Abstract
Purpose of Review
This review will cover the most relevant findings on the use of machine learning (ML) techniques in the field of non-affective psychosis, by summarizing the studies published in the last three years focusing on illness detection and treatment.
Recent Findings
Multiple ML tools that include mostly supervised approaches such as support vector machine, gradient boosting, and random forest showed promising results by applying these algorithms to various sources of data: socio-demographic information, EEG, language, digital content, blood biomarkers, neuroimaging, and electronic health records. However, the overall performance, in the binary classification case, varied from 0.49, which is to be considered very low (i.e., noise), to over 0.90. These results are fully justified by different factors, some of which may be attributable to the preprocessing of the data, the wide variety of the data, and the a-priori setting of hyperparameters. One of the main limitations of the field is the lack of stratification of results based on biological sex, given that psychosis presents differently in men and women; hence, the necessity to tailor identification tools and data analytic strategies.
Summary
Timely identification and appropriate treatment are key factors in reducing the consequences of psychotic disorders. In recent years, the emergence of new analytical tools based on artificial intelligence such as supervised ML approaches showed promises as a potential breakthrough in this field. However, ML applications in everyday practice are still in its infancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychosis affects 3% of the global population over their lifetime [1, 2]. The economic burden of these mental disorders is also substantial, both in terms of lost work productivity and direct costs (medications, hospitalizations) [3]. Individuals affected by psychosis have a high likelihood of relapse, with reported rates up to 81.9% five years after an initial recovery [4]; patients also have a higher risk for suicide, especially during the first episodes [5]. Psychosis is still considered a chronic condition associated with considerable disability [2]: in fact, the rates of recovery from psychosis remain low (median is 13.5%) [6] and individuals affected suffer from an astonishing premature mortality [7]. The personal toll suffered by patients and their caregivers in addition to the economic burden for the community make psychosis prevention and early treatment a public health priority [8].
Consistently, with the critical period hypothesis [9, 10], an overwhelming amount of evidence supports the benefits of implementing early detection and intervention in psychotic disorders [11]. Early detected patients show less severe symptoms at care presentation, better global functioning and an overall better quality of life at 2 years [12], lower rates of suicidal behaviors [5] and risk of hospitalizations [4], reduced encounters with the criminal justice system [13, 14], and overall better outcomes up to 10 years after their first episode [15].
Psychotic disorders are usually preceded by a period of variable duration characterized by subthreshold symptoms of psychosis, known as prodromes [16, 17], that include suspiciousness, social withdrawal, diminished attention and concentration, and a drop in overall functioning [16, 17]. However, not all the subjects who will experience prodromal symptoms, or defined as being at high risk for psychosis (CHR-P), will progress to frank psychosis [17,18,19,20,21]. Identifying biomarkers that could be used to determine who will progress to psychosis would allow the delivery of preventive measures to the subgroup that would benefit the most [22].
Studies have struggled so far to identify valid biomarkers of progression to psychosis [23] or schizophrenia [24]. Promising candidate biomarkers have been tested in multiple domains in patients with schizophrenia and individuals with prodromes of psychosis: genetic (e.g., NRG1 gene) [25, 26], brain structures (e.g., gray matter loss, increased levels of neurotransmitters) [27, 28], neurocognitive performance (e.g., working memory, attention deficit) [29], and neuroendocrine anomalies [30].
Within the many strategies that have been tested during the past year to improve the detection and outcomes of psychosis, machine learning (ML) methodologies have seen a tremendous development [31,32,33,34]. The term machine learning refers to the subdomain of statistics and computer science focusing on the elaboration of complex algorithms able not only to build models from often huge datasets but also to improve their accuracy, imitating the way humans learn. ML can be employed to uncover patterns of risk of conversion to psychosis that could enable clinicians and stakeholders to implement timely intervention to delay or prevent psychosis [35•]. ML tools offer promise for early detection (i.e., to detect first signs of psychosis and help with differential diagnosis) and prediction of treatment response [33]. Lastly, ML could offer a tool to analyze data obtained from Electronic Health Records (EHRs): this represents a complex but invaluable source of information that is routinely collected in a routine clinical setting but infrequently analyzed because of the poor quality of the data, the lack of standardized instruments, and the large volume of information.
Given the tremendous development of ML approaches to analyze data regarding non-affective psychosis, a review of the most current literature is needed.
Methods
This narrative review will cover the most relevant findings on the use of ML techniques in the field of non-affective psychosis, by summarizing the studies published in the last 3 years.
The authors searched the following electronic databases: Ovid MEDLINE, Embase, Psycinfo, and Cochrane.
The search used a combination of controlled vocabulary and free-text terms to capture the concepts of “psychosis” and “machine learning.” Example searches are as follows: bipolar or delusion* or hallucination* or psychoses or psychosis or psychotic or schizophren* or schizoaffective or mania or manic and “artificial intelligence” or “deep learning” or “machine learning” or “neural network*.” In addition, a manual search was conducted based on literature references of relevant articles. We focused on recent articles in the English language. Full-text review of the included studies was carried out, and data were extracted on study’s characteristics and outcomes.
Results
Given the lack of standardized identifiable biomarkers for psychosis, research has explored different sources of reliable information that could be analyzed by means of ML to improve their accuracy and statistical power.
Specifically, sociodemographic information, EEG, neuroimaging (MRI, PET), neurocognitive assessments, psychometric scales, genetic genotyping, blood and CSF immunology, digital phenotyping (e.g., social media, smartphone use), and speech profiling have been investigated.
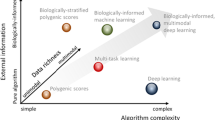
The studies included in this review employed an assortment of ML techniques, mainly supervised algorithms, comparing their performance in various clinically significant tasks.
The most frequent types of data explored were neuroimaging data, mostly from MRI, followed by EEG, language characteristics, and genetic information. There was considerably less evidence regarding the immediate clinical utility of analyzing digital phenotyping data and electronic health records (EHRs). This difference might be explained by the better suitability of the certain type of information to be processed by currently established ML algorithms, as well as the wide heterogeneity in data sources and structure. The technique that was most frequently applied in the included studies was SVM, while unsupervised ML algorithms were rarely employed, principally for data pre-processing, for example adopting PCA for dimensionality reduction.
The main sources of information that have been employed in ML algorithms will be summarized below.
Socio-Demographic Factors
Given the complex interconnectivity of this type of data, ML might represent a powerful tool able to untangle it and extract relevant patterns. In our review, the studies addressing this challenge employed socio-demographic data to predict the quality of life, healthcare services utilization, transition to psychosis, treatment response, and functional recovery. The combination of socio-demographic factors with other markers, such as clinical features, appeared to improve the accuracy of the ML algorithms.
Beaudoin et al. analyzed with a LASSO algorithm (a regression analysis method that uses variable selection and regularization to improve the predictability and interpretability of the produced statistical model) a cohort of 919 patients with schizophrenia and found patients and parents’ educational level (most likely also associated with socio-economic status) were strong predictors of quality of life, also, female gender was a strong predictor [36].
