our centre, good working relationships with pathology colleagues allow rapid paraffin section reporting and a chance for these organs to be safely utilised in carefully selected patients with appropriate counselling. Furthermore, transplantation centres managing other organs from the index donor must be notified at the earliest opportunity.
Current guidelines from the British Transplantation Society state that all living donors with renal masses identified on work-up should be referred to a urologist for further evaluation and offered the standard of care [4].
In the context of sufficient renal function, potential donors wishing to consider radical nephrectomy, ex vivo excision of a small renal mass with subsequent donation of the reconstructed kidney can be considered with support of the multidisciplinary team and appropriate informed consent from the donor and recipient [4].
Identification Post-transplant
In the event of identification of a renal mass in the post-transplant period, we advocate investigation and management to largely reflect that of a renal mass in a solitary kidney in the non-transplant population. Additional factors to consider in this patient group are immunosuppression therapy and the implication for other organs from the index donor.
Guidelines from both the European Association of Urologists and the American Urological Association recommend radiological work-up of any renal mass with cross-sectional, multiphasic contrast-enhanced imaging with CT or MRI [22, 23]. Depending on the time interval between transplantation and detection of the renal mass, thoracic imaging should be considered to assess for evidence of metastatic spread, while bone and brain imaging reserved for cases with clinical suspicion of disease at these sites.
A cross-sectional study of registry data from all transplant recipients in the UK between January 2001 and December 2010 demonstrated that from 21,029 renal transplants, there were 12 cases of donor-transmitted cancer identified in the kidney in the post-operative period [2]. Nine of these were incidental findings on biopsy performed routinely or to investigate graft dysfunction, two were identified on biopsy after lymphoma was discovered at post mortem of the donor, and one on biopsy performed after small cell lung cancer was diagnosed in the paired kidney. The study did not report on the radiological assessment of these cases.
In any identified cases of donor-transmitted cancer, all other organs from the index donor must be identified and the recipients undergo investigation to exclude transmission of malignancy. In the case of a short time interval between tumour implantation and discovery of donor-transmitted malignancy from other organs, explantation of the graft can be considered both to treat the primary lesion and to allow cessation of immunosuppression and initiation of systemic treatment, as required.
Pathology
The nature of masses diagnosed in the renal graft and reported in the literature is extremely varied, as outlined in Table 2. Here we focus on those most relevant to the transplant surgeon and urologist.
Angiomyolipoma
Distinctive on cross-sectional imaging for having the same attenuation as fat, an angiomyolipoma (AML) is a benign neoplasm made up of mature adipose tissue and smooth muscle cells, which strongly expresses oestrogen receptor β. Classic studies on the natural history of AMLs [30, 31] suggest a cut off of 4 cm below which symptoms are uncommon, and can be managed expectantly with biennial ultrasound surveillance [32]. While ideally an AML would be excised prior to transplantation to mitigate the risk of growth and subsequent haemorrhage, BTS guidelines support small tumours < 1 cm in a difficult location being transplanted with annual ultrasound surveillance. Special care must be taken in women of childbearing potential, as a rise in oestrogen levels in pregnancy promote AML growth.
The mammalian target of rapamycin (mTOR) pathway is implicated in the development of AML when associated with tuberous sclerosis. Phase-2 trials assessing mTOR inhibitor sirolimus have demonstrated shrinkage of AMLs in this population [33, 34]. mTOR inhibitors also have a role in immunosuppression following renal transplantation. A case study reported successful shrinkage of an incidentally detected AML from 4 to 2.4 cm by switching mycophenolate mofetil to sirolimus outside the tuberous sclerosis setting [26].
Oncocytoma
Oncocytomas are the most common benign renal tumours. Often asymptomatic and incidental, they appear as a contrast-enhancing mass on CT making them impossible to distinguish from renal cell carcinoma (RCC) without histopathology. There is no evidence for a risk of malignant transformation. A case report of biopsy-confirmed oncocytoma in a renal allograft demonstrated stable radiological appearances over 5 years with annual MRI surveillance [28].
Renal Cell Carcinoma
It is known that solid organ recipients are at approximately two times the risk of developing any malignancy compared with the general population, suggesting that immunosuppression plays a role in its development [35]. Large national observational studies have demonstrated a several-fold risk of developing RCC in native kidneys following renal transplantation [35, 36]. Here we focus on RCC development in the renal graft.
Clear Cell
Clear cell RCC is the commonest histological subtype in the general population, accounting for 70–80% of cases [32]. In the renal transplant population, only 38–46% of RCCs arising in the kidney graft are clear cell RCC [6, 27••].
