Abstract
Purpose of review
To systematically examine changes in suicide trends following the initial COVID-19 outbreak, focusing on geographical and temporal heterogeneity and on differences across sociodemographic subgroups.
Recent findings
Of 46 studies, 26 had low risk of bias. In general, suicides remained stable or decreased following the initial outbreak – however, suicide increases were detected during spring 2020 in Mexico, Nepal, India, Spain, and Hungary; and after summer 2020 in Japan. Trends were heterogeneous across sociodemographic groups (i.e., there were increases among racially minoritized individuals in the US, young adults and females across ages in Japan, older males in Brazil and Germany, and older adults across sex in China and Taiwan). Variations may be explained by differences in risk of COVID-19 contagion and death and in socioeconomic vulnerability.
Summary
Monitoring geographical, temporal, and sociodemographic differences in suicide trends during the COVID-19 pandemic is critical to guide suicide prevention efforts.
Similar content being viewed by others
Introduction
The SARS-CoV-2 pandemic has brought about a substantial burden of psychosocial stressors (e.g. bereavement of loved ones, fear of contagion and death, isolation and loneliness, downstream negative economic effects), affecting mental health and psychological wellbeing of the general population [1, 2]. Initial evidence from representative longitudinal surveys suggests that prevalence of symptoms indicative of common mental health conditions, such as symptoms of depression or anxiety, may have increased notably following the onset of the pandemic [3,4,5,6,7,8]. According to Global Burden of Disease estimates, prevalence of depression and anxiety increased by around 25% across the globe in 2020 [9].
Additionally, early reports also suggested increases in suicidal ideation in the general population [10, 11], leading to concern that suicide deaths would increase following the initial pandemic outbreak [12]. The first available evidence, however, did not confirm such increases [13]. As the pandemic unfolded, however, it became progressively clear that the impact of the pandemic on suicide across the globe is heterogeneous across place and population subgroups as well as over time. For instance, a large study including data through October, 2020 on 21 different locations identified increases in suicide in Vienna, Austria; Puerto Rico; and Japan (suicide remained stable or decreased in the other 18 study locations) [13]. A systematic review based on 9 original reports of population-based suicide mortality data, also highlighted increases in suicide rates in Japan, noticeable after the summer of 2020, with particularly concerning trends among young females [14].
Variations across place and population subgroups and over time in the impact of the pandemic on suicide should be expected because the intensity of pandemic-related stressors (e.g., COVID-19 incidence and mortality, physical distancing measures, negative downstream economic effects) were also heterogeneous across place and population subgroups and over time. Examining the geographical and temporal variations in suicide trends during the COVID-19 era can enhance our understanding regarding the potential risk or protective role of specific components of the pandemic (e.g., intensity of the initial pandemic outbreak) and contagion containment measures (e.g., stay-at-home mandates). In addition, focusing on the vulnerability to suicide of population subgroups can help identify high-risk individuals and design, implement, and scale-up targeted prevention strategies.
Notwithstanding, no study has systematically reviewed the heterogeneity across place and population groups and over time in variations in suicide during the COVID-19 era, despite potential implications for suicide prevention efforts during the current and future major societal crises. The goal of this review was to systematically examine and summarize the existing evidence on changes in population-based suicide trends during the period following the initial pandemic outbreak, with a focus on assessing geographical and temporal heterogeneity as well as differences across population groups defined by sociodemographic characteristics.
Methods
Search Strategy and Databases
We conducted a systematic integrative literature review, combining the rigor of a systematic review with the flexibility of an integrative review [15]. We searched PubMed, ProQuest Central, and Ebscohost (restricted to PsycInfo and SocINDEX) on July 25, 2022. Search terms were: suicide and (COVID-19 or pandemic or coronavirus or SARS-CoV-2). This review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 guidelines (Supplementary Table S1) [16].
Inclusion and Exclusion Criteria
Supplementary Table S2 outlines the criteria for inclusion in the review. In brief, studies were included if they reported original, peer-reviewed research published between 01/01/2020 and 07/10/2022, and included population-based estimates of suicide counts or suicide mortality rates before and after the initial COVID-19 pandemic outbreak, with or without explicitly estimating the effect of the pandemic on variations in suicide.
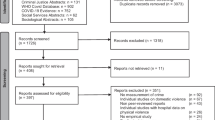
Study Screening and Full-text Review
Two independent researchers (GMA, AS) screened all titles and abstracts separately. In 12 out of 8414 (0.1%) papers initially screened and 2 out of 48 (4%) papers reviewed in full-text, reviewers had to discuss appropriateness of study inclusion. Supplementary Fig. S1 is a flowchart representing the manuscript review process.
Data Extraction, Synthesis, and Analysis
We used an abstraction form to capture all relevant study details, including data on general manuscript information (authors, publication year, setting), methods (period examined; definition of the COVID-19 period; outcome measure; additional covariates), and results (main findings and, when appropriate, results by subgroups). We did not assess quality of suicide data as papers did not include such information.
Analyses of time series data where a potential interruption of the time series (e.g., emergence of the COVID-19 pandemic) is of interest are typically referred to as interrupted time-series analyses (ITSA). There are three common threats to validity in ITSA studies: autocorrelation, seasonality, and non-stationarity (for details, see Appendix 1). The abstraction form included specific variables to indicate if autocorrelation, seasonality, and non-stationarity were explicitly assessed and controlled for; papers were assessed as possibly biased if they failed to address these possible threats to validity. Two independent researchers (GMA, AS) performed an evaluation of the risk of bias of the articles, based on work by Hategeka et al. [17] (see Appendix 1 for details). We dichotomized the scale between low and high risk of bias. Because designs were largely similar across studies, the difference between low and high risk of bias was in most cases defined by use of an appropriate ITSA technique (e.g., Autoregressive Integrated Moving Average [ARIMA] models or segmented regression) with explicit control for autocorrelation, seasonality, and non-stationarity.