In order to build the NAPLS2 calculator [37], Koutsouleris et al. included demographic and clinical features and found that a supervised ML approach was able to have a balanced accuracy of 68% in the identification of those individuals who will subsequently transit to psychosis (specificity was 73%, sensitivity 63%) [38].
In order to predict resources used by patients with non-affective psychosis, logistic regression, classification tree, and random forest methods were applied: Kwakernaak et al. found that the number of psychotic episodes, paid employment, and engagement in social activities affected healthcare consumption [39]. Moreover, the random forest method was found to be the best suited to model risk factors. Legge et al. found that ML approaches such as the conditional inference random forests model identified age at onset, premorbid IQ, and poor social adjustment to be the best predictors of treatment-resistant psychosis, with an accuracy of 0.59, mirroring findings from regression analyses [40].
Similarly, Leighton found that clinical routine data assessment such as employment status at baseline and severity of psychotic symptoms (suspiciousness, hostility, delusions) were able to positively or negatively predict rates of functional recovery respectively (measured as being employed, in education, or training), with an accuracy of 85% by applying elastic net regularized logistic regression models [41].
EEG has often been investigated as a potential tool for early identification: it is a non-invasive assessment, versatile, and with a limited cost [42•]. In our review, the most promising results obtained by exploiting encephalographic data were achieved in discriminating individuals with schizophrenia from healthy subjects and in predicting response to clozapine and ECT [43]. As expected, a generally lower accuracy was noted for the algorithms seeking to classify psychotic and depressed patients.
For instance, Baraditis demonstrated that microstate alterations obtained by resting state EEG and analyzed with SVM supervision were able to discriminate individuals with schizophrenia by healthy controls, with high accuracy (82.7%), sensitivity (83.5%), and specificity (85.3%) [44]. Deep learning convolution neural network was successfully applied to examine multi channels auditory related EEG single trials to distinguish subjects with schizophrenia from healthy controls with an accuracy of 78% [45]. A linear discriminant analysis classifier was successfully applied to test if resting state EEG was not only able to discriminate schizophrenia patients from controls (with an accuracy of 80.66%) but also to stratify patients based on their symptom severity, with an accuracy as high as 88.10% for positive symptoms [46]. Masychev et al. found that patients with schizophrenia have distinctive features at the auditory odd-ball P300 EEG (a measure of brain connectivity, where the presentation of a continuous series of similar tones at a somewhat moderate rate, and the reaction of the participant to this “oddball” stimulus is recorded with EEG) when analyzed by means of supervised ML tools with an accuracy of 92.68% [47]. Moreover, the inferior frontal gyrus EEG features, analyzed with supervised ML methods, most accurately classify schizophrenia patients from controls (accuracy 78.95%) and positive from negative type schizophrenia (accuracy 89.29%) [48]. Linear discriminant analysis and SVM classifiers were also applied to data drawn by the application of EEG to distinguish features of the disease in subjects with schizophrenia from others with depressions, or controls: the SVM classifier showed good accuracy in distinguishing schizophrenia or depressed patients from controls (71.31% and 74.55% respectively), lower performance in distinguishing patients with schizophrenia by those with depression (59.71%) [49]. Finally, Ciprian et al. developed a linear discriminant analysis algorithm to study auditory EEG measures of connectivity activities in the brain of 57 individuals with schizophrenia, to predict response to clozapine treatment with an impressive accuracy of 95.83% [50]. From the same group, Masychev et al. applied a two-step ML analysis, that was able to distinguish most responders to clozapine from least responders, with an accuracy of 89.90% [43]. Moreover, resting-state EEG was found to be a good predictor of response to ECT in patients with schizophrenia [51] (total accuracy 92.68%): transfer entropy, which represents information flow at the EEG, was used as the key information in the random forest method. These studies provided further evidence to support the use of ML tools to analyze EEG data to discriminate the best candidates to clozapine or ECT treatment.
Language
Given that psychotic disorders are often characterized by disorganized speech (loosening of associations) and content disorders (delusions, echolalia) [52], investigators have applied a variety of natural language (NLP) techniques supervised linear discriminant analysis and supervised leave-one-subject-out cross validation + convex hull classifier to perform speech analysis to identify schizophrenia early in the course of the disease. In the studies included in this review, both form and content features of speech were examined not only in identifying psychosis or transition to illness but also in differentiating schizophrenic patients based on symptom clusters. In our sample, the speech analysis of individuals at clinically high risk for psychosis appears to provide the best results in terms of accuracy.
A study conducted in prodromal individuals found that language alterations including reduced usage of possessive pronouns and semantic coherence had an 83% accuracy in predicting psychosis onset in the training dataset (and 79% in a further independent prodromal sample) and an accuracy of 72% in discriminating patients who recently converted from psychosis from controls [53]. This finding was confirmed by Rezaii et al. that investigated speech in prodromal individuals [54]: progression to psychosis was predicted by low levels of semantic density and an increased tendency to talk about voices and sounds (with an impressive 90% of accuracy, analyzed by a supervised neural network). Speech profile was analyzed with several ML tools, such as supervised gradient boosting [55], latent semantic analysis [56•, 57], random forest [55, 56•], SVM with radial basis function [58•], and multi-layer perceptron [58•]. In their extensive reviews, Ratana et al. [58•], Corcoran et al. [59•], and De Boer et al. [56• ,60] provided an overview of the use of speech analysis such as semantic coherence, semantic density, and acoustic analysis via ML, especially within the NLP processing framework, to detect early signs of psychosis: such tools should be considered reliable and valid in the challenging field of early detection of psychosis and major psychiatric disorders. Also, speech analysis could be a useful tool to detect subjects with schizophrenia within the general population, by analyzing their written excerpts transcribed from their verbal utterances, employing supervised techniques (word2vec, SVM with radial basis kernel) [53]. Results from the study by [57] Sarizynksa-Wawer et al. were superior in terms of accuracy than clinically-based assessment, with an accuracy of 80%, highlighting the need to include such analysis in routine evaluation. Within this line of investigation, Tan et al. found that schizophrenia patients had higher incidences of speech aberrance across five types of variables [55]: utterance, single words, speaking rate, turns, and formulation errors. By using supervised gradient boosting and random forest algorithm, 21 speech variables across the above-mentioned types were significant classifiers for a schizophrenia diagnosis with a specificity and sensitivity up to 90% for both models. Moreover, ML techniques can distinguish subjects with positive or negative symptoms based on their speech acoustics, with an accuracy of 86.2%, as shown by De Boer et al. [60].
