Abstract
Purpose of Review
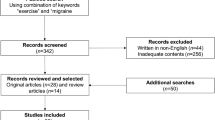
This review aimed to investigate emerging evidence regarding the effectiveness of exercise for migraines, focusing on the results of recent trials. Additionally, it explored the possibility of exercise as a treatment for migraines.
Recent Findings
Between 2020 and 2023, five, four, one, and two trials were conducted regarding the effect of aerobic exercise, anaerobic exercise, Tai Chi, and yoga, respectively, on migraine; all studies showed significant effects. Two trials on aerobic exercise showed that high-intensity exercise was similar to or slightly more effective than moderate-intensity exercise as a treatment for migraines. Three trials on anaerobic exercise reported its effectiveness in preventing migraines.
Summary
Regarding efficacy, side effects, and health benefits, aerobic exercises and yoga are potentially beneficial strategies for the prevention of migraines. Further studies are needed to develop evidence-based exercise programs for the treatment of migraines.

Similar content being viewed by others
Data Availability
Data generated in this study is available from the corresponding author upon request.
Abbreviations
- AE:
-
Aerobic exercise
- AMIT:
-
Amitriptyline
- BAI:
-
Beck Anxiety Index
- BDI:
-
Beck Depression Index
- CCT:
-
Controlled clinical trial
- CM:
-
Chronic migraine
- CMSE:
-
Craniocervical muscle-strengthening exercise
- CTTH:
-
Chronic tension type headache
- DB + J:
-
Diaphragmatic breathing and jogging
- EM:
-
Episodic migraine
- EME + J:
-
Eye movement exercise and jogging
- HIIT:
-
High-intensity interval training
- HIT:
-
High-intensity training
- HIT-6:
-
Headache Impact Test-6
- HR:
-
Heart rate
- MCT:
-
Moderate-intensity continuous training
- MIDAS:
-
Migraine Disability Assessment Test
- MIT:
-
Moderate-intensity training
- NOS:
-
Newcastle–Ottawa Scale
- OR:
-
Odds ratio
- PRISMA:
-
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomized controlled trial
- SD:
-
Standard deviation
- SMD:
-
Standardized mean difference
- Supp:
-
Supplements
- TTH:
-
Tension type headache
- VD:
-
Vitamin D supplements
References
Papers of particular interest and those published recently have been highlighted as follows: • Of importance •• Of major importance
Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018;19(1):17. https://doi.org/10.1186/s10194-018-0846-2.
Becker WJ, Findlay T, Moga C, Scott NA, Harstall C, Taenzer P. Guideline for primary care management of headache in adults. Can Fam Physician. 2015;61(8):670–9.
Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache. 2015;55(1):3–20. https://doi.org/10.1111/head.12499.
Bigal ME, Lipton RB. The epidemiology, burden, and comorbidities of migraine. Neurol Clin. 2009;27(2):321–34. https://doi.org/10.1016/j.ncl.2008.11.011.
Buse DC, Manack A, Serrano D, Turkel C, Lipton RB. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry. 2010;81(4):428–32. https://doi.org/10.1136/jnnp.2009.192492.
Scher AI, Bigal ME, Lipton RB. Comorbidity of migraine. Curr Opin Neurol. 2005;18(3):305–10. https://doi.org/10.1097/01.wco.0000169750.52406.a2.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Daenen L, Varkey E, Kellmann M, Nijs J. Exercise, not to exercise, or how to exercise in patients with chronic pain? Applying science to practice. Clin J Pain. 2015;31(2):108–14. https://doi.org/10.1097/ajp.0000000000000099.
Häuser W, Klose P, Langhorst J, Moradi B, Steinbach M, Schiltenwolf M, et al. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther. 2010;12(3):R79. https://doi.org/10.1186/ar3002.
Dinler M, Diracoglu D, Kasikcioglu E, Sayli O, Akin A, Aksoy C, et al. Effect of aerobic exercise training on oxygen uptake and kinetics in patients with fibromyalgia. Rheumatol Int. 2009;30(2):281–4. https://doi.org/10.1007/s00296-009-1126-x.
Hoffman MD, Shepanski MA, Mackenzie SP, Clifford PS. Experimentally induced pain perception is acutely reduced by aerobic exercise in people with chronic low back pain. J Rehabil Res Dev. 2005;42(2):183–90. https://doi.org/10.1682/jrrd.2004.06.0065.