Papillary
Papillary renal cell carcinoma accounts for 42–55% of RCCs arising in the renal graft [6, 27••], compared with 10% in the general population [37]. While a higher incidence of papillary RCC in the native kidneys of patients with end-stage renal disease is well described [38, 39], there is little explanation in the literature for the predominance of this histological subtype in the renal allograft. To the best of our knowledge, there are no reports in the literature of the incidence of type 1 versus type 2 papillary RCC in the renal allograft.
As up to 40% of papillary RCCs are multifocal [32], such tumours arising in recipients of living donor transplants should prompt assessment in the living donor’s remaining kidney. Also consideration that the graft may develop further papillary neoplasms in future should be considered when planning treatment, with an emphasis on nephron-sparing approaches. In the case of a deceased donor, alerting the team managing the recipient of the contralateral kidney is mandatory.
RCC Unique to End-Stage Renal Disease
In 2006, Tickoo et al. described how 261 tumours examined from 66 native end-stage renal disease (ESRD) kidneys fell into two distinct groups: those that are also seen in the sporadic setting (clear cell, papillary, etc.) and those unique to ESRD that are difficult to classify into known RCC subtypes [39]. Of the tumours unique to ESRD, two histologic subgroups were identified, ‘acquired cystic disease-associated RCC’ and ‘clear-cell papillary RCC of the end-stage kidneys’.
It seems reasonable to consider that a failed renal graft may be susceptible to the same tumours seen in native kidneys of patients with ESRD. Tillou et al. reported on a multicentre cohort in which 3 of 79 de novo tumours developing in renal grafts demonstrated ‘mixed’ clear and papillary cell tumours [6]. These cases may have represented RCCs unique to ESRD, although graft function of these cases was not reported.
Donor-Derived Cancer (De Novo)
The landmark TracerX Renal study described the genetic evolution, nature and timing of oncogenic mutations in clear cell renal cell carcinoma [40••, 41••]. It demonstrated that key oncogenic events occurring in childhood and adolescence result in clinically apparent tumours several decades later [41••]. This would support the notion that clear cell tumours arising in a renal graft would be de novo tumours derived from susceptible donor cells, not clinically apparent at the time of transplantation. However, higher rates of renal cell carcinomas in the transplant population compared with the general population support the theory that events at the time of transplantation and immune suppression may promote further oncogenesis in donor renal cells.
The idea that donor-derived tumours arise in the allograft several years after transplantation is not new. Park et al. demonstrated with DNA analysis that a de novo RCC in the renal allograft arose from donor-derived cells 258 months after transplantation [42].
When assessing the renal transplant recipient therefore, it is important to consider not just the age of the patient but also the biological age of their transplant kidney. A 35-year-old patient receiving a kidney transplant from a deceased donor 20 years their senior, for example, would fall into the peak population incidence for development of RCC over the next 10 years. Donor risk factors for development of RCC, smoking status for example, should also be considered.
Management
While no guidelines for the investigation and management of renal graft masses currently exist, parallels can be drawn with the management of a mass in a solitary native kidney. Cancer control must be balanced against the preservation of renal function and avoidance of a return to dialysis. For malignant neoplasms, nephron-sparing strategies should be prioritised where there is a realistic prospect of disease control. For benign lesions, conservative management with surveillance is preferred. In a non-functioning renal graft, loss of function is not relevant. Additional factors to consider in the transplant population are suitability and availably of organs for future transplant, if required, and reduction of immunosuppression therapy, which is likely to improve cancer outcomes.
Renal Mass Biopsy
In the non-transplant population, renal mass biopsy is not mandated prior to treatment, except for ablative therapies or active surveillance [22, 23]. In the transplant population, renal biopsies provide important additional tumour information to help weigh up the risk-benefit profile of conservative versus invasive treatment options. In a French national series between 1988 and 2009, 30 out of 79 (38.0%) renal cell carcinomas identified in renal grafts underwent biopsy for histological diagnosis [6]. Over a similar time period in the USA, only 20.7% of patients with diagnosed with RCC in the non-transplant setting underwent biopsy prior to treatment [43].
Active Surveillance
Active surveillance is the management of choice for asymptomatic benign lesions, small solid masses < 2 cm, or for patients in whom the risk of complications from intervention outweigh the oncological benefit of active treatment [22, 23]. Recommended frequency of repeat imaging is every 3–6 months for the first year and annually thereafter [22, 23]. European guidelines recommend a biopsy prior to embarking on active surveillance [22].