Digital Phenotyping
Given the availability of passive data from electronic devices such as smartphones or smartwatches, it is easy to postulate that ML techniques have great potential to become extremely useful for analyzing these large volumes of data for the early identification of psychosis or the transition between the different phases of illness [53, 61,62,63]. Researchers scanned Facebook content, texts, and Google searches to be able to predict psychosis or relapse applying SVM and random forest that mastered the task with a maximum accuracy of 96%. More so, latent semantic analysis can be extremely helpful to monitor social media in order to screen for and predict transition to psychosis, as summarized in Feldman et al. review [64]. For example, a random forest algorithm was able to distinguish the social media post text of subjects with schizophrenia from those of healthy control with an accuracy of 96% [65]. SVM algorithm and random forest were valid tools to predict a diagnosis of schizophrenia spectrum disorder and a relapse, with an AUC of 0.74 and 0.71 respectively [66] by analyzing text originating from Google searches. Moreover, by analyzing Facebook activity archives with a supervised random forest, the algorithm was able to distinguish subjects with schizophrenia, from those with mood disorders or healthy controls, with high accuracy. More importantly, the analysis of Facebook content alone (e.g., choice of words, punctuation) was able to predict a diagnosis over a year in advance of hospitalization. A validated, structured questionnaire was administered through the smartphone to 260 patients with psychosis and 212 controls, in order to capture mental states daily: within the various ML techniques applied (supervised random forest, SVM, Gaussian processes, logistic regression, and neural networks), the SVM with radial kernel achieved an accuracy of 82% in distinguishing emotional patterns of patients from controls [67].
Blood and CSF Biomarkers
Blood biomarkers have also been studied as potential candidates that could identify individuals at risk of developing psychosis early in the course of illness [25]. Some of the studies we analyzed focus their attention on plasma proteomic data and inflammatory alteration (such as neurotrophins and oxidative stress markers) in cerebrospinal fluid. These markers combined with ML techniques were able to discern between SCZ and BD and to predict progression to psychotic [21]. Peripheral plasma proteomic data (mostly indicating a dysregulated complement and coagulation cascade) paired with baseline clinical data were successfully used to identify those individuals who will convert from clinical high risk to frank psychosis: ((AUC), 0.95) [68]. Moreover, the model was able to predict who, 6 years later, will have psychotic experience (PPV, 67.8%; and NPV, 75.8%) [68]. Different algorithms have also been tested to analyze CSF alterations to investigate if subjects with schizophrenia show compartment-specific alterations from classical inflammatory CNS disease with high accuracy (0.88 psychosis vs intracranial hypertension) [69]. Supervised ML has been also used to analyze biomarkers including neurotrophins, inflammatory (IL-10), and oxidative stress markers (e.g., glutathione peroxidase), associated with psychosis: the supervised algorithm failed to distinguish BD from SCZ (accuracy = 49%), but was able to reach a prediction accuracy of 77.5% and 72.5% to identify, respectively, patients with SCZ and BD from controls [70]. It is possible that affective and non-affective psychosis share the same pathophysiological mechanisms so that it is hard to distinguish them by using these biological markers [71, 72].
Genetics
The high degree of complexity in genetic data represents a hurdle for traditional statistical genetics; however, with the exponential growth of computing power and datasets volume of recent years, ML has emerged as an attractive option. As expected, the studies in our review showed a wide range of performance rating, likely caused by high heterogeneity in study design. Even for this type of biomarker, the integration with different data sources, e.g., brain morphology or cognitive features, seems to yield better predicting results.
Genetic analysis is also becoming popular in the field, given the initial evidence of a potential role of both inherited as well as de novo mutation variants [105] in neuronally expressed genes [73, 74], contributing to synaptic dysfunction in the pathogenesis of SCZ. Trakadis applied the supervised Extreme Gradient Boosting (XGBoost) with regularization in a case–control study (2545 SCZ and 2545 controls) to identify genetic markers of a risk for developing SCZ (accuracy = 0.85, sensitivity = 0.85, specificity = 0.86) including genes that regulate neurogenesis and neuronal development, synaptic plasticity, memory, and axonal development [75]. A larger schizophrenia case–control study of 11,853 subjects applied supervised support vector machines (SVM) with linear and radial basis function kernel methods to identify possible genes contributing to the risk of developing SCZ [76]: the sensitivity and specificity were lower compared to the Trakadis study (AUC 0.60–0.66); moreover, its prediction accuracy was lower than that obtained by the use of polygenic risk score [77, 78]. A further study [79] tried to test the effect of 77 risk loci known to be strongly associated with SCZ to predict six different cognitive phenotypes in subjects with schizophrenia, finding that polygenic risk scores and random forest had similar predictive strength and error. However, as highlighted in the systematic review conducted by Bracher-Smith et al. [31], ML methods performance measures have a wide range of abilities (from 0.48 to AUC 0.95) and are still inadequate for prediction modeling: the most commonly employed were supervised naïve Bayes, k-nearest neighbors, penalized regression, random forest, Gaussian processed, SVM, and neural networks. Finally, as Yang et al. underlined in their research on individuals with schizophrenia, ML tools can become even more precise predictive tools when combining genetic and brain morphology data [80]. A further example in this sense is the work by Chen et al. [81, 82] that applied an updated biologically imported machine learning (BioMM) approaches to identify a blood DNA methylation signature that could differentiate schizophrenia from healthy control, and investigate the association of peripheral biomarkers, and neural functioning. Blood-based immunological biomarkers were combined with cognitive data in a multi-domain data integration machine learning model in order to differentiate subjects with schizophrenia from healthy controls with a sensitivity of 84% and specificity of 81% [83].
Neuroimaging
Given the high clinical heterogeneity of psychiatric disorders, the kaleidoscopic presentation at onset and the dynamic evolution, ML methods have been largely employed to analyze neuroimaging data, alone or in combination with other evaluations including blood biomarkers, neuropsychological tests, and clinical structured assessment. With a very few exceptions represented by the application of unsupervised algorithms (non-negative matrix factorization) to analyze data from magnetoencephalography and structural MRI in first-episode schizophrenia patients [84], most studies applied supervised ML techniques.
The vast majority of the studies focusing on the prediction of psychosis conversion applied ML to resting state MRI. Koutsouleris et al. found that it was possible to increase by 40% the diagnostic certainty of subjects who will convert to frank psychosis by applying the MRI-based biomarker, specifically the prefrontal perisylvian and subcortical brain structures [85, 86]. Transition outcomes were correctly predicted in 80% of test cases using MRI-based predictors, which increased prognostic certainty by 36% (sensitivity: 76%, specificity: 85%) [87].
Kambeitz et al. tried to test an ML tool to predict global functioning outcomes at the individual level, by focusing on cortical area reductions in superior temporal, inferior frontal, and inferior parietal areas, with an accuracy of 82%, underlining the utility of ML in stratifying the risk to progression towards psychosis in ultra-high risk individuals [88, 89].