Results
Study Designs and Methodological Variation
Table 1 summarizes the characteristics of the 46 studies. A total of 27 studies used suicide counts as the outcome of interest [13, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. Of them, the majority examined monthly suicide counts, except for two reports from Nepal not specifying the time window [18, 37], a study examining daily suicides in Maryland, US [21], two studies conducted in Peru assessing biweekly suicide counts [22, 23], and studies examining periods longer than one month [27, 28, 34, 38, 39, 41]. In 20 studies, the outcome of interest was measured as suicide rate – and expressed as monthly suicide rate [29, 44,45,46,47,48,49,50,51,52,53,54], annual suicide rate [55,56,57,58], or suicide rate using a different time window [59,60,61,62].
There was between-study variation in the definition of the COVID-19 period, largely due to geographical variation in the timing of the first local case of SARS-CoV-2. While 22 studies defined March 2020 as the beginning of the pandemic, [18, 19, 21,22,23, 27,28,29, 34, 36,37,38, 40, 43, 46, 50, 51, 54, 58,59,60,61], 6 studies [13, 20, 24, 44, 47, 52] – including Pirkis et al.’s study featuring data from 21 countries [13], used April 2020, 11 studies used January 2020 [25, 30, 31, 35, 39, 41, 42, 45, 56, 57, 62] and 3 studies February 2020 [48, 49, 53]. The studies by Eguchi et al. [26] and Nomura et al. [32] did not report a specific COVID-19 period.
There was substantial heterogeneity in choice of statistical approach to estimate the difference between expected and observed suicide counts or rates. In general, all approaches aimed at estimating the counterfactual outcome (e.g., monthly suicide count, or monthly suicide rate) had the COVID-19 pandemic outbreak not taken place – in order to then compare expected vs. observed outcomes. The majority of studies adopted an ITSA approach based on some specification of a segmented regression – e.g., Poisson [13, 19, 20, 23, 24, 29, 40, 41, 46, 48, 50, 55, 61], quasi-Poisson [26, 30, 32, 34, 36], negative binomial [31, 42, 51], linear [21, 22, 25, 44, 47], or non-specified segmented regression [45, 54] model with a variety of additional covariables, such as unemployment rate [19], sex [23], intensity of travel restrictions [51], and interaction terms between the covariates [34]. Only 3 studies implemented ITSA based on seasonal autoregressive integrated moving average models [27, 28, 59]. In addition, 2 Japanese studies used a difference-in-difference approach: both included appropriate control for seasonality and non-stationarity [52, 53]. Appendix 1 specifies approaches undertakes to deal with seasonality, non-stationarity, and autocorrelation. All in all, a total of 26 out of 46 included studies (56.5%) were considered at low risk of bias.
Geographical Variation Between Countries
Figure 1 represents suicide variations following onset of the pandemic across the globe. Regarding North America, evidence indicates that suicides decreased in Canada [58] and the United States [56] but increased in Mexico. In Canada, February–March bimonthly suicide rates were 10.8 and 7.3 per 100,000 persons in 2019 and 2020, respectively; [58] decreases were also reported by studies focused on British Columbia, where a comparison of suicide rates between March-August 2020 vs. the average during the same months during the 2010–2019 period yielded an IRR (95% CI) = 0.92 (0.86, 0.98) [59], (and Nova Scotia, with 30 fewer suicides than expected between March 2020 and February 2021) [40]. In the United States, suicide counts were an estimated (95% CI) 2432 (1071, 3791) lower than expected between March and August 2000 [27]. One study highlighted that firearm suicide rates also did not change in the US in 2020, compared to 2019 [57]. In Mexico, suicide increased by 3% (95% CI = 1%, 6%) between April-December 2020. In South America, studies detected no increases in suicide in Brazil [34] and evidence of an initial decrease following the initial pandemic outbreak in Peru [22, 23]. In Asia, studies also revealed heterogeneity across place. There is some evidence of marked increases in suicide in Nepal (25% in 2020 compared to 2019) [37, 44] and India (15% in 2020 compared to 2017) [55]. In the Chinese region of Guangdong [62] and in Taiwan [31, 45], on the contrary, studies suggest decreases in suicide after January 2020, compared to expected rates: an 18.5% decrease between January and June 2020 in Guangdong [62] and 0.08 fewer suicides per 100,000 persons per month throughout 2020 in Taiwan [45]. Japan has been the subject of extensive reporting regarding suicide rates following the initial pandemic outbreak. Taken together, evidence indicates that suicide decreased between the pandemic outbreak and early summer of 2020 [29, 49, 53] and subsequently increased throughout late summer, fall, and winter 2020–2021. According to the study by Tanaka and Okamoto, suicide rates in Japan first decreased by 14% (95% CI: 10%, 18%) between February and June 2020 and then increased by 16% (95% CI: 11%, 21%) between July and October 2020 [53]. Variation in suicide in Japan were heterogeneous across sex and age groups, as discussed below. [26, 29, 30, 32, 41, 47, 49, 52, 53]
At least two large studies suggest that suicide remained stable in Australia in 2020 [25, 48]. Regarding Europe, evidence is also mixed across place: Suicide decreased during the initial phases of the COVID-19 pandemic in Milan, Italy (in terms of suicide counts and in the proportion of autopsies corresponding with suicides between March–April 2020) [43], and the Austrian region of Tyrol (with around 20 fewer suicides than expected between April-September 2020) [24]. On the other hand, between March and December 2020 there were 7% (95% CI: 2%, 12%) increases in suicide rates in Spain (although an initial decrease was detected in Catalonia) [35, 46], and 16% increases in suicide counts in Hungary [36]; and there were increases in suicide in 2020 compared to 2017 – according to one suboptimal study directly comparing crude annual suicide counts [39]. In Norway [38, 61], Finland [50], the Italian region of Emilia-Romagna [42], and the German regions of Rhineland-Palatinate [42] and Leipzig [51], suicide remained stable during the initial months of pandemic.