Thermal Ablation
In the non-transplant setting, thermal ablation of small renal tumours < 3 cm in the form of cryotherapy or radiofrequency ablation is often reserved for frail or comorbid patients, due to its low associated morbidity but higher recurrence rates [22, 23]. In the transplant setting, preservation of renal function with these techniques has made it an attractive tool for the management of small renal masses in the renal graft. A multicentre national French cohort reported treatment of 48 renal graft masses of mean tumour size 2.1 cm with these methods and only a single recurrence that was treated with repeat ablation [44]. While ablative treatments are suitable for exophytic lesions, they should be avoided in masses at the hilum or near the collecting system.
Surgery: Radical Versus Nephron Sparing
Concerns about tumour progression in the setting of immunosuppression initially lead to radical transplant nephrectomy as the default surgical option for proven RCC in the renal graft and, with it, a return to dialysis. Favourable oncological outcomes of nephron-sparing surgery for renal graft tumours have been demonstrated with minimal impact on renal function [5, 45, 46]. In a systematic review of 163 patients with solid renal masses in the renal graft, 110 (67.5%) underwent partial nephrectomy [27••]. This mirrors a trend toward nephron-sparing surgery in the management for renal masses in the general population [22, 23].
Zero-ischaemic partial nephrectomy, by avoiding clamping of the transplant renal artery, has also been reported in an attempt to avoid an ischaemic insult on the renal graft intra-operatively. Reported estimated blood loss was 500 ml, and the patient did not require transfusion [44].
Immunosuppression
Systemic therapy for the management of renal cell cancer has rapidly evolved in the past decade, with an increased understanding of the molecular biology and pathophysiology of RCC. Mammalian target of rapamycin (mTOR) inhibitors have a role in both immunosuppression following transplantation [47] and renal cell cancer control [22].
Javaid et al. published a two-patient case series of native kidney RCC in the presence of a functioning renal transplant [48]. Both patients underwent native nephrectomy for high-risk RCC, followed by a change in their immunosuppression therapy from a calcineurin inhibitor to mTOR inhibitor sirolimus. Both patients remained recurrence free at 3 years.
A systematic review of case series and case reports of solid renal masses in the renal graft reported that of 163 patients identified, 29 had their immunosuppression protocol adjusted with 20 switching to mTOR inhibitors [27••].
Conclusion
Masses arising in the renal graft after transplantation may be benign or malignant. Investigation and management will depend on the timing of identification of the mass during the transplantation pathway. Tumours detected post-transplantation are investigated and managed to mirror those in the general population with a particular emphasis on preservation of graft function. In an environment of increasingly elderly organ donors and increased graft survival, a mass in the renal allograft is likely to become an increasingly frequent issue facing urologists and transplant surgeons.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
NHS Blood and Transplant. Organ donation and transplantation: activity report 2017/18. 2018.
Desai R, Collett D, Watson CJ, Johnson P, Evans T, Neuberger J. Cancer transmission from organ donors - unavoidable but low risk. Transplantation. 2012;94(12):1200–7.
Myron Kauffman H, McBride MA, Cherikh WS, Spain PC, Marks WH, Roza AM. Transplant tumor registry: donor related malignancies. Transplantation. 2002;74(3):358–62.
British Transplantation Society. Guidelines for living donor kidney transplantation. Fourth Edition [Internet]. 2018. Available from: www.bts.org.uk
Ploussard G, Chambade D, Meria P, Gaudez F, Tariel E, Verine J, et al. Biopsy-confirmed de novo renal cell carcinoma (RCC) in renal grafts: a single-centre management experience in a 2396 recipient cohort. Br J Urol Int. 2011:195–9.
Tillou X, Doerfler A, Collon S, Kleinclauss F, Patard JJ, Badet L, et al. De novo kidney graft tumors: results from a multicentric retrospective national study. Am J Transplant. 2012;12(12):3308–15.
Nankivell BJ, Kuypers DR. Diagnosis and prevention of chronic kidney allograft loss. Lancet. 2011;378(9800):1428–37.
Naesens M, Heylen L, Lerut E, Claes K, De Wever L, Claus F, et al. Intrarenal resistive index after renal transplantation. N Engl J Med. 2013;369(19):1797–806.
Breda A, Budde K, Figueiredo A, Garcia E, Olsburgh J, Regele H, et al. EAU guidelines on renal transplantation. 2019.
Kidney Disease Improving Global Outcomes. KDIGO Clinical Practice Guideline for the care of kidney transplant recipients. Am J Transplant. 2009;9(Supplement 3):S131–55.
Kasiske BL, Vazquez MA, Harmon WE, Brown RS, Danovitch GM, Gaston RS, et al. Recommendations for the outpatient surveillance of renal transplant recipients. J Am Soc Nephrol. 2000;11:S1–86.