Resting state MRI alone can help build a machine-learned classifier for diagnosing schizophrenia with an accuracy of 87% [90]. Structural MRI is gaining importance to help differentiate between SCZ and healthy controls, as summarized in de Filippis et al. review [91•], as SVM could reach an accuracy of 100% if combined with more recent ML tools [92]. A parameter that has been studied as a potential biomarker of psychosis is the disrupted functional asymmetry: this value in the left thalamus discriminated control vs FEP/UHR individuals with high sensitivity (68.42% and 81.08% respectively) [93]. Antonucci et al. found that SVM built with a repeated nested cross-validation framework was able to distinguish schizophrenia patients from HC by computing attentional control task in fMRI, to identify a pattern of connectivity alterations, with an accuracy of 66.9% [94]. An explainable deep neural network framework provided insight on some brain-based imaging markers, especially decreased density in the insula and frontal and superior temporal lobe, and reduce white matter in the cingulum, hippocampus, with high accuracy (up to 84%) for gray matter [95]. ML was also employed to discriminate subjects with schizophrenia from healthy control with an accuracy of 0.72% [96], or predict the response to treatment in first-episode drug naïve subjects, with an accuracy of 82.5% [97]. Also, deep neural network models were applied to identify brain abnormalities with an accuracy of 81.5% [98] supervised SVM-RFE combining functional and structural MRI was able to distinguish schizophrenia patients from HC with an accuracy of up to 80% [99], and combining polygenic risk score and structural imaging methods with 71.6% accuracy by exploring data of more than 1000 subjects from eight independent sites across China [100].
Individual structural and functional connectivity networks can also help to distinguish subjects with SCZ from healthy controls, as shown by Arbabshirani et al. [101] and Han et al. [102]. These networks were analyzed by Han et al. using SVM in SCZ and MDD patients. SCNMF (supervised convex nonnegative matrix factorization) was successfully employed to draw the distinct characteristics of the two diagnoses, with an 82.6% accuracy. The inferior parietal lobule, middle cingulate, and cingulate cortex were the most discriminative areas in terms of functional properties: as Zeng et al. pointed out, those regions are the ones involved in the salience, control, and default network [103]. Qureshi et al. focused on functional connectivity as a potential biomarker of SCZ, with an accuracy of 0.99 [104]. Moreover, aberrant connectivity in temporal and occipital regions resulted in a good prediction marker, according to Li et al. [105]. Anticorrelated networks between sub-cortical and cortical areas were found to be a strong marker of schizophrenia (accuracy = 0.69) [106].
Sensorimotor circuits also might play a relevant role in the pathogenesis or clinical presentation of SCZ, as demonstrated by the high accuracy (0.95) of the ML algorithm (SVM) applied by Guo et al. [107]. Linear SVM and nonlinear (decision tree) ML algorithms can be helpful to predict the outcomes of at 1 year, specifically by looking at the dynamics of resting state functional connectivity with the default mode network with an accuracy ranging between 75 and 90% [108]. Finally, an ML algorithm could possibly inform about the risk of developing psychosis in non-affected siblings of patients with schizophrenia, as hypothesized by Morgan et al. based on the results of their study on functional connectivity patterns [109].
Given that MRI scans are easily administered, they should be included in the routine baseline assessment of individuals at their first episode of psychosis, or under evaluation for psychosis risk. The advantages are considerable: first, MRI can pick up rare organic causes of psychosis (e.g., tumors), but they can also track the progression of psychosis in the brain (e.g., measures of cortical thickness). However, despite being MRI a very promising tool, it has not been fully implemented in clinical practice because of several translational challenges: first, MRI are quite expensive and given the resources constraints in many healthcare services it might be not easy to charge for this “unnecessary cost”, second, neuroimaging sessions take time to be performed (at least 30–40 minutes per session) and again it might not be suitable for working patients (who might have limited time available), or for individuals who struggle with claustrophobia or other forms of anxiety.
Electronic Health Records
In order to offer a precision medicine approach, it might be necessary to create more population-based data reflecting the real incidence of mental disorders and to use electronic health records (EHRs) [110]. In that regard, EHRs have a lot of potential for speeding up clinical research and for helping clinicians to predict the outcome for each patient [111]. For example, Holderness et al. used two types of artificial neural networks (ANN), multiple multilayer perceptron (MMP) and RBF, to predict whether sentences in a patient’s EHR are linked to one or more of the identified risk factor domains for readmission [112]. Overall agreement was good when compared to annotators, with a mean accuracy of 80.5%. Senior et al. [113] developed a natural language processing technique in order to extract variables from clinical notes to predict risk factors for suicide in 57 patients with SCZ and BD. In comparison to the manual evaluation, the overall accuracy was good (the overall micro precision was 0.77, recall was 0.90, and F1 was 0.83.).
ML to Predict Treatment Outcome
Multiple attempts have been made to predict the course of psychosis in research using ML [114, 115] with inconsistent accuracy (up to 70%). Researchers tried to identify some markers to forecast that, for example, depressive symptoms, poorer educational attainment, functional problems, unemployment, and unsatisfied psychosocial demands and antipsychotic medication were some of the strongest ones. Lower education, functional deficits, unemployment, and unmet psychosocial needs discovering a marker to foretell the response to antipsychotic is a promising way to apply the ML technique: resting-state functional MRI combined with LASSO was used to evaluate the clozapine response in 3 months.
One of the first studies that used ML to predict outcomes in an FEP sample was conducted by Koutsouleris et al.: lower education, functional deficits, unemployment, and unmet psychosocial needs were identified as the most accurate predictors of 4- and 52-week outcomes (with an accuracy of 73.8–75%) [38, 87]. A similar study was conducted a few years later on a sample of 523 subjects diagnosed with schizophrenic disorders, by applying a linear SVM and recursive feature elimination within a nested cross-validation design to recognize patterns in a wide range of genetic, clinical, and environmental variables. The accuracy in predicting symptomatic outcome was 62.2 to 64.7%. The most important predictors were global assessment of functioning areas, psychotic and depressive symptoms, broad quality-of-life indicators and overall functioning, and antipsychotics use; psychosocial needs were also confirmed as a strong predictor [116].
Antipsychotics represent the core component of any comprehensive psycho-social treatment for psychosis [117]. However, two features have characterized psychosis treatment so far: no biomarker or clinical characteristic has been identified as an indicator of antipsychotic response [118]; second, treatment-resistant psychosis emerges in up to a third of patients [119, 120] and there are no reliable tools to predict the lack of response to a certain antipsychotic. Thus, ML holds the promise to help clinicians in moving towards a more personalized pharmacotherapy to increase the accuracy and relevance of predictions for pharmacological treatment outcomes [121]. Sarpal et al., using resting-state functional MRI, found that 91 regions that have functional connections with the striatum were an accurate prognostic tool for treatment response to antipsychotic in acutely psychotic patients [122]; however, the accuracy was 78%. A LASSO algorithm was also used to predict clozapine response at 3 months [123].
A brain source localization (BSL) procedure using the linearly constrained minimum variance (LCMV) beamforming approach was also explored: response to clozapine treatment can be predicted by the symbolic transfer entropy features with an accuracy of 95.83% [124].
Given the high incidence of treatment-resistant schizophrenia, a growing number of studies are delving into the pharmacogenomics of antipsychotics, but despite the efforts that have been made so far, no reliable predictive markers have been identified that might be employed in clinical management and that could enhance the quality of life of these patients. However, recent studies implemented ML methods to investigate the genetics of treatment-resistant schizophrenia, reporting promising findings that could pave the way for the application of pharmacogenomics in the clinical practice [125].
Discussion
This review summarizes the findings of the most current literature on the application of ML techniques for the identification, diagnosis, and treatment of non-affective psychosis.