Geographical Variation Within Countries
Two studies from Nepal and Mexico reported notable within-country geographical variation – most salient increases took place in Sudurpaschim and Karnali provinces, in Nepal [44], and in Mexico City, in Mexico (in fact suicide decreased in other Mexican states, such as Baja California) [20]. Also, three studies examined specific US states: suicide rates decreased by 13% between March 10 and May 20 2020 (compared to the same period between 2014–2019) in Connecticut [60] and by 0.45 per 100,000 persons per month Minnesota and Michigan [54], though suicide counts remained roughly unchanged in Massachusetts [28].
Temporal Variation
Some studies provide evidence that suicide rates changed dynamically over the months following onset of the pandemic. In several locales, an initial decrease in suicide was followed by a subsequent increase – yet the duration of the initial decrease was highly variable across place. In Peru, biweekly suicide counts dropped during the initial weeks of the pandemic, with a slope (95%CI) of 0.9 (0.8, 1.1), for a subsequent increase of 1.2 (0.9, 1.5) that ended up by the end of the stay-at-home mandate in June 2020, with suicide reaching back levels comparable to 2019. In Milan, Italy, compared to the same months in 2019, suicide counts were lower between April 2020 and March 2021, and higher in April 2021. In Catalonia, Spain, compared to 2019, suicide counts decreased in April 2020 for an Incidence Rate Ratio (IRR) (95% CI) = 0.64 (0.41, 1.02) but increased between June and September 2020, with IRRs ranging between 1.14 and 1.31 (95% CIs not reported) [35]. The initial analysis by Pirkis and colleagues in 21 countries, including April-July 2020 data, did not reveal increases in any locale – however, inclusion of data up to October 2020 indicated increases in suicide in Vienna (Austria), Puerto Rico, and Japan – IRRs (95% CI) = 1.31 (1.08, 1.59), 1.29 (1.05, 1.58), and 1.05 (1.04, 1.07), respectively. In fact, the largest body of evidence indicating temporal variation in the impact of COVID-19 on population suicide comes from a series of Japanese studies. Two initial studies including data up to June 2020, indicated a downward trend in suicide in Japan [19, 29]. Notwithstanding, subsequent studies revealed higher-than-expected suicide counts between July and November 2020 [26, 32, 33, 47, 52], with a peak excess 25.8% suicides in October 2020 [30], driving an overall 10% higher-than-expected suicide count in 2020 compared to 2019 [41]. Studies cited the following potential explanations for initial reductions in suicide during the pandemic: a temporal increase in social cohesion, positive effects of remote work and home schooling, or implementation of economic stimulus aid. Subsequent increases in suicide in specific locations were largely attributed to socioeconomic stress.
Variation By Sociodemographic Variables
Several studies report heterogeneity in the effect of COVID-19 on suicide by sociodemographic characteristics. Variations by the most frequent variable of stratification, sex, are summarized in Table 1. All other results stratified by sociodemographic variables, including groups defined by sex and age, are summarized in Table 2. In most settings, effects were homogeneous across sex. However, there were exceptions. In Peru, initial decreases resulted in one fewer female suicide and two fewer male suicides per million residents per month [22]. In Japan, excess suicides between July and October 2020 were entirely driven by increases in female suicide [26, 49]; with male suicide increasing only after October 2020 [32, 52]. In October 2020 in Japan, suicide went up by 61% among women, but only by 6% among men [30]. Between July 2020 and September 2021, the increase was of 31% among women but only 17% among men [47].
In terms of age, several studies reporting age group-stratified results found no relevant results to report. Notwithstanding, a study examining data from Rhineland-Palatinate, in Germany, and Emilia-Romagna, in Italy, revealed increases in suicide among men aged 70 and older [42]. Similarly in Guangdong, China, suicide rates during the COVID-19 period increased only among males and females aged 0–15 (increasing by 150% in males and 127% in females) and 70–79 (increasing by 21% in males and 12% in females) [62]. Further, suicide rates went down in all age groups but older adults in Taiwan – in fact, older adults in Taiwan experienced 40% increases in suicide in August (RR, 95% CI = 1.41, 1.08–1.82) and October 2020 (RR, 95% CI = 1.44, 1.11–1.88) [45]. In Japan, on the contrary, even though suicide increased across sex and age group after October, 2020, increases occurred earlier among females of all ages and young males [41] and were particularly salient among females aged 20–39 (i.e., suicide went up by 94% in June 2020 among females aged 20–29) [19, 52]. Tanaka and Okamoto, in addition, also detected suicide increases among Japanese adolescents [53]. In Brazil, increases affected especially men aged 60 and older and women aged 30–59 in the Northern region, and women aged > 59 in the Northeastern region [34].
Evidence is scarce regarding socioeconomic status (SES): only the study by Arya et al. in India reported that increases were fivefold higher among males residing in low SES states [55]. Along these lines, Eguchi et al. reported results by job type – finding no variation in suicide among self-employed residents and increases in suicide throughout all pandemic periods among housewives (a specific category for females not employed outside of the home) [26].
