Abstract
Purpose of Review
The aim of this review paper is to evaluate the current data regarding clinical use of ultrasound (US) for diagnosis of systemic vasculitis.
Recent Findings
In recent years, US has emerged as an image modality taking a central role in the diagnosis and monitoring of vasculitides by measuring vessel wall inflammation and changes in vessel wall thickness. US has been recognized as an important tool predominantly in the diagnosis of large vessel vasculitis (LVV). Signs like the “halo sign” in temporal arteries of patients with giant cell arteritis (GCA) have demonstrated to be a robust marker. In other types of vasculitides the role of US is not well defined yet but could be of help by diagnosing secondary findings when there is organ involvement, like interstitial lung disease in small vessel vasculitis (SVV).
Summary
Different modes of ultrasound (US) are being studied for this purpose, especially since it is a non-invasive technique that can limit exposure to ionizing radiation.
In conclusion there is clear evidence for the use of US particularly color duplex US (CDS) in the diagnosis of LVV like GCA and Takayasu’s arteritis (TAK). Nevertheless, there is urgent need for more data in regard to the use of US in small/medium vessel vasculitis, as well as the role of US in monitoring of patients with LVV.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 Revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Arthritis Rheum. 2012;65(1):1–11.
Jennette JC. Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Clin Exp Nephrol. 2013;17(5):603–6.
Gonzalez-Gay MA, Miranda-Filloy JA, Lopez-Diaz MJ, Perez-Alvarez R, Gonzalez-Juanatey C, Sanchez-Andrade A, et al. Giant cell arteritis in northwestern Spain. Medicine. 2007;86(2):61–8.
Schmidt WA. Imaging in vasculitis. Best Pract Res Clin Rheumatol. 2013;27(1):107–18.
• Buda N, Masiak A, Zdrojewski Z. Utility of lung ultrasound in ANCA-associated vasculitis with lung involvement. PLoS One. 2019;14(9):e0222189 This trial analyzed patients with ANCA-associated vasculitis with lung involvement and compared the findings of CT images and US. In cases of pleural-adjacent CT lesions, there were comparable findings on US, suggesting this modality could be use to follow progression.
Wang H, Li J, Jiang Y, Dai Q, Jiang Y, Hou Y, et al. Polyarteritis nodosa with multiple aneurysms and renal arteriovenous fistula successfully diagnosed by colour Doppler sonography. Clin Rheumatol. 2010;32(S1):89–92.
Özçakar ZB, Fitöz S, Yıldız AE, Yalçınkaya F. Childhood polyarteritis nodosa: diagnosis with non-invasive imaging techniques. Clin Rheumatol. 2016;36(1):165–71.
Son MBF, Newburger JW. Kawasaki Disease. Pediatr Rev. 2013;34(4):151–62.
Mccrindle BW, Cifra B. The role of echocardiography in Kawasaki disease. Int J Rheum Dis. 2017;21(1):50–5.
Kamiya T, Kawasaki T, Okuni M, Katoh H, Babak, Nakano H. Diagnostic criteria of cardiovascular lesions in Kawasaki disease. Report of subcommittee on standardization of diagnostic criteria and reporting of coronary artery lesions in Kawasaki disease. Research Committee on Kawasaki Disease Ministry of Health and Welfare, Tokyo, Japanese Ministry of Health and Welfare. 1984: pp 1–10.
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association [Internet]. Circulation. U.S. National Library of Medicine. 2004 [Cited 2020Jan1]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15505111. Accessed 24 Nov 2019
Wu T-H, Kuo H-C, Tain Y-L, Lin K-M, Kuo H-C, Chien S-J. Common carotid artery intima-media thickness is useful for diagnosis of the acute stage of Kawasaki disease. BMC Pediatr. 2014;14(1):98.
Chen KY, Zannino D, Curtis N, Cheung M, Burgner D. Increased aortic intima-media thickness following Kawasaki disease. Atherosclerosis. 2017;260:75–80.
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 2010;33(8):1122–8.
Ashton-Key MR, Gallagher PJ. False-negative temporal artery biopsy. Am J Surg Pathol. 1992;16(6):634–5.