Most of the studies focused on neuroimaging data, especially MRI, with a specific focus on cortical area reductions in superior temporal, inferior frontal, and inferior parietal areas that could help identifying the progression to psychosis in UHR individuals. The disrupted thalamus functional asymmetry in fMRI matched with SVM and deep neuronal model showed to be a useful marker to distinguish SCZ from healthy volunteers as well as the decreased density in the insula, frontal and superior temporal lobe, or the reduced white matter in the cingulum and hippocampus, or connectivity alterations (tested with a computing attentional control task in fMRI). ML techniques can also be a helpful tool to predict treatment outcome: for example, 91 regions that have functional connections with the striatum have been studied with the LASSO algorithm. The linearly constrained minimum variance (LCMV) was also utilized to predict clozapine response after 3 months.
When dealing with socio-demographic data, the best ML method was found to be the random forest that was able to identify the age at onset, premorbid QI, and poor social activities as the most frequent predictor of psychosis. A lot of studies focused on resting state EEG: SVM seems to be one of the most accurate methods to discriminate healthy controls from patients with SCZ or depression. Moreover, the supervised ML technique matched with auditory EEG revealed to be a useful tool to predict the response to clozapine and ECT treatments.
Supervised ML techniques such as SVM and gradient boosting were used to test language features to distinguish psychotic from healthy people. Low semantic density, higher prevalence of speech aberrance, and increased predisposition to talk about voices and sounds seem to be strictly associated with SCZ patients. Furthermore, random forest and SVM were shown to predict psychosis and relapse by monitoring Google searches and social media posts.
Proteomic and inflammation alterations (such as neurotrophins, IL-10, and glutathione peroxidase) combined with ML technologies were able to distinguish healthy controls from patients with bipolar disorders or schizophrenia. Even genetic features could be some interesting options to explore because it is known that neuronally expressed genes are involved in the etiology of SCZ by causing synaptic disruption. Both SVM and other ML were tested but it was clear that these information about gene loci and DNA methylation need to be combined with cognitive or neuroimaging data to be more accurate.
Such findings are very promising, especially when ML is employed to decipher possible predictors of psychosis by using neuroimaging data; however, it has not been fully implemented in clinical practice because of several translational challenges (cost, resources restraints, claustrophobia). Moreover, almost none of the study provided results stratified by biological sex: given that psychosis has a different epidemiology, clinical presentation, and pathophysiology in the two sexes [126,127,128], there is the necessity to develop adequate data analytic strategies to account for this important biological characteristic.
From a strictly technical standpoint, almost all the studies considered in this review applied supervised ML techniques, which is quite common in the context of both classifications (binary and multiple) and regression. On the other hand, studies incorporating unsupervised ML techniques to preprocess the data, for example operating a dimensionality reduction or identifying the most relevant variables without the need for human intervention, obtained better performance measures. Most of the studies used SVMs, supervised classifiers operating by finding the optimal decision boundary to distinguish two classes in a dataset, which can be either linear or non-linear. The successful use of SVM is likely driven by the great confidence gained by the field in using this technique as well as the wide availability of fully automatic computer tools for its use. However, it is interesting to note that overall performance (in the case of binary classification) varied from 0.49, which is to be considered very low (i.e., noise), to over 0.90. These results are fully justified by different factors, some of which may be attributable to the preprocessing of the data, the wide variety of the data, and the a-priori setting of hyperparameters (parameters not learned during the training phase of the methodology but set by the architect of the software https://doi.org/10.3934/mine.2023012).
Conclusions
As a discipline, psychiatry suffers from some main challenges: first, there is a lack of biological markers of disease and prognosis, second, there is a large heterogeneity in clinical presentation, treatment response, and progression, and third, most of research studies, with a very selected and neat population, do not always translate into real-world practice. Thus, even ML shows a limited accuracy despite having a great potential. While DL techniques would not be able to provide any insights into the psychopathology of psychosis, they might unveil a pattern, by using large and various sources of data (biological, clinical, passive data from wearable electronic devices on patients, EHRs) not based on epistemological assumptions. This will allow a better understanding of the disease and provide useful tools to personalize both identification and treatment.
Abbreviations
- AI:
-
Artificial intelligence
- ANN:
-
Artificial neural networks
- AUC:
-
Area under curve
- BD:
-
Bipolar disorder
- CHR-P:
-
Clinical high risk for psychosis
- DL:
-
Deep learning
- EEG:
-
Electroencephalography
- EHRs:
-
Electronic health records
- FEP:
-
First episode psychosis
- ML:
-
Machine learning
- MMP:
-
Multiple multilayer perceptron
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PCA:
-
Principal component analysis
- PPV:
-
Positive predictive value
- RBF:
-
Radial basis function
- RF:
-
Random forest
- SCZ:
-
Schizophrenia
- SVM:
-
Support vector machine
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bhugra D. The global prevalence of schizophrenia. PLoS Medicine. 2005;2(5):e151.
World Health Organization. Schizophrenia. 2019 [cited 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia.
Simon GE. Social and economic burden of mood disorders. Biol Psychiat. 2003;54(3):208–15.
Robinson DG, et al. Predictors of hospitalization of individuals with first-episode psychosis: data from a 2-year follow-up of the RAISE-ETP. Psychiatr Serv. 2019;70(7):569–77.
Melle I, et al. Early detection of the first episode of schizophrenia and suicidal behavior. Am J Psychiatry. 2006;163(5):800–4.
Jaaskelainen E, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296–306.
Nordentoft M, et al. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. 2013;8(1):e55176.
Malla A, McGorry P. Early intervention in psychosis in young people: a population and public health perspective. Am J Public Health. 2019;109(S3):S181–4.
Birchwood M, Fiorillo A. The critical period for early intervention. Psychiatr Rehabil Ski. 2000;4(2):182–98.
Birchwood M, Todd P, Jackson C. Early intervention in psychosis. The critical period hypothesis. Br J Psychiatry Suppl. 1998;172(33):53–9.
Correll CU, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiat. 2018;75(6):555–65.
Lieberman JA, Small SA, Girgis RR. Early detection and preventive intervention in schizophrenia: from fantasy to reality. Am J Psychiatr. 2019;176(10):794–810.
Pollard JM, Ferrara M, Lin IH, Kucukgoncu S, Wasser T, Li F, Srihari VH. Analysis of early intervention services on adult judicial outcomes. JAMA Psychiatr. 2020;77(8):871–2.
Ferrara M, Guloksuz S, Mathis WS, Li F, Lin I, Syed S, Gallagher K, Shah J, Kline E, Tek C, Keshavan M. First help-seeking attempt before and after psychosis onset: measures of delay and aversive pathways to care. Soc Psychiatry Psychiatr Epidemiol. 2021;56(8):1359–69.
Ten Velden HW, et al. Early detection, early symptom progression and symptomatic remission after ten years in a first episode of psychosis study. Schizophr Res. 2013;143(2–3):337–43.
Powers AR, et al. Duration of the psychosis prodrome. Schizophr Res. 2020;216:443–9.