Song TJ, Chu MK. Exercise in Treatment of Migraine Including Chronic Migraine. Curr Pain Headache Rep. 2021;25(3):14. https://doi.org/10.1007/s11916-020-00929-w.
Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev. 2022;18(2): e1230. https://doi.org/10.1002/cl2.1230.
Oliveira AB, Ribeiro RT, Mello MT, Tufik S, Peres MFP. Anandamide Is Related to Clinical and Cardiorespiratory Benefits of Aerobic Exercise Training in Migraine Patients: A Randomized Controlled Clinical Trial. Cannabis Cannabinoid Res. 2019;4(4):275–84. https://doi.org/10.1089/can.2018.0057.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 2 Feb 2024.
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane. 2023.
Bond DS, Thomas JG, Lipton RB, Roth J, Pavlovic JM, Rathier L, et al. Behavioral Weight Loss Intervention for Migraine: A Randomized Controlled Trial. Obesity (Silver Spring). 2018;26(1):81–7. https://doi.org/10.1002/oby.22069.
Darabaneanu S, Overath CH, Rubin D, Lüthje S, Sye W, Niederberger U, et al. Aerobic exercise as a therapy option for migraine: a pilot study. Int J Sports Med. 2011;32(6):455–60. https://doi.org/10.1055/s-0030-1269928.
Dittrich SM, Günther V, Franz G, Burtscher M, Holzner B, Kopp M. Aerobic exercise with relaxation: influence on pain and psychological well-being in female migraine patients. Clin J Sport Med. 2008;18(4):363–5. https://doi.org/10.1097/JSM.0b013e31817efac9.
•• Hanssen H, Minghetti A, Magon S, Rossmeissl A, Rasenack M, Papadopoulou A, et al. Effects of different endurance exercise modalities on migraine days and cerebrovascular health in episodic migraineurs: A randomized controlled trial. Scand J Med Sci Sports. 2018;28(3):1103–12. https://doi.org/10.1111/sms.13023. This was the first clinical trial to observe the effect of high-intensity aerobic exercise on the prevention of migraine.
Krøll LS, Hammarlund CS, Linde M, Gard G, Jensen RH. The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial. Cephalalgia. 2018;38(12):1805–16. https://doi.org/10.1177/0333102417752119.
Narin SO, Pinar L, Erbas D, Oztürk V, Idiman F. The effects of exercise and exercise-related changes in blood nitric oxide level on migraine headache. Clin Rehabil. 2003;17(6):624–30. https://doi.org/10.1191/0269215503cr657oa.
Santiago MD, Carvalho Dde S, Gabbai AA, Pinto MM, Moutran AR, Villa TR. Amitriptyline and aerobic exercise or amitriptyline alone in the treatment of chronic migraine: a randomized comparative study. Arq Neuropsiquiatr. 2014;72(11):851–5. https://doi.org/10.1590/0004-282x20140148.
Varkey E, Cider A, Carlsson J, Linde M. Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31(14):1428–38. https://doi.org/10.1177/0333102411419681.
Amin FM, Aristeidou S, Baraldi C, Czapinska-Ciepiela EK, Ariadni DD, Di Lenola D, et al. The association between migraine and physical exercise. J Headache Pain. 2018;19(1):83. https://doi.org/10.1186/s10194-018-0902-y.
Lemmens J, De Pauw J, Van Soom T, Michiels S, Versijpt J, van Breda E, et al. The effect of aerobic exercise on the number of migraine days, duration and pain intensity in migraine: a systematic literature review and meta-analysis. J Headache Pain. 2019;20(1):16. https://doi.org/10.1186/s10194-019-0961-8.
Broman-Fulks JJ, Storey KM. Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety Stress Coping. 2008;21(2):117–28. https://doi.org/10.1080/10615800701762675.
Broocks A, Bandelow B, Pekrun G, George A, Meyer T, Bartmann U, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603–9. https://doi.org/10.1176/ajp.155.5.603.
Carmeli E, Barak S, Morad M, Kodesh E. Physical exercises can reduce anxiety and improve quality of life among adults with intellectual disability : original research article. International SportMed Journal. 2009;10(2):77–85. https://doi.org/10.10520/EJC48373.
Goldin P, Ziv M, Jazaieri H, Gross JJ. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Front Hum Neurosci. 2012;6:295. https://doi.org/10.3389/fnhum.2012.00295.