Last, there is some evidence that suicide dynamics during the initial phases of the pandemic were affected by racial and ethnic minoritization in the United States: a study using state-wide data from Connecticut found that between March 10 and May 20, 2020 suicide increased by 60% among non-White individuals (a group that, in this study, included individuals of Black, Hispanic, Asian, and “Other” ethno-racial background), while it decreased to a 6-year low among White counterparts [60]. Likewise, in Maryland mean daily suicides increased by 94% among Black but decreased by 45% among White residents in 2020 compared to the 2017–2019 period, and after March 5, 2020 suicide had an increasing slope in Black residents (0.30) but a decreasing one in White counterparts (-0.19) [21]. Studies considered increases in suicide among socially and racially minoritized groups, females, young males, and older individuals as supportive of a potential role of socioeconomic stress on suicide risk with higher impact on disadvantaged groups.
Discussion
This systematic integrative literature review included all population-based estimates of changes in suicide during the months after the onset of the COVID-19 pandemic accessible using scientific databases and reported in English, Spanish, or French. We focused on describing heterogeneity in suicide variation across place and over time, as well as across population groups defined by sociodemographic characteristics. We did this for two reasons: first, the experience of the pandemic and of pandemic-related mental health stressors varied markedly across geographical and temporal contexts and persons – that is, “pandemic” as an exposure is ill-defined and, as such, of limited use to guide public health decision-making [63, 64]. Focusing on differences across geographical or temporal contexts or population groups in suicide during the pandemic can guide identification of potential specific pandemic-related stressors (e.g., universal stay-at-home mandates without stimulus payments) or effect measure modifiers (e.g., level of uptake of remote work) that may function as actionable drivers of despair and suicide rates. Second, specific sociodemographic groups may have particularly high suicide risk during the pandemic and should be identified for prioritization of targeted interventions. The main finding was that, even though increases in suicide following the initial pandemic outbreak were not detected in most study locations, changes in suicide during the COVID-19 era varied geographically, temporally, and across population groups.
We found that during the initial months of the pandemic, suicide decreased or remained unchanged in all locations with published data. This is in keeping with a previous systematic review including data up to July 2021 [14]. Interpreting this finding is challenging, given that many experts expected increases in suicide driven by pandemic-related stressors [12], and in light of increases in population prevalence of mental health symptoms [3,4,5,6,7,8] and suicidal thoughts [11] in several contexts. In many studies, reductions in suicide during the pandemic period were partially attributed to a temporal increase in social cohesion generated by the social disruption driven by the pandemic [13, 25, 34, 51]. This phenomenon, sometimes referred to as “pulling together effect” and initially described in the work of Emile Durkheim [65], has been previously reported in the aftermath of natural wars [66], disasters [67], pandemics [65, 68], and other major societal crises. Additional proposed explanations for lower-than-expected suicide rates included: a greater surveillance of youth due to extended stays at home with adult family members [29, 34], reduced access to means such as pesticides or medications [23], crisis response strategies including bolstering mental health services to maintain access [13, 50], extended unemployment benefits and stimulus aids [25, 28], campaigns of mental health awareness bolstering videocall contact [28], reductions in time living alone [23], reductions in commuting time due to work-from-home policies [19, 53], reduction in stress among children and adolescents due to home schooling [19, 29, 53], and in the particular case of Taiwan lack of need for physical distancing measures [31, 45].
As the pandemic evolved, however, subsequent increases in suicide were reported in specific locations: there were higher-than-expected suicide rates in Mexico, Puerto Rico, Japan, Vienna (Austria), Spain, Hungary, and Poland. In studies reporting monthly variation of suicide rates, higher-than-expected suicide rates started to be detected around 3–5 months after the initial outbreak [23, 30, 32, 35, 49, 52, 53]. For instance, several authors found suicide in Japan to have decreased between February and June 2020, with subsequent increases from July 2020 onwards [49, 52, 53]. Two observations stand out regarding suicide increases among specific population groups during the pandemic. First, increases were sex- and age-patterned in some locations. In Japan, increases in suicide took place earlier and were more marked among females (especially young females) than males [26, 30, 32, 49, 52, 53]. In Guangdong (China) [62], Rhineland-Palatinate (Germany) and Emilia-Romagna (Italy) [42], and Taiwan [45], on the contrary, suicides went up only among older adults (especially older men). Second, markers of minoritization and social disadvantage also played a role in suicide variation. For instance, in the United States, although suicide decreased after the initial outbreak in the general population, the decline was driven by decreases among White persons, with immediate increases reported among non-White residents in Connecticut [60] and Black residents in Maryland [21].
Considering all available evidence, this review supports a potential role of (i) differences in risk of COVID-19 contagion and mortality and (ii) minoritization and socioeconomic disadvantage on suicide rates and trends during the pandemic. As mentioned, suicide rates increased disproportionately among older individuals and especially older males in some locations. COVID-19 incidence and mortality were also much higher in older adults than for the rest of the population during the initial phases of the pandemic [69], likely contributing to increased fear of contagion and death, bereavement of partners and close friends, and loneliness due to isolation measures, stressors more acutely affecting older adults compared to their working-age counterparts. Death of a partner or close relative is a major risk factor for suicide in the short-term [70]: the increase in suicide risk following death of a spouse is highest in older adults [71] – especially among older males [72]. Importantly, while differences in risk of COVID-19 contagion and mortality may explain excess suicides among older adults, there are no clear differences between locations with and without increases in suicide among older individuals.