Sykes LA, Ferrara M, Addington J, Bearden CE, Cadenhead KS, Cannon TD, Cornblatt BA, Perkins DO, Mathalon DH, Seidman LJ, Tsuang MT. Predictive validity of conversion from the clinical high risk syndrome to frank psychosis. 2020;216:184–91.
Cannon TD, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65(1):28–37.
Fusar-Poli P, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69(3):220–9.
De Pablo GS, Catalan A, Fusar-Poli P. Clinical validity of DSM-5 attenuated psychosis syndrome: advances in diagnosis, prognosis, and treatment. JAMA Psychiatry. 2020;77(3):311–20.
van Os J, Guloksuz S. A critique of the “ultra‐high risk” and “transition” paradigm. World Psychiatry. 2017;16(2):200–6.
Gifford G, et al. Using neuroimaging to help predict the onset of psychosis. Neuroimage. 2017;145:209–17.
Hunter SA, Lawrie SM. Imaging and genetic biomarkers predicting transition to psychosis. Curr Top Behav Neurosci. 2018;40:353–88.
Mirzakhanian H, Singh F, Cadenhead KS. Biomarkers in psychosis: an approach to early identification and individualized treatment. Biomarkers in medicine. 2014;8(1):51–7.
Mei L, Nave KA. Neuregulin-ERBB signaling in the nervous system and neuropsychiatric diseases. Neuron. 2014;83(1):27–49.
Lencz T, et al. Generalized and specific neurocognitive deficits in prodromal schizophrenia. Biol Psychiatry. 2006;59(9):863–71.
Veronese M, et al. A potential biomarker for treatment stratification in psychosis: evaluation of an [18F] FDOPA PET imaging approach. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2021;46(6):1122–32.
Keshavan MS, Anderson S, Pettergrew JW. Is schizophrenia due to excessive synaptic pruning in the prefrontal cortex? The Feinberg hypothesis revisited. J Psychiatr Res. 1994;28(3):239–65.
Oliver LD, et al. From the group to the individual in schizophrenia spectrum disorders: biomarkers of social cognitive impairments and therapeutic translation. Biol Psychiat. 2022;91(8):699–708.
Walker EF, et al. Cortisol levels and risk for psychosis: initial findings from the North American prodrome longitudinal study. Biol Psychiatry. 2013;74(6):410–7.
Bracher-Smith M, Crawford K, Escott-Price V. Machine learning for genetic prediction of psychiatric disorders: a systematic review. Molecular Psychiatry. 2021;26(1):70–9.
Leighton SP, et al. Development and validation of multivariable prediction models of remission, recovery, and quality of life outcomes in people with first episode psychosis: a machine learning approach. Lancet Digital Health. 2019;1(6):e261–70.
Mechelli A. Machine learning : methods and applications to brain disorders. 1st ed. San Deigo: Elsevier. pages cm; 2019.
Amoretti S, et al. Identifying clinical clusters with distinct trajectories in first-episode psychosis through an unsupervised machine learning technique. Eur Neuropsychopharmacol. 2021;47:112–29.
• Ellis JK, Walker EF, Goldsmith DR. Selective review of neuroimaging findings in youth at clinical high risk for psychosis: on the path to biomarkers for conversion. Front Psychiatry. 2020;11:567534. Review on the characterization of youth at clinical high risk for psychosis with neuroimaging data and machine learning tools applications.
Beaudoin M, et al. Prediction of quality of life in schizophrenia using machine learning models on data from Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial. NPJ Schizophr. 2022;8(1):29.
Cannon TD, et al. An individualized risk calculator for research in prodromal psychosis. Am J Psychiatry. 2016;173(10):980–8.
Koutsouleris N, et al. Multimodal machine learning workflows for prediction of psychosis in patients with clinical high-risk syndromes and recent-onset depression. JAMA Psychiat. 2021;78(2):195–209.
Kwakernaak S, et al. Using machine learning to predict mental healthcare consumption in non-affective psychosis. Schizophr Res. 2020;218:166–72.
Legge SE, et al. Clinical indicators of treatment-resistant psychosis. B J Psych. 2020;216(5):259–66.
Leighton SP, et al. Predicting one-year outcome in first episode psychosis using machine learning. PLoS One. 2019;14(3):e0212846.
• Barros C, Silva CA, Pinheiro AP. Advanced EEG-based learning approaches to predict schizophrenia: Promises and pitfalls. Artif Intell Med. 2021;114:102039. Comprehensive review on ML application on EEG-based data.
Masychev K, et al. Quantitative biomarkers to predict response to clozapine treatment using resting EEG data. Schizophr Res. 2020;223:289–96.
Baradits M, Bitter I, Czobor P. Multivariate patterns of EEG microstate parameters and their role in the discrimination of patients with schizophrenia from healthy controls. Psychiatry Res. 2020;288:112938.
Barros C, et al. From sound perception to automatic detection of schizophrenia: an EEG-based deep learning approach. Front Psychiatry. 2021;12: 813460.
Kim JY, Lee HS, Lee SH. EEG source network for the diagnosis of schizophrenia and the identification of subtypes based on symptom severity—A machine learning approach. J Clin Med. 2020;9(12):3934.
Masychev K, et al. Advanced signal processing methods for characterization of schizophrenia. IEEE Trans Biomed Eng. 2021;68(4):1123–30.
Tikka SK, et al. Artificial intelligence-based classification of schizophrenia: a high density electroencephalographic and support vector machine study. Indian J Psychiatry. 2020;62(3):273–82.
Jang K-I, et al. Machine learning-based electroencephalographic phenotypes of schizophrenia and major depressive disorder. Front Psychiatry. 2021;12: 745458.
Ciprian C, et al. A machine learning approach using effective connectivity to predict response to clozapine treatment. IEEE transactions on neural systems and rehabilitation engineering : a publication of the IEEE Engineering in Medicine and Biology Society. 2020;28(12):2598–607.
Min B, et al. Prediction of individual responses to electroconvulsive therapy in patients with schizophrenia: machine learning analysis of resting-state electroencephalography. Schizophr Res. 2020;216:147–53.
APA 2013 American Psychiatric Association. American Psychiatric Association DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Corcoran CM, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67–75.
Rezaii N, Walker E, Wolff P. A machine learning approach to predicting psychosis using semantic density and latent content analysis. NPJ Schizophr. 2019;5(1):1–12.
Tan EJ, et al. Investigating the diagnostic utility of speech patterns in schizophrenia and their symptom associations. Schizophr Res. 2021;238:91–8.
• De Boer JN, Brederoo SG, Voppel AE, Sommer IE. Anomalies in language as a biomarker for schizophrenia. Current opinion in psychiatry. 2020 May 1;33(3):212–8. Review on the feasibility of using computational linguistic tools paired with ML to analyze language disturbances as a discriminant feature in schizophrenic patients and as a predictor for psychosis development.
Sarzynska-Wawer J, et al. Detecting formal thought disorder by deep contextualized word representations. Psychiatry Res. 2021;304: 114135.