The Renal Association, British Transplantation Society. Clinical practice guideline in post-operative care in the kidney transplant recipient. 2017.
Knoll GA, Blydt-Hansen TD, Campbell P, Cantarovich M, Cole E, Fairhead T, et al. Canadian Society of Transplantation and Canadian Society of Nephrology commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Kidney Dis. 2010;56(2):219–46.
Heemann U, Abramowicz D, Spasovski G, Vanholder R. Endorsement of the Kidney Disease Improving Global Outcomes (KDIGO) guidelines on kidney transplantation: a European Renal Best Practice (ERBP) position statement. Nephrol Dial Transplant. 2011;26(7):2099–106.
SaBTO Advisory committee on the safety of blood tissues and organs. Transplantation of organs from deceased donors with cancer or a history of cancer [Internet]. 2014. Available from: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/2911/transplantation_of_organs_from_deceased_donors_with_cancer_or_a_history_of_cancer.pdf
Nalesnik MA, Woodle ES, DiMaio JM, Vasudev B, Teperman LW, Covington S, et al. Donor-transmitted malignancies in organ transplantation: assessment of clinical risk. Am J Transplant. 2011;11(6):1140–7.
Nicol DL, Preston JM, Wall DR, Griffin AD, Campbell SB, Isbel NM, et al. Kidneys from patients with small renal tumours: a novel source of kidneys for transplantation. BJU Int. 2008;102(2):188–92.
Ogawa Y, Kobayashi T, Shiroma S, Kojima K, Mannami R, Mannami M, et al. Restored kidney transplant using kidneys affected by small tumors: outcomes and lessons learned. Transplant International. 2012; 239.
Mannami M, Mannami R, Mitsuhata N, Nishi M, Tsutsumi Y, Nanba K, et al. Last resort for renal transplant recipients, “restored kidneys” from living donors/patients. Am J Transplant. 2008;8(4):811–8.
• Hevia V, Hassan Zakri R, Fraser Taylor C, Bruins HM, Boissier R, Lledo E, et al. Effectiveness and harms of using kidneys with small renal tumors from deceased or living donors as a source of renal transplantation: a systematic review. Eur Urol Focus. 2019;5(3):508–17 A systematic review of 109 kidneys with excision of small renal masses prior to transplantation demonstrating similar functional outcome to other donor kidneys, and only one local recurrence.
Brook NR, Gibbons N, Johnson DW, Nicol DL. Outcomes of transplants from patients with small renal tumours, live unrelated donors and dialysis wait-listed patients. Transpl Int. 2010;23(5):476–83.
Ljungberg B, Albiges L, Abu-Ghanem Y, Bensalah K, Dabestani S, Montes SFP, et al. European Association of Urology Guidelines on renal cell carcinoma: the 2019 update. Eur Urol. 2019;75(5):799–810.
Gervais DA, Giambarresi L, Lane BR, Campbell S, Davis BJ, Bass EB, et al. Renal mass and localized renal cancer: AUA guideline. J Urol. 2017;198(3):520–9.
• Tillou X, Guleryuz K, Collon S, Doer A. Renal cell carcinoma in functional renal graft: toward ablative treatments. Transplant Rev. 2016;30:20–6 Literature review of 201 functional graft renal cell carcinomas reporting tumour histology, and management with tendency to a nephron sparing approaches.
Chen KT, Olszanski A, Farma JM. Donor transmission of melanoma following renal transplant. Case Rep Transplant. 2012;2012:1–3.
Chiu HF, Wen MC, Li JR, Ho HC, Shu KH. Successful treatment with sirolimus for an angiomyolipoma mimicking renal cell carcinoma in a transplanted kidney. Transpl Int. 2015;28(9):1116–20.
•• Griffith JJ, Amin KA, Waingankar N, Lerner S, Delaney V, Ames S, et al. Solid renal masses in transplanted allograft kidneys : a closer look at the epidemiology and management. Am J Transplant. 2017;17:2775–81 A PRISMA methodology literature review reporting epidemiology and management of 174 small renal masses identified in transplant kidney grafts.
Pagano D, di Francesco F, Rosa L, Nwaiwu CA, Li Petri S, Gruttadauria S. Oncocytoma managed by active surveillance in a transplant allograft kidney: a case report. World J Surg Oncol. 2018;16(1):2–5.
Villanueva LAA, Knust M, Quintella L, Suassuna JHR, Araújo NC. Renal oncocytoma in a kidney transplant patient: the imaging features on contrast-enhanced ultrasonography (CEUS): a case report. Brazilian J Nephrol. 2018;40(1):86–90.