Kim SH, Schneider SM, Bevans M, Kravitz L, Mermier C, Qualls C, et al. PTSD symptom reduction with mindfulness-based stretching and deep breathing exercise: randomized controlled clinical trial of efficacy. J Clin Endocrinol Metab. 2013;98(7):2984–92. https://doi.org/10.1210/jc.2012-3742.
Oldridge N, Guyatt G, Jones N, Crowe J, Singer J, Feeny D, et al. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am J Cardiol. 1991;67(13):1084–9. https://doi.org/10.1016/0002-9149(91)90870-q.
Smits JA, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depress Anxiety. 2008;25(8):689–99. https://doi.org/10.1002/da.20411.
Villaverde Gutiérrez C, Torres Luque G, Ábalos Medina GM, Argente del Castillo MJ, Guisado IM, Guisado Barrilao R, et al. Influence of exercise on mood in postmenopausal women. J Clin Nurs. 2012;21(7–8):923–8. https://doi.org/10.1111/j.1365-2702.2011.03972.x.
Wedekind D, Broocks A, Weiss N, Engel K, Neubert K, Bandelow B. A randomized, controlled trial of aerobic exercise in combination with paroxetine in the treatment of panic disorder. World J Biol Psychiatry. 2010;11(7):904–13. https://doi.org/10.3109/15622975.2010.489620.
Hovland A, Nordhus IH, Sjøbø T, Gjestad BA, Birknes B, Martinsen EW, et al. Comparing physical exercise in groups to group cognitive behaviour therapy for the treatment of panic disorder in a randomized controlled trial. Behav Cogn Psychother. 2013;41(4):408–32. https://doi.org/10.1017/s1352465812000446.
Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587–96. https://doi.org/10.1097/PSY.0b013e318148c19a.
Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159(19):2349–56. https://doi.org/10.1001/archinte.159.19.2349.
Blumenthal JA, Sherwood A, Babyak MA, Watkins LL, Smith PJ, Hoffman BM, et al. Exercise and pharmacological treatment of depressive symptoms in patients with coronary heart disease: results from the UPBEAT (Understanding the Prognostic Benefits of Exercise and Antidepressant Therapy) study. J Am Coll Cardiol. 2012;60(12):1053–63. https://doi.org/10.1016/j.jacc.2012.04.040.
Doyne EJ, Ossip-Klein DJ, Bowman ED, Osborn KM, McDougall-Wilson IB, Neimeyer RA. Running versus weight lifting in the treatment of depression. J Consult Clin Psychol. 1987;55(5):748–54. https://doi.org/10.1037/0022-006x.55.5.748.
Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8. https://doi.org/10.1016/j.amepre.2004.09.003.
Epstein D. Aerobic Activity Versus Group Cognitive Therapy: An Evaluative Study of Contrasting Interventions for the Alleviation of Clinical Depression. Reno: University of Nevada; 1986.
Foley LS, Prapavessis H, Osuch EA, De Pace JA, Murphy BA, Podolinsky NJ. An examination of potential mechanisms for exercise as a treatment for depression: A pilot study. Ment Health Phys Act. 2008;1(2):69–73. https://doi.org/10.1016/j.mhpa.2008.07.001.
Hemat-Far A, Shahsavari A, Mousavi SR. Effects of Selected Aerobic Exercises on the Depression and Concentrations of Plasma Serotonin in the Depressed Female Students Aged 18 to 25. J Appl Res Clin Exp Ther. 2012;12:47–52.
Klein MH, Greist JH, Gurman AS, Neimeyer RA, Lesser DP, Bushnell NJ, et al. A comparative outcome study of group psychotherapy vs. exercise treatments for depression. International Journal of Mental Health. 1984;13(3/4):148–76.
Krogh J, Saltin B, Gluud C, Nordentoft M. The DEMO trial: a randomized, parallel-group, observer-blinded clinical trial of strength versus aerobic versus relaxation training for patients with mild to moderate depression. J Clin Psychiatry. 2009;70(6):790–800. https://doi.org/10.4088/jcp.08m04241.
Krogh J, Videbech P, Thomsen C, Gluud C, Nordentoft M. DEMO-II trial. Aerobic exercise versus stretching exercise in patients with major depression-a randomised clinical trial. PLoS One. 2012;7(10):316. https://doi.org/10.1371/journal.pone.0048316.