• Ratana R, Sharifzadeh H, Krishnan J, Pang S. A comprehensive review of computational methods for automatic prediction of schizophrenia with insight into indigenous populations. Front Psychiatry. 2019;10:659. Extensive review of the state-of-the-art techniques based on ML within the NLP framework, with a focus on non-Western cultures.
• Corcoran CM, Mittal VA, Bearden CE, Gur RE, Hitczenko K, Bilgrami Z, Savic A, Cecchi GA, Wolff P. Language as a biomarker for psychosis: A natural language processing approach. Schizophr Res. 2020;226:158–66. Review of the emerging possibility of using computational analysis of ecological language to better understand and treat individuals at CHR for psychosis.
De Boer JN, Voppel AE, Brederoo SG, Schnack HG, Truong KP, Wijnen FN, Sommer IE. Acoustic speech markers for schizophrenia-spectrum disorders: a diagnostic and symptom-recognition tool. Psychol Med. 2021:1–11.
Hays R, et al. Deriving symptom networks from digital phenotyping data in serious mental illness. BJPsych Open. 2020;6(6):e135.
Rodriguez-Villa E, et al. Smartphone Health Assessment for Relapse Prevention (SHARP): a digital solution toward global mental health. BJPsych Open. 2021;7(1):e29.
Benoit J, et al. Systematic Review of digital phenotyping and machine learning in psychosis spectrum illnesses. Harv Rev Psychiatry. 2020;28(5):296–304.
Feldman J, Hamlyn A, Rice T. Social media in screening and monitoring for early intervention in psychosis. Schizophr Res. 2021;238:70–2.
Bae YJ, Shim M, Lee WH. Schizophrenia Detection Using Machine Learning Approach from Social Media Content. Sensors. 2021;21(17):5924.
Birnbaum ML, et al. Utilizing machine learning on internet search activity to support the diagnostic process and relapse detection in young individuals with early psychosis: feasibility study. JMIR Mental Health. 2020;7(9):e19348.
Stamate D, et al. Identifying psychosis spectrum disorder from experience sampling data using machine learning approaches. Schizophr Res. 2019;209:156–63.
Mongan D, et al. Development of proteomic prediction models for transition to psychotic disorder in the clinical high-risk state and psychotic experiences in adolescence. JAMA Psychiat. 2021;78(1):77–90.
Rauber S, et al. Cerebrospinal fluid flow cytometry distinguishes psychosis spectrum disorders from differential diagnoses. Mol Psychiatry. 2021;26(12):7661–70.
Pinto JV, et al. Peripheral biomarker signatures of bipolar disorder and schizophrenia: A machine learning approach. Schizophr Res. 2017;188:182–4.
Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21(12):1696–709.
Goodkind M, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiat. 2015;72(4):305–15.
Goetzl EJ, et al. Decreased mitochondrial electron transport proteins and increased complement mediators in plasma neural-derived exosomes of early psychosis. Transl Psychiatry. 2020;10(1):361.
Goetzl EJ, et al. Neural cell-derived plasma exosome protein abnormalities implicate mitochondrial impairment in first episodes of psychosis. FASEB J. 2021;35(2):e21339.
Trakadis YJ, Sardaar S, Chen A, Fulginiti V, Krishnan A. Machine learning in schizophrenia genomics, a case‐control study using 5,090 exomes. Am J Med Genet B Neuropsychiatr. 2019;180(2):103–12.
Vivian-Griffiths T, et al. Predictive modeling of schizophrenia from genomic data: comparison of polygenic risk score with kernel support vector machines approach. Am J Med Genet B Neuropsychiatr Genet. 2019;180(1):80–5.
Escott-Price V, et al. No evidence for enrichment in schizophrenia for common allelic associations at imprinted loci. PLoS One. 2015;10(12):e0144172.
International Schizophrenia C, et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460(7256):748–52.
Zheutlin AB, et al. Multivariate Pattern analysis of genotype–phenotype relationships in schizophrenia. Schizophr Bull. 2018;44(5):1045–52.
Yang H, Liu J, Sui J, Pearlson G, Calhoun VD. A hybrid machine learning method for fusing fMRI and genetic data: combining both improves classification of schizophrenia. Front Human Neurosci. 2010;4:192.
Chen J, et al. Neurobiological divergence of the positive and negative schizophrenia subtypes identified on a new factor structure of psychopathology using non-negative factorization: an international machine learning study. Biol Psychiat. 2020;87(3):282–93.
Chen J, et al. Association of a reproducible epigenetic risk profile for schizophrenia with brain methylation and function. JAMA Psychiat. 2020;77(6):628–36.
Fernandes BS, et al. Precision psychiatry with immunological and cognitive biomarkers: a multi-domain prediction for the diagnosis of bipolar disorder or schizophrenia using machine learning. Transl Psychiatry. 2020;10(1):162.
Phalen H, et al. Non-negative matrix factorization reveals resting-state cortical alpha network abnormalities in the first-episode schizophrenia spectrum. Biol Psychiatry: Cogn Neurosci. 2020;5(10):961–70.
Koutsouleris N, et al. Disease prediction in the at-risk mental state for psychosis using neuroanatomical biomarkers: results from the FePsy study. Schizophr Bull. 2011;38(6):1234–46.
Koutsouleris N, et al. Use of Neuroanatomical pattern classification to identify subjects in at-risk mental states of psychosis and predict disease transition. Arch Gen Psychiatry. 2009;66(7):700–12.
Koutsouleris N, et al. Detecting the Psychosis prodrome across high-risk populations using neuroanatomical biomarkers. Schizophr Bull. 2014;41(2):471–82.
Kambeitz-Ilankovic L, et al. Prediction of outcome in the psychosis prodrome using neuroanatomical pattern classification. Schizophr Res. 2016;173(3):159–65.
Kambeitz J, et al. Detecting neuroimaging biomarkers for schizophrenia: a meta-analysis of multivariate pattern recognition studies. Neuropsychopharmacology. 2015;40(7):1742–51.
Kalmady SV, et al. Towards artificial intelligence in mental health by improving schizophrenia prediction with multiple brain parcellation ensemble-learning. NPJ Schizophr. 2019;5(1):2.
• de Filippis R, Carbone EA, Gaetano R, Bruni A, Pugliese V, Segura-Garcia C, De Fazio P. Machine learning techniques in a structural and functional MRI diagnostic approach in schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2019;15:1605. Extensive study evaluating the use of structural and functional MRI coupled with ML techniques for early diagnosis, treatment response definition, and prognosis of schizophrenic patients.
Pinaya WH, Mechelli A, Sato JR. Using deep autoencoders to identify abnormal brain structural patterns in neuropsychiatric disorders: A large‐scale multi‐sample study. Hum Brain Mapp. 2019;40(3):944–54.
Zhu Y, Nakatani H, Yassin W, Maikusa N, Okada N, Kunimatsu A, Abe O, Kuwabara H, Yamasue H, Kasai K, Okanoya K. Application of a Machine Learning Algorithm for Structural Brain Images in Chronic Schizophrenia to Earlier Clinical Stages of Psychosis and Autism Spectrum Disorder: A Multiprotocol Imaging Dataset Study. Schizophr Bulletin. 2022;48(3):563–74.