Steiner MS, Goldman SM, Fishman EK, Marshall FF. The natural history of renal angiomyolipoma. J Urol. 1993;150:1782–6.
De Luca S, Terrone C, Rocca RS. Management of renal angiomyolipoma: a report of 53 cases (multiple letters) [3]. BJU Int. 1999;83:215–8.
Wein AJ, Kavoussi LR, Partin AW, Peters CA. Campbell-Walsh urology. Eleventh Edition. 2016. p1306.
Davies DM, De Vries PJ, Johnson SR, McCartney DL, Cox JA, Serra AL, et al. Sirolimus therapy for angiomyolipoma in tuberous sclerosis and sporadic lymphangioleiomyomatosis: a phase 2 trial. Clin Cancer Res. 2011;17(12):4071–81.
Dabora SL, Franz DN, Ashwal S, Sagalowsky A, DiMario FJ, Miles D, et al. Multicenter phase 2 trial of sirolimus for tuberous sclerosis: kidney angiomyolipomas and other tumors regress and VEGF- D levels decrease. PLoS One. 2011;6(9).
Engels E, Pfeiffer R, Fraumeni J, Kasiske B, Israni A, Snyder J, et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA J Am Med Assoc. 2011;306(17):1891–901.
Kasiske BL, Snyder JJ, Gilbertson DT, Wang C. Cancer after kidney transplantation in the United States. Am J Transplant. 2004;4:905–13.
Deng FM, Melamed J. Histologic variants of renal cell carcinoma: does tumor type influence outcome? Urol Clin North Am. 2012;39(2):119–32.
Gigante M, Neuzillet Y, Patard J-J, Tillou X, Thuret R, Branchereau J, et al. Renal cell carcinoma (RCC) arising in native kidneys of dialyzed and transplant patients: are they different entities? BJU Int. 2012;110(11b):E570–3.
Tickoo SK, de Peralta-Venturina MN, Harik LR, Worcester HD, Salama ME, Young AN, et al. Spectrum of epithelial neoplasms in end-stage renal disease. Am J Surg Pathol. 2006;30(2):141–53.
•• Turajlic S, Xu H, Litchfield K, Rowan A, Chambers T, Lopez JI, et al. Tracking cancer evolution reveals constrained routes to metastases: TRACERx Renal. Cell. 2018;173(3):581–594.e12 Prospective multicenter study and two validation cohorts assess the genetic evolution and identify genomic drivers of metastatic renal cell carcinoma.
•• Mitchell TJ, Turajlic S, Rowan A, Nicol D, Farmery JHR, O’Brien T, et al. Timing the landmark events in the evolution of clear cell renal cell cancer: TRACERx Renal. Cell. 2018;173(3):611–623.e17 Whole genome sequencing study of 33 clear cell renal cell carcinomas demonstrates that key oncogenic drivers occur as early as late childhood and early adolescence.
Park K, Inoue H, Kim C, Tomoyoshi T. Nephron-sparing surgery for de novo renal cell carcinoma in an allograft kidney: a case report. Int J Urol. 1997;4:611–4.
Leppert JT, Hanley J, Wagner TH, Chung BI, Srinivas S, Chertow GM, et al. Utilization of renal mass biopsy in patients with renal cell carcinoma. Urology. 2014;83(4):774–80.
Eldred-Evans D, Tay A, Rottenberg G, Pattison J, O’Brien T, Olsburgh J. Zero-ischaemia zero-transfusion transplant kidney partial nephrectomy. 2014.
Tillou X, Guleryuz K, Doerfler A, Bensadoun H, Chambade D, Codas R, et al. Nephron sparing surgery for de novo kidney graft tumor: results from a multicenter national study. Am J Transplant. 2014;14(9):2120–5.
Barama A, St-Louis G, Nicolet V, Hadjeres R, Daloze P. Renal cell carcinoma in kidney allografts: a case series from a single center. Am J Transplant. 2005;5(12):3015–8.
Larson TS, Dean PG, Stegall MD, Griffin MD, Textor SC, Schwab TR, et al. Complete avoidance of calcineurin inhibitors in renal transplantation: a randomized trial comparing sirolimus and tacrolimus. Am J Transplant. 2006;6(3):514–22.
Javaid MM, Chowdhury S, Henderson A, Olsburgh J. Advanced native kidney renal cell carcinoma in renal transplant recipients: role of sirolimus as dual anti-cancer and anti-rejection agent. Clin Nephrol. 2013;79(02):154–60.
Acknowledgements
This article was made open access with the financial support of King’s College London.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Kidney Diseases
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.