The potential role of minoritization and socioeconomic disadvantage as important actionable effect measure modifiers of the association between pandemic-related stressors and suicide is partially supported by observations from this review. First, suicide did not increase in countries where economic stimulus efforts were rapidly deployed (e.g., Australia [48], United States [57]) but did increase in countries without such policies (e.g., Spain [46], Mexico [20]) – suggesting that market protection measures can moderate increases in suicide rates during major societal crises. Moreover, in Japan, authors highlighted that economic relief policies implemented right after the initial pandemic outbreak were discontinued after June 2020 – which was followed by upward trends in suicide [53]. Second, higher-than-expected suicide rates affected sociodemographic groups at higher economic vulnerability (i.e., at higher risk of unemployment, overrepresented in the hospitality and tourism industries, with lower access to remote job opportunities), such as young males and females of all ages in Japan [26, 41, 52, 53]. Regarding increases in female suicide in Japan, the impact of the pandemic on burden for caregivers [30, 53] (especially following school closures [53]) and on rising rates of domestic violence [26, 32, 33] may also have played a relevant role. All these factors are deeply intertwined, as overall increases in precarious and informal work typically re-establish women as an economically dependent flexible labor supply [73], increasing the gender gap in socioeconomic vulnerability. In the United States suicide increased only among ethno-racially minoritized residents [21, 60], the group with (i) the highest excess COVID-19 mortality [74], (ii) the highest exposure to unemployment, and (iii) the lowest uptake of work-from-home policies [75]. In Mexico, researchers cited overcrowding as a potential cause for excess suicide mediated by excess COVID-19 incidence and mortality, as suicide increases were highest in Mexico City [20]. In Brazil, Orellana and de Souza emphasized that increases took place among older individuals in the Northern and Northeastern regions – the population groups with the lowest access to the Internet [34].
The findings of this review have three important implications for public health decision-making. First, disproportionate increases in suicide among older individuals underscore the importance of targeting older individuals at high-risk for suicide (e.g., following loss of a partner or close friend), reducing social disconnectedness through early, proactive social care evaluation [76] and deploying older age-friendly suicide prevention strategies (e.g., within geriatric facilities). Also, this finding highlights the importance of further assessing differences in policies regulating safety nets for older adults between countries with and without suicide increases in this age group. Second, the enhancing role of minoritization and socioeconomic disadvantage for suicide risk during the pandemic suggests that additional protective socioeconomic measures (e.g., prolonged unemployment subsidies) should be put in place for individuals working low-wage, informal, and contingency jobs, and those with reduced access to work-from-home positions. Third, suicide trends overall and by sociodemographic group should continue to be monitored across the globe, ideally reducing the lag between deaths take place and mortality data are available, given that suicide drivers can vary dramatically over time (e.g., firearm sales have recently gone up in the United States) [77] and to guide early identification of emerging high-risk groups.
This study has strengths worth noting. We based the review on an extensive search strategy that included multiple large databases. In addition, we used multiple reviewers to increase reliability of study selection and data extraction procedures, as well as of assessments of risk of bias. On the other hand, there were important methodological differences across studies (e.g., differences in the temporal definition of the COVID-19 or the control periods or in choice of statistical approach) that may account for part of the observed heterogeneity in results. Most studies, however, defined the COVID-19 period based on the date of the first confirmed case locally, used the previous 1–4 years as control period, and chose appropriate statistical methods for time-series analyses where an intervention (onset of the pandemic) is under consideration (i.e., interrupted time-series analysis using segmented regression or ARIMA models with appropriate adjustment for autocorrelation, seasonality, and non-stationarity). Moreover, the subset of studies examining suicide in Japan during the pandemic used a variety of designs but found overall similar results, suggesting relative robustness to choice of statistical approach.
In conclusion, this systematic integrative review including all population-based studies assessing changes in suicide following the onset of the pandemic found suicide trends during the pandemic to be heterogeneous across place and population subgroups and over time – though suicide rates remained unchanged or decreased in most locations. These findings support a relevant role of two factors modifying suicide risk among specific population groups during the pandemic. First, risk of COVID-19 contagion and mortality, as well as of bereavement and loss due to COVID-19, may explain the excess risk of suicide among older adults and especially males in several places – although explanations to why suicide among older adults only increased in some locations remain elusive. Second, socioeconomic vulnerability (e.g., vulnerability to unemployment, barriers to work-from-home jobs) may explain increases in suicide following interruption of stimulus aids and the excess risk of suicide among females and young males in Japan. Moreover, both factors affected ethno-racially minoritized persons in the United States, whose suicide risk also increased disproportionately. These findings highlight the importance of targeting social disconnectedness and deploying appropriate suicide prevention for older persons, ensuring access to labor market protection measures for socioeconomically vulnerable groups, and maintaining continued monitoring efforts to improve early detection of changes in suicide trends.
References
Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567–76. https://doi.org/10.1016/j.jad.2021.09.098.
Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201–11. https://doi.org/10.1017/S0033291721000015.
Budimir S, Pieh C, Dale R, Probst T. Severe Mental Health Symptoms during COVID-19: A Comparison of the United Kingdom and Austria. Healthcare (Basel). 2021;9(2):191. https://doi.org/10.3390/healthcare9020191.
Pieh C, Budimir S, Delgadillo J, Barkham M, Fontaine JRJ, Probst T. Mental Health During COVID-19 Lockdown in the United Kingdom. Psychosom Med. 2021;83(4):328–37. https://doi.org/10.1097/PSY.0000000000000871.
Brunoni AR, Suen PJC, Bacchi PS. Prevalence and risk factors of psychiatric symptoms and diagnoses before and during the COVID-19 pandemic: findings from the ELSA-Brasil COVID-19 mental health cohort. Psychol Med. Published online April 21, 2021:1–12. https://doi.org/10.1017/S0033291721001719.