Martinsen EW, Hoffart A, Solberg Ø. Comparing aerobic with nonaerobic forms of exercise in the treatment of clinical depression: A randomized trial. Compr Psychiatry. 1989;30(4):324–31. https://doi.org/10.1016/0010-440X(89)90057-6.
Mota-Pereira J, Silverio J, Carvalho S, Ribeiro JC, Fonte D, Ramos J. Moderate exercise improves depression parameters in treatment-resistant patients with major depressive disorder. J Psychiatr Res. 2011;45(8):1005–11. https://doi.org/10.1016/j.jpsychires.2011.02.005.
Mutrie N. Exercise as a Treatment for Depression within a National Health Service (antidepressant, aerobic exercise, general practioner). United States -- Pennsylvania: The Pennsylvania State University. 1986. p. 188.
Pinchasov BB, Shurgaja AM, Grischin OV, Putilov AA. Mood and energy regulation in seasonal and non-seasonal depression before and after midday treatment with physical exercise or bright light. Psychiatry Res. 2000;94(1):29–42. https://doi.org/10.1016/s0165-1781(00)00138-4.
Salehi I, Hosseini SM, Haghighi M, Jahangard L, Bajoghli H, Gerber M, et al. Electroconvulsive therapy and aerobic exercise training increased BDNF and ameliorated depressive symptoms in patients suffering from treatment-resistant major depressive disorder. J Psychiatr Res. 2014;57:117–24. https://doi.org/10.1016/j.jpsychires.2014.06.018.
Veale D, Le Fevre K, Pantelis C, de Souza V, Mann A, Sargeant A. Aerobic exercise in the adjunctive treatment of depression: a randomized controlled trial. J R Soc Med. 1992;85(9):541–4. https://doi.org/10.1177/014107689208500910.
Chen LJ, Fox KR, Ku PW, Chang YW. Effects of Aquatic Exercise on Sleep in Older Adults with Mild Sleep Impairment: a Randomized Controlled Trial. Int J Behav Med. 2016;23(4):501–6. https://doi.org/10.1007/s12529-015-9492-0.
Elavsky S, McAuley E. Lack of perceived sleep improvement after 4-month structured exercise programs. Menopause. 2007;14(3 Pt 1):535–40. https://doi.org/10.1097/01.gme.0000243568.70946.d4.
Karimi S, Soroush A, Towhidi F, Makhsosi BR, Karimi M, Jamehshorani S, et al. Surveying the effects of an exercise program on the sleep quality of elderly males. Clin Interv Aging. 2016;11:997–1002. https://doi.org/10.2147/cia.S106808.
King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial Jama. 1997;277(1):32–7.
King AC, Pruitt LA, Woo S, Castro CM, Ahn DK, Vitiello MV, et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J Gerontol A Biol Sci Med Sci. 2008;63(9):997–1004. https://doi.org/10.1093/gerona/63.9.997.
Oudegeest-Sander MH, Eijsvogels TH, Verheggen RJ, Poelkens F, Hopman MT, Jones H, et al. Impact of physical fitness and daily energy expenditure on sleep efficiency in young and older humans. Gerontology. 2013;59(1):8–16. https://doi.org/10.1159/000342213.
Sternfeld B, Guthrie KA, Ensrud KE, LaCroix AZ, Larson JC, Dunn AL, et al. Efficacy of exercise for menopausal symptoms: a randomized controlled trial. Menopause. 2014;21(4):330–8. https://doi.org/10.1097/GME.0b013e31829e4089.
Tadayon M, Abedi P, Farshadbakht F. Impact of pedometer-based walking on menopausal women’s sleep quality: a randomized controlled trial. Climacteric. 2016;19(4):364–8. https://doi.org/10.3109/13697137.2015.1123240.
Tan X, Alén M, Wiklund P, Partinen M, Cheng S. Effects of aerobic exercise on home-based sleep among overweight and obese men with chronic insomnia symptoms: a randomized controlled trial. Sleep Med. 2016;25:113–21. https://doi.org/10.1016/j.sleep.2016.02.010.
Alipouri M, Amiri E, Hoseini R, Hezarkhani LA. Effects of eight weeks of aerobic exercise and vitamin D supplementation on psychiatric comorbidities in men with migraine and vitamin D insufficiency: A randomized controlled clinical trial. J Affect Disord. 2023;334:12–20. https://doi.org/10.1016/j.jad.2023.04.108.