Borchers AT, Gershwin ME. Giant cell arteritis: a review of classification, pathophysiology, geoepidemiology and treatment. Autoimmun Rev. 2012;11(6–7):A544–54.
• Banz Y, Stone JH. Why do temporal arteries go wrong? Principles and pearls from a clinician and a pathologist. Rheumatology. 2018;57(suppl_2):ii3–ii10 This review described a clinical case that illustrated the high negative predictive value of temporal artery biopsies and discussed the causes and possible solutions to this problem.
Dejaco C, Duftner C, Buttgereit F, Matteson EL, Dasgupta B. The spectrum of giant cell arteritis and polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology. 2016:kew273. https://doi.org/10.1093/rheumatology/kew273.
Terslev L, Diamantopoulos AP, Døhn UM, Schmidt WA, Torp-Pedersen S. Settings and artefacts relevant for Doppler ultrasound in large vessel vasculitis. Arthritis Res Ther. 2017;19(1):167.
Weyand CM, Goronzy JJ. Medium- and Large-Vessel Vasculitis. New Engl J Med. 2003;349(2):160–9.
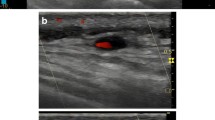
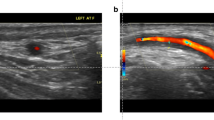
Schmidt WA, Kraft HE, Vorpahl K, Völker L, Gromnica-Ihle EJ. Color duplex ultrasonography in the diagnosis of temporal arteritis. New Engl J Med. 1997;337(19):1336–42.
Aschwanden M, Daikeler T, Kesten F, Baldi T, Benz D, Tyndall A, et al. Temporal artery compression sign - a novel ultrasound finding for the diagnosis of giant cell arteritis. Ultraschall Med. 2012;34(01):47–50.
Aschwanden M, Imfeld S, Staub D, Baldi T, Walker U, Berger C, et al. The ultrasound compression sign to diagnose temporal giant cell arteritis shows an excellent interobserver agreement [Internet]. Clin Exp Rheumatol. 2015 [cited 2020Jan2]. Available from: https://www.clinexprheumatol.org/abstract.asp?a=9106. Accessed 10 Dec 2019
Monti S, Floris A, Ponte C, Schmidt WA, Diamantopoulos AP, Pereira C, et al. The use of ultrasound to assess giant cell arteritis: review of the current evidence and practical guide for the rheumatologist. Rheumatology. 2017;57(2):227–35.
Karassa FB, Matsagas MI, Schmidt WA, Ioannidis JP. Meta-analysis: test performance of ultrasonography for giant-cell arteritis. Ann Intern Med. 2005;142(5):359.
Ball EL, Walsh SR, Tang TY, Gohil R, Clarke JMF. Role of ultrasonography in the diagnosis of temporal arteritis. Br J Surg. 2010;97(12):1765–71.
Arida A, Kyprianou M, Kanakis M, Sfikakis PP. The diagnostic value of ultrasonography-derived edema of the temporal artery wall in giant cell arteritis: a second meta-analysis. BMC Musculoskelet Disord. 2010;11(1):44.
Ultrasound definitions for cranial and large vessel giant cell arteritis: results of a reliability exercise on images and videos of the Omeract Ultrasound Large Vessel Vasculitis Task Force [Internet]. ACR Meeting Abstracts. [cited 2020Jan1]. Available from: https://acrabstracts.org/abstract/ultrasound-definitions-for-cranial-and-large-vessel-giant-cell-arteritis-results-of-a-reliability-exercise-on-images-and-videos-of-the-omeract-ultrasound-large-vessel-vasculitis-task-force/. Accessed 20 Dec 2020
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of Giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess. 2016;20(90):1–238.
Czihal M, Schröttle A, Baustel K, Lottspeich C, Dechant C, Treitl K-M, et al. B-mode sonography wall thickness assessment of the temporal and axillary arteries for the diagnosis of giant cell arteritis: a cohort study [Internet]. Clin Exp Rheumatol. U.S. National Library of Medicine; 2017 [Cited 2019Dec2]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28375835. Accessed 10 Nov 2019
Diamantopoulos AP, Haugeberg G, Hetland H. et al. Diagnostic value of color Doppler ultrasonography of temporal arteries and large vessels in giant cell arteritis: a consecutive case series. Arthritis Care Res 2014;66:113–9.
Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer M, Blockmans D, et al. Trial of tocilizumab in giant-cell arteritis. New Engl J Med. 2017;377(4):317.
Aschwanden M, Schegk E, Imfeld S, Staub D, Rottenburger C, Berger CT, et al. Vessel wall plasticity in large vessel giant cell arteritis: an ultrasound follow-up study. Rheumatology. 2018;58(5):792–7.
Terslev L, Hammer H, Torp-Pedersen S, Szkudlarek M, Iagnocco A, Dagostino M, et al. EFSUMB minimum training requirements for rheumatologists performing musculoskeletal ultrasound. Ultraschall Med. 2013;34(05):475–7.
Miguel ED, Roxo A, Castillo C, Peiteado D, Villalba A, Martín-Mola E. The utility and sensitivity of colour Doppler ultrasound in monitoring changes in giant cell arteritis [Internet]. Clin Exp Rheumatol. 2012 [cited 2020Jan2]. Available from: https://www.clinexprheumatol.org/abstract.asp?a=5526. Accessed 25 Dec 2019
Miguel ED, Beltran LM, Monjo I, Deodati F, Schmidt WA, Garcia-Puig J. Atherosclerosis as a potential pitfall in the diagnosis of giant cell arteritis. Rheumatology. 2017;57(2):318–21.
Soussan M, Nicolas P, Schramm C, Katsahian S, Pop G, Fain O, et al. Management of large-vessel vasculitis with FDG-PET. Medicine. 2015;94(14).
Maeda H, Handa N, Matsumoto M, Hougaku H, Ogawa S, Oku N, et al. Carotid lesions detected by B-mode ultrasonography in Takayasu's arteritis: "macaroni sign" as an indicator of the disease [Internet]. Ultrasound Med Biol. U.S. National Library of Medicine; 1991 [Cited 2020Jan19]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/1685816.
Meini S, Meini S, Franco VD, From VDF, Auteri A, Auteri A, et al. Takayasu's arteritis [Internet]. Circulation. 2006 [cited 2020Jan1]. Available from: https://doi.org/10.1161/CIRCULATIONAHA.106.628206?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub=pubmed
Schmidt WA. Diagnosis of early Takayasu arteritis with sonography. Rheumatology. 2002;41(5):496–502.
Magnoni M, Dagna L, Coli S, Cianflone D, Sabbadini MG, Maseri A. Assessment of Takayasu arteritis activity by carotid contrast-enhanced ultrasound. Circ Cardiovasc Imaging. 2011;4(2):e1–2.
Giordana P, Baqué-Juston M, Jeandel P, Mondot L, Hirlemann J, Padovani B, et al. Contrast-enhanced ultrasound of carotid artery wall in Takayasu Disease. Circulation. 2011;124(2):245–7.
Staub D, Partovi S, Schinkel AFL, Coll B, Uthoff H, Aschwanden M, et al. Correlation of carotid artery atherosclerotic lesion echogenicity and severity at standard US with intraplaque neovascularization detected at contrast-enhanced US. Radiology. 2011;258(2):618–26.
Germanò G, Macchioni P, Possemato N, Boiardi L, Nicolini A, Casali M, et al. Contrast-enhanced ultrasound of the carotid artery in patients with large vessel vasculitis: correlation with positron emission tomography findings. Arthritis Care Res. 2016;69(1):143–9.
Czihal M, Lottspeich C, Schröttle A, Treitl KM, Treitl M, Leipe J, et al. Relapses in three patients with Takayasu arteritis under tocilizumab treatment detected by contrast enhanced ultrasound. Vasa. 2018;47(2):149–52.
Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018;77(5):636–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vasculitis
Rights and permissions
About this article
Cite this article
Lopez, D., Guevara, M. Use of Ultrasound in the Diagnosis and Management of the Vasculitides. Curr Rheumatol Rep 22, 31 (2020). https://doi.org/10.1007/s11926-020-00902-x
Published:
DOI: https://doi.org/10.1007/s11926-020-00902-x