Daly M, Robinson E. Anxiety reported by US adults in 2019 and during the 2020 COVID-19 pandemic: Population-based evidence from two nationally representative samples. J Affect Disord. 2021;286:296–300. https://doi.org/10.1016/j.jad.2021.02.054.
Hyland P, Shevlin M, McBride O, et al. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr Scand. 2020;142(3):249–56. https://doi.org/10.1111/acps.13219.
Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8. https://doi.org/10.1016/j.bbi.2020.04.028.
Santomauro DF, Herrera AMM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–12. https://doi.org/10.1016/S0140-6736(21)02143-7.
Mortier P, Vilagut G, Ferrer M, et al. Thirty-day suicidal thoughts and behaviours in the Spanish adult general population during the first wave of the Spain COVID-19 pandemic. Epidemiol Psychiatr Sci. 2021;30:e19. https://doi.org/10.1017/S2045796021000093.
Czeisler MÉ. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69. https://doi.org/10.15585/mmwr.mm6932a1.
Reger MA, Stanley IH, Joiner TE. Suicide Mortality and Coronavirus Disease 2019-A Perfect Storm? JAMA Psychiat. 2020;77(11):1093–4. https://doi.org/10.1001/jamapsychiatry.2020.1060.
Pirkis J, John A, Shin S, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–88. https://doi.org/10.1016/S2215-0366(21)00091-2.
John A, Eyles E, Webb RT, et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. Published online June 17, 2021. https://doi.org/10.12688/f1000research.25522.2.
Torraco RJ. Writing Integrative Literature Reviews: Guidelines and Examples. Hum Resour Dev Rev. 2005;4(3):356–67. https://doi.org/10.1177/1534484305278283.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Hategeka C, Ruton H, Karamouzian M, Lynd LD, Law MR. Use of interrupted time series methods in the evaluation of health system quality improvement interventions: a methodological systematic review. BMJ Glob Health. 2020;5(10):e003567. https://doi.org/10.1136/bmjgh-2020-003567.
Acharya SR, Shin YC, Moon DH. COVID-19 outbreak and suicides in Nepal: Urgency of immediate action. Int J Soc Psychiatry. 2021;67(5):606–8. https://doi.org/10.1177/0020764020963150.
Anzai T, Fukui K, Ito T, Ito Y, Takahashi K. Excess Mortality From Suicide During the Early COVID-19 Pandemic Period in Japan: A Time-Series Modeling Before the Pandemic. J Epidemiol. 2021;31(2):152–6. https://doi.org/10.2188/jea.JE20200443.
Borges G, Garcia JA, Pirkis J, et al. A state level analyses of suicide and the COVID-19 pandemic in Mexico. BMC Psychiatry. 2022;22(1):460. https://doi.org/10.1186/s12888-022-04095-8.
Bray MJC, Daneshvari NO, Radhakrishnan I, et al. Racial Differences in Statewide Suicide Mortality Trends in Maryland During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Psychiat. 2021;78(4):444–7. https://doi.org/10.1001/jamapsychiatry.2020.3938.
Calderon-Anyosa RJC, Kaufman JS. Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med. 2021;143:106331. https://doi.org/10.1016/j.ypmed.2020.106331.
Calderon-Anyosa RJC, Bilal U, Kaufman JS. Variation in Non-external and External Causes of Death in Peru in Relation to the COVID-19 Lockdown. :18.
Deisenhammer EA, Kemmler G. Decreased suicide numbers during the first 6 months of the COVID-19 pandemic. Psychiatry Research. 2021;295:113623. https://doi.org/10.1016/j.psychres.2020.113623.
Dwyer J, Dwyer J, Hiscock R, et al. COVID-19 as a context in suicide: early insights from Victoria, Australia. Aust N Z J Public Health. 2021;45(5):517–22. https://doi.org/10.1111/1753-6405.13132.
Eguchi A, Nomura S, Gilmour S, et al. Suicide by gender and 10-year age groups during the COVID-19 pandemic vs previous five years in Japan: An analysis of national vital statistics. Psychiatry Research. 2021;305:114173. https://doi.org/10.1016/j.psychres.2021.114173.
Faust JS, Du C, Mayes KD, et al. Mortality From Drug Overdoses, Homicides, Unintentional Injuries, Motor Vehicle Crashes, and Suicides During the Pandemic, March-August 2020. JAMA. 2021;326(1):84–6. https://doi.org/10.1001/jama.2021.8012.
Faust JS, Shah SB, Du C, Li SX, Lin Z, Krumholz HM. Suicide Deaths During the COVID-19 Stay-at-Home Advisory in Massachusetts, March to May 2020. JAMA Netw Open. 2021;4(1). https://doi.org/10.1001/jamanetworkopen.2020.34273.
Isumi A, Doi S, Yamaoka Y, Takahashi K, Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse & Neglect. 2020;110:104680. https://doi.org/10.1016/j.chiabu.2020.104680.
Koda M, Harada N, Eguchi A, Nomura S, Ishida Y. Reasons for Suicide During the COVID-19 Pandemic in Japan. JAMA Netw Open. 2022;5(1):e2145870. https://doi.org/10.1001/jamanetworkopen.2021.45870.
Lin CY, Chang SS, Shen LJ. Decrease in Suicide During the First Year of the COVID-19 Pandemic in Taiwan. J Clin Psychiatry. 2021;82(6):21br14137. https://doi.org/10.4088/JCP.21br14137.
Nomura S, Kawashima T, Harada N, et al. Trends in suicide in Japan by gender during the COVID-19 pandemic, through December 2020. Psychiatry Research. 2021;300:113913. https://doi.org/10.1016/j.psychres.2021.113913.