Eslami R, Parnow A, Pairo Z, Nikolaidis P, Knechtle B. The effects of two different intensities of aerobic training protocols on pain and serum neuro-biomarkers in women migraineurs: a randomized controlled trail. Eur J Appl Physiol. 2021;121(2):609–20. https://doi.org/10.1007/s00421-020-04551-x.
Malek EM, Navalta JW, McGinnis GR. Time of day and chronotype-dependent synchrony effects exercise-induced reduction in migraine load: a pilot cross-over randomized trial. Int J Environ Res Public Health. 2023. https://doi.org/10.3390/ijerph20032083.
• Matin H, Taghian F, Chitsaz A. Artificial intelligence analysis to explore synchronize exercise, cobalamin, and magnesium as new actors to therapeutic of migraine symptoms: a randomized, placebo-controlled trial. Neurol Sci. 2022;43(7):4413–24. https://doi.org/10.1007/s10072-021-05843-6. This recent clinical trial observed that high-intensity interval training was effective in preventive treatment of migraine.
Rahimi MD, Hassani P, Kheirkhah MT, Fadardi JS. Effectiveness of eye movement exercise and diaphragmatic breathing with jogging in reducing migraine symptoms: A preliminary, randomized comparison trial. Brain Behav. 2023;13(1):e2820. https://doi.org/10.1002/brb3.2820.
La Touche R, Fierro-Marrero J, Sánchez-Ruíz I, Rodríguez de Rivera-Romero B, Cabrera-López CD, Lerma-Lara S, et al. Prescription of therapeutic exercise in migraine, an evidence-based clinical practice guideline. J Headache Pain. 2023;24(1):68. https://doi.org/10.1186/s10194-023-01571-8.
Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142(9):765–75. https://doi.org/10.7326/0003-4819-142-9-200505030-00013.
Herring MP, Jacob ML, Suveg C, O’Connor PJ. Effects of short-term exercise training on signs and symptoms of generalized anxiety disorder. Ment Health Phys Act. 2011;4(2):71–7. https://doi.org/10.1016/j.mhpa.2011.07.002.
Pilu A, Sorba M, Hardoy MC, Floris AL, Mannu F, Seruis ML, et al. Efficacy of physical activity in the adjunctive treatment of major depressive disorders: preliminary results. Clin Pract Epidemiol Ment Health. 2007;3:8. https://doi.org/10.1186/1745-0179-3-8.
Sims J, Galea M, Taylor N, Dodd K, Jespersen S, Joubert L, et al. Regenerate: assessing the feasibility of a strength-training program to enhance the physical and mental health of chronic post stroke patients with depression. Int J Geriatr Psychiatry. 2009;24(1):76–83. https://doi.org/10.1002/gps.2082.
Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of progressive resistance training in depressed elders. J Gerontol A Biol Sci Med Sci. 1997;52(1):M27-35. https://doi.org/10.1093/gerona/52a.1.m27.
Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, Fiatarone Singh MA. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol A Biol Sci Med Sci. 2005;60(6):768–76. https://doi.org/10.1093/gerona/60.6.768.
• Aslani P, Hassanpour M, Razi O, Knechtle B, Parnow A. Resistance Training Reduces Pain Indices and Improves Quality of Life and Body Strength in Women with Migraine Disorders. 2021. This is the first clinical trial to report the effectiveness of resistance traning, an anaerobic exercise, as a preventive treatment for migraine.
• Benatto MT, Florencio LL, Bragatto MM, Dach F, Fernández-de-Las-Peñas C, Bevilaqua-Grossi D. Neck-specific strengthening exercise compared with placebo sham ultrasound in patients with migraine: a randomized controlled trial. BMC Neurol. 2022;22(1):126. https://doi.org/10.1186/s12883-022-02650-0. This study is the first to report the migraine prevention effect of specific neck tanning, another anaerobic exercise.
Rinne M, Garam S, Kukkonen-Harjula K, Tokola K, Häkkinen A, Ylinen J, et al. Neck-Shoulder Region Training for Chronic Headache in Women: A Randomized Controlled Trial. Clin Rehabil. 2023;37(10):1322–31. https://doi.org/10.1177/02692155231170687.
Sun L, Li G, Liu F, Wang Y, Zhang L, Minoret C. Resistance exercise relieves symptoms of vestibular migraine patients with MRI diagnosis: A randomized parallel-controlled single-blind clinical trial. Rev Neurol (Paris). 2022;178(4):370–6. https://doi.org/10.1016/j.neurol.2021.06.008.