Antonucci LA, et al. A pattern of cognitive deficits stratified for genetic and environmental risk reliably classifies patients with schizophrenia from healthy control subjects. Biol Psychiat. 2020;87(8):697–707.
Chang Y-W, et al. Development of an Al-based web diagnostic system for phenotyping psychiatric disorders. Front Psychiatry. 2020;11: 542394.
Cai X-L, et al. Generalizability of machine learning for classification of schizophrenia based on resting-state functional MRI data. Hum Brain Mapp. 2020;41(1):172–84.
Cao B, et al. Treatment response prediction and individualized identification of first-episode drug-naive schizophrenia using brain functional connectivity. Mol Psychiatry. 2020;25(4):906–13.
Cui Y, Li C, Liu B, Sui J, Song M, Chen J, Chen Y, Guo H, Li P, Lu L, Lv L. Consistent brain structural abnormalities and multisite individualised classification of schizophrenia using deep neural networks. Br J Psychiatry. 2022:1–8.
Gutierrez-Gomez L, et al. Stable biomarker identification for predicting schizophrenia in the human connectome. Neuroimage Clin. 2020;27:102316.
Hu K, et al. Multisite schizophrenia classification by integrating structural magnetic resonance imaging data with polygenic risk score. Neuroimage Clin. 2021;32:102860.
Arbabshirani MR, Castro E, Calhoun VD. Accurate classification of schizophrenia patients based on novel resting-state fMRI features. In 2014 36th Annual International Conference of the IEEE Eng Med Bio Soc. IEEE. 2014:6691–4.
Han W, et al. Low-rank network signatures in the triple network separate schizophrenia and major depressive disorder. Neuroimage Clin. 2019;22: 101725.
Zeng LL, et al. Multi-site diagnostic classification of schizophrenia using discriminant deep learning with functional connectivity MRI. EBioMedicine. 2018;30:74–85.
Qureshi MNI, et al. Multimodal discrimination of schizophrenia using hybrid weighted feature concatenation of brain functional connectivity and anatomical features with an extreme learning machine. Front Neuroinform. 2017;11:59.
Li J, et al. Machine learning technique reveals intrinsic characteristics of schizophrenia: an alternative method. Brain Imaging Behav. 2019;13(5):1386–96.
Ramkiran S, Sharma A, Rao NP. Resting-state anticorrelated networks in schizophrenia. Psychiatry Res Neuroimaging. 2019;284:1–8.
Guo W, et al. Using short-range and long-range functional connectivity to identify schizophrenia with a family-based case-control design. Psychiatry Res: Neuroimaging. 2017;264:60–7.
Kottaram A, et al. Predicting individual improvement in schizophrenia symptom severity at 1-year follow-up: comparison of connectomic, structural, and clinical predictors. Hum Brain Mapp. 2020;41(12):3342–57.
Morgan SE, et al. Functional magnetic resonance imaging connectivity accurately distinguishes cases with psychotic disorders from healthy controls, based on cortical features associated with brain network development. Biol Psychiatry: Cogn Neurosci. 2021;6(12):1125–34.
Miotto R, et al. Deep patient: an unsupervised representation to predict the future of patients from the electronic health records. Sci Rep. 2016;6(1):26094.
Simon GE, et al. First presentation with psychotic symptoms in a population-based sample. Psychiatr Serv. 2017;68(5):456–61.
Holderness E, et al. Analysis of risk factor domains in psychosis patient health records. J Biomed Semantics. 2019;10(1):19.
Senior M, Burghart M, Yu R, Kormilitzin A, Liu Q, Vaci N, Nevado-Holgado A, Pandit S, Zlodre J, Fazel S. Identifying Predictors of Suicide in Severe Mental Illness: A Feasibility Study of a Clinical Prediction Rule (Ox ford M ental I llness and S uicide Tool or OxMIS). Front Psychiatry. 2020;11:268.
Mourao-Miranda J, et al. Individualized prediction of illness course at the first psychotic episode: a support vector machine MRI study. Psychol Med. 2012;42(5):1037–47.
Santesteban-Echarri O, et al. Predictors of functional recovery in first-episode psychosis: a systematic review and meta-analysis of longitudinal studies. Clin Psychol Rev. 2017;58:59–75.
de Nijs J, Burger TJ, Janssen RJ, Kia SM, van Opstal DP, de Koning MB, de Haan L, Cahn W, Schnack HG. Individualized prediction of three-and six-year outcomes of psychosis in a longitudinal multicenter study: a machine learning approach. NPJ Schizophr. 2021;7(1):1–11.
Correll CU, et al. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiat. 2017;74(7):675–84.
Martinuzzi E, et al. Stratification and prediction of remission in first-episode psychosis patients: the OPTiMiSE cohort study. Transl Psychiatry. 2019;9(1):20.
Kapur S, Phillips AG, Insel TR. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol Psychiatry. 2012;17(12):1174–9.
Meltzer HY, et al. Neuropsychologic deficits in schizophrenia: relation to social function and effect of antipsychotic drug treatment. Neuropsychopharmacology. 1996;14(3 Suppl):27S-33S.
Korda AI, Andreou C, Borgwardt S. Pattern classification as decision support tool in antipsychotic treatment algorithms. Exp Neurol. 2021;339:113635.
Sarpal DK, et al. Baseline striatal functional connectivity as a predictor of response to antipsychotic drug treatment. Am J Psychiatry. 2016;173(1):69–77.
Fonseca de Freitas D, Kadra-Scalzo G, Agbedjro D, Francis E, Ridler I, Pritchard M, Shetty H, Segev A, Casetta C, Smart SE, Downs J. Using a statistical learning approach to identify sociodemographic and clinical predictors of response to clozapine. J Psychopharmacol. 2022;36(4):498–506.
Ciprian C, et al. A machine learning approach using effective connectivity to predict response to clozapine treatment. IEEE Trans Neural Syst Rehabil Eng. 2020;28(12):2598–607.
Pisanu C, Squassina A. Treatment-resistant schizophrenia: insights from genetic studies and machine learning approaches. 2019;10.
Pence AY, et al. Gender differences in the association between environment and psychosis. Schizophr Res. 2022;243:120–37.
Ferrara M, Srihari VH. Early intervention for psychosis in the United States: Tailoring services to improve care for women. Psychiatr Serv. 2021;72(1):5–6.
Brand BA, de Boer JN, Dazzan P, Sommer IE. Towards better care for women with schizophrenia-spectrum disorders. The Lancet Psychiatry. 2022.
Acknowledgements
The editors would like to thank Dr. Daniel McFarland for taking the time to review this manuscript.
Funding
Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Complex Medical-Psychiatric Issues
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferrara, M., Franchini, G., Funaro, M. et al. Machine Learning and Non-Affective Psychosis: Identification, Differential Diagnosis, and Treatment. Curr Psychiatry Rep 24, 925–936 (2022). https://doi.org/10.1007/s11920-022-01399-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-022-01399-0