Nomura S, Kawashima T, Yoneoka D, et al. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Research. 2021;295:113622. https://doi.org/10.1016/j.psychres.2020.113622.
Orellana JDY, de Souza MLP. Excess suicides in Brazil: Inequalities according to age groups and regions during the COVID-19 pandemic. Int J Soc Psychiatry. Published online May 27, 2022:002076402210978. https://doi.org/10.1177/00207640221097826.
Pérez V, Elices M, Vilagut G, et al. Suicide-related thoughts and behavior and suicide death trends during the COVID-19 in the general population of Catalonia. Spain Eur Neuropsychopharmacol. 2022;56:4–12. https://doi.org/10.1016/j.euroneuro.2021.11.006.
Osváth P, Bálint L, Németh A, Kapitány B, Rihmer Z, Döme P. Changes in suicide mortality of Hungary during the first year of the COVID-19 pandemic. Orv Hetil. 2021;162(41):1631–6. https://doi.org/10.1556/650.2021.32346.
Pokhrel S, Sedhai YR, Atreya A. An increase in suicides amidst the coronavirus disease 2019 pandemic in Nepal. Med Sci Law. 2021;61(2):161–2. https://doi.org/10.1177/0025802420966501.
Qin P, Mehlum L. National observation of death by suicide in the first 3 months under COVID-19 pandemic. Acta Psychiatr Scand. 2021;143(1):92–3. https://doi.org/10.1111/acps.13246.
Rogalska A, Syrkiewicz-Świtała M. COVID-19 and Mortality, Depression, and Suicide in the Polish Population. Front Public Health. 2022;10:854028. https://doi.org/10.3389/fpubh.2022.854028.
Schleihauf E, Bowes MJ. Suicide and drug toxicity mortality in the first year of the COVID-19 pandemic: use of medical examiner data for public health in Nova Scotia. Health Promot Chronic Dis Prev Can. 2021;42(2):60–7. https://doi.org/10.24095/hpcdp.42.2.02.
Watanabe M, Tanaka H. Increased suicide mortality in Japan during the COVID-19 pandemic in 2020. Psychiatry Research. 2022;309:114422. https://doi.org/10.1016/j.psychres.2022.114422.
Wollschläger D, Schmidtmann I, Blettner M, et al. Suicides During the COVID-19 Pandemic 2020 Compared to the Years 2011–2019 in Rhineland-Palatinate (Germany) and Emilia-Romagna (Italy). Dtsch Arztebl Int. 2021;118(47):814–5. https://doi.org/10.3238/arztebl.m2021.0365.
Calati R, Gentile G, Fornaro M, Tambuzzi S, Zoja R. Preliminary suicide trends during the COVID-19 pandemic in Milan. Italy Journal of Psychiatric Research. 2021;143:21–2. https://doi.org/10.1016/j.jpsychires.2021.08.029.
Acharya B, Subedi K, Acharya P, Ghimire S. Association between COVID-19 pandemic and the suicide rates in Nepal. PLoS ONE. 2022;17(1):e0262958. https://doi.org/10.1371/journal.pone.0262958.
Chen YY, Yang CT, Pinkney E, Yip PSF. Suicide trends varied by age-subgroups during the COVID-19 pandemic in 2020 in Taiwan. J Formos Med Assoc. 2022;121(6):1174–7. https://doi.org/10.1016/j.jfma.2021.09.021.
de la Torre-Luque A, Pemau A, Perez-Sola V, Ayuso-Mateos JL. [Suicide mortality in Spain in 2020: The impact of the COVID-19 pandemic]. Rev Psiquiatr Salud Ment. Published online February 2, 2022. https://doi.org/10.1016/j.rpsm.2022.01.003.
Horita N, Moriguchi S. Trends in Suicide in Japan Following the 2019 Coronavirus Pandemic. JAMA Network Open. 2022;5(3):e224739. https://doi.org/10.1001/jamanetworkopen.2022.4739.
Leske S, Kõlves K, Crompton D, Arensman E, de Leo D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. 2021;8(1):58–63. https://doi.org/10.1016/S2215-0366(20)30435-1.
Osaki Y, Otsuki H, Imamoto A, et al. Suicide rates during social crises: Changes in the suicide rate in Japan after the Great East Japan earthquake and during the COVID-19 pandemic. J Psychiatr Res. 2021;140:39–44. https://doi.org/10.1016/j.jpsychires.2021.05.035.
Partonen T, Kiviruusu O, Grainger M, et al. Suicides from 2016 to 2020 in Finland and the effect of the COVID-19 pandemic. Br J Psychiatry. 2022;220(1):38–40. https://doi.org/10.1192/bjp.2021.136.
Radeloff D, Papsdorf R, Uhlig K, Vasilache A, Putnam K, von Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol Psychiatr Sci. 2021;30:e16. https://doi.org/10.1017/S2045796021000019.
Sakamoto H, Ishikane M, Ghaznavi C, Ueda P. Assessment of Suicide in Japan During the COVID-19 Pandemic vs Previous Years. JAMA Network Open. 2021;4(2):e2037378. https://doi.org/10.1001/jamanetworkopen.2020.37378.
Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021;5(2):229–38. https://doi.org/10.1038/s41562-020-01042-z.
Rossom RC, Penfold RB, Owen-Smith AA, Simon GE, Ahmedani BK. Suicide Deaths Before and During the Coronavirus Disease 2019 Pandemic: An Interrupted Time-series Study. Med Care. 2022;60(5):357–60. https://doi.org/10.1097/MLR.0000000000001700.
Arya V, Page A, Spittal MJ, et al. Suicide in India during the first year of the COVID-19 pandemic. J Affect Disord. 2022;307:215–20. https://doi.org/10.1016/j.jad.2022.03.066.