•• Woldeamanuel YW, Oliveira ABD. What is the efficacy of aerobic exercise versus strength training in the treatment of migraine? A systematic review and network meta-analysis of clinical trials. J Headache Pain. 2022;23(1):134. https://doi.org/10.1186/s10194-022-01503-y. This recent meta-analysis observed that high-intensity aerobic exercise had efficacy similar to moderate-intensity aerobic exercise as a preventive treatment for migraine.
Boroujeni MZ, Marandi SM, Esfarjani F, Sattar M, Shaygannejad V, Javanmard SH. Yoga intervention on blood NO in female migraineurs. Adv Biomed Res. 2015;4:259. https://doi.org/10.4103/2277-9175.172995.
John PJ, Sharma N, Sharma CM, Kankane A. Effectiveness of yoga therapy in the treatment of migraine without aura: a randomized controlled trial. Headache. 2007;47(5):654–61. https://doi.org/10.1111/j.1526-4610.2007.00789.x.
Kisan R, Sujan M, Adoor M, Rao R, Nalini A, Kutty BM, et al. Effect of Yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int J Yoga. 2014;7(2):126–32. https://doi.org/10.4103/0973-6131.133891.
Sharma VM, Manjunath NK, Nagendra HR, Ertsey C. Combination of Ayurveda and Yoga therapy reduces pain intensity and improves quality of life in patients with migraine headache. Complement Ther Clin Pract. 2018;32:85–91. https://doi.org/10.1016/j.ctcp.2018.05.010.
Cramer H, Lauche R, Anheyer D, Pilkington K, de Manincor M, Dobos G, et al. Yoga for anxiety: A systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2018;35(9):830–43. https://doi.org/10.1002/da.22762.
Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013;30(11):1068–83. https://doi.org/10.1002/da.22166.
Wang WL, Chen KH, Pan YC, Yang SN, Chan YY. The effect of yoga on sleep quality and insomnia in women with sleep problems: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):195. https://doi.org/10.1186/s12888-020-02566-4.
Kumar A, Bhatia R, Sharma G, Dhanlika D, Vishnubhatla S, Singh RK, et al. Effect of yoga as add-on therapy in migraine (CONTAIN): A randomized clinical trial. Neurology. 2020;94(21):e2203–12. https://doi.org/10.1212/wnl.0000000000009473.
Mehta JN, Parikh S, Desai SD, Solanki RC, A GP. Study of Additive Effect of Yoga and Physical Therapies to Standard Pharmacologic Treatment in Migraine. J Neurosci Rural Pract. 2021;12(1):60–6. https://doi.org/10.1055/s-0040-1718842.
Xie YJ, Tian L, Hui SS, Qin J, Gao Y, Zhang D, et al. Efficacy and feasibility of a 12-week Tai Chi training for the prophylaxis of episodic migraine in Hong Kong Chinese women: A randomized controlled trial. Front Public Health. 2022;10:1000594. https://doi.org/10.3389/fpubh.2022.1000594.
Funding
This research was supported by a grant from the Korea Health Technology Research and Development Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant no.: HV22C0106), and a National Research Foundation of Korea grant from the Korean government (Ministry of Science and Information and Communication Technology) (grant no.: 2022R1A2C1091767). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
WSH conceptualized and designed the study, analyzed the data, and drafted the manuscript. MKC conceptualized and designed the study; collected, analyzed, and interpreted the data; and reviewed the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
MKC was the site investigator for a multicenter trial sponsored by Biohaven Pharmaceuticals, Allergan Korea, and the Ildong Pharmaceutical Company, has received lecture honoraria from Eli Lilly and Company, Handok-Teva, and the Ildong Pharmaceutical Company over the past 24 months, and has received grants from the Yonsei University College of Medicine (6–2021-0229), the Korea Health Industry Development Institute (KHIDI) (HV22C0106), and an NRF grant from the Korean government (MSIT) (2022R1A2C1091767). WSH has no conflicts of interest to declare.
Human and Animal Rights and Informed Consent
All reported studies and experiments involving humans or animals performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ha, WS., Chu, M.K. Advances in Exercise in the Clinical Trials of Migraine: A Scoping Review. Curr Pain Headache Rep (2024). https://doi.org/10.1007/s11916-024-01269-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-024-01269-9