Garnett MF. Suicide Mortality in the United States, 2000–2020. 2022;(433):8.
Kegler SR, Simon TR, Zwald ML, et al. Vital Signs : Changes in Firearm Homicide and Suicide Rates — United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2022;71(19). https://doi.org/10.15585/mmwr.mm7119e1.
McIntyre RS, Lui LM, Rosenblat JD, et al. Suicide reduction in Canada during the COVID-19 pandemic: lessons informing national prevention strategies for suicide reduction. J R Soc Med. 2021;114(10):473–9. https://doi.org/10.1177/01410768211043186.
Barbic D, Scheuermeyer FX, Barbic SP, Honer WG. Suicide Deaths in British Columbia during the First Wave of the COVID-19 Pandemic. Can J Psychiatry. 2021;66(9):830–1. https://doi.org/10.1177/07067437211018398.
Mitchell TO, Li L. State-Level Data on Suicide Mortality During COVID-19 Quarantine: Early Evidence of a Disproportionate Impact on Racial Minorities. Psychiatry Research. 2021;295:113629. https://doi.org/10.1016/j.psychres.2020.113629.
Stene-Larsen K, Raknes G, Engdahl B, et al. Suicide trends in Norway during the first year of the COVID-19 pandemic: A register-based cohort study. Eur Psychiatry. 2022;65(1):e26. https://doi.org/10.1192/j.eurpsy.2022.17.
Zheng XY, Tang SL, Ma SL, et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open. 2021;11(6):e045317. https://doi.org/10.1136/bmjopen-2020-045317.
Cole SR, Frangakis CE. The consistency statement in causal inference: a definition or an assumption? Epidemiology. 2009;20(1):3–5. https://doi.org/10.1097/EDE.0b013e31818ef366.
Hernán MA, Taubman SL. Does obesity shorten life? The importance of well-defined interventions to answer causal questions. Int J Obes (Lond). 2008;32(Suppl 3):S8-14. https://doi.org/10.1038/ijo.2008.82.
Bastiampillai T, Allison S, Brailey J, Ma M, Wa SK, Looi JCL. Pandemics and Social Cohesion: 1918–1920 Influenza Pandemic and the Reduction in US Suicide Rates. Prim Care Companion CNS Disord. 2021;23(3):20com02882. https://doi.org/10.4088/PCC.20com02882.
Thomas K, Gunnell D. Suicide in England and Wales 1861–2007: a time-trends analysis. Int J Epidemiol. 2010;39(6):1464–75. https://doi.org/10.1093/ije/dyq094.
Matsubayashi T, Sawada Y, Ueda M. Natural disasters and suicide: evidence from Japan. Soc Sci Med. 2013;82:126–33. https://doi.org/10.1016/j.socscimed.2012.12.021.
Gaddy HG. Social distancing and influenza mortality in 1918 did not increase suicide rates in the United States. SSM Popul Health. 2021;16:100944. https://doi.org/10.1016/j.ssmph.2021.100944.
Goldstein JR, Lee RD. Demographic perspectives on the mortality of COVID-19 and other epidemics. Proc Natl Acad Sci. 2020;117(36):22035–41. https://doi.org/10.1073/pnas.2006392117.
Ajdacic-Gross V, Ring M, Gadola E, et al. Suicide after bereavement: an overlooked problem. Psychol Med. 2008;38(5):673–6. https://doi.org/10.1017/S0033291708002754.
Mogensen H, Möller J, Hultin H, Mittendorfer-Rutz E. Death of a Close Relative and the Risk of Suicide in Sweden-A Large Scale Register-Based Case-Crossover Study. PLoS One. 2016;11(10):e0164274. https://doi.org/10.1371/journal.pone.0164274.
Erlangsen A. Loss of partner and suicide risks among oldest old: a population-based register study. Age Ageing. 2004;33(4):378–83. https://doi.org/10.1093/ageing/afh128.
Insarauto V. Women’s Vulnerability to the Economic Crisis through the Lens of Part-time Work in Spain. Work Employ Soc. 2021;35(4):621–39. https://doi.org/10.1177/09500170211001271.
Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–2. https://doi.org/10.1001/jama.2020.6548.
St-Denis X. Sociodemographic Determinants of Occupational Risks of Exposure to COVID-19 in Canada. Can Rev Sociol. 2020;57(3):399–452. https://doi.org/10.1111/cars.12288.
Van Orden K, Conwell Y. Suicides in Late Life. Curr Psychiatry Rep. 2011;13(3):234–41. https://doi.org/10.1007/s11920-011-0193-3.
McKnight PBLR. Three million more guns: The Spring 2020 spike in firearm sales. Brookings. Published July 13, 2020. Accessed February 1, 2021. https://www.brookings.edu/blog/up-front/2020/07/13/three-million-more-guns-the-spring-2020-spike-in-firearm-sales/.
Acknowledgements
The authors acknowledge Dr. Irene Martinez-Morata for help with data visualization.
Funding
This work was partially funded by grants by the National Institute of Mental Health (Grant number R01-MH121410), the Instituto de Salud Carlos III (Grant number FIS PI19CIII/00037), the Martin Escudero Foundation, and the ASISA Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare no conflicts of interest/competing interests related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martínez-Alés, G., Szmulewicz, A., López-Cuadrado, T. et al. Suicide Following the COVID-19 Pandemic Outbreak: Variation Across Place, Over Time, and Across Sociodemographic Groups. A Systematic Integrative Review. Curr Psychiatry Rep 25, 283–300 (2023). https://doi.org/10.1007/s11920-023-01427-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-023-01427-7