Abstract
Purpose of Review
To summarize recent findings regarding triptan use in the acute treatment of pediatric migraine.
Recent Findings
Prevalence of pediatric migraine is rising. The American Headache Society and American Academy of Neurology updated guidelines to provide evidence-based recommendations for the treatment of acute migraine in youth. In the setting of a dearth of new randomized controlled trials (RCTs), we review current guidelines, triptan use in the emergency department, and an era of secondary analyses.
Summary
Measuring the efficacy of triptans in pediatric migraine has been challenged by high placebo response rates. Secondary analyses, combining data from multiple RCTs, support that triptans are safe and effective in the treatment of migraine. Triptans are a vital tool and the only FDA-approved migraine-specific treatment available in pediatrics. There is a need for further studies and funding support in pediatric headache medicine.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Onofri A, Pensato U, Rosignoli C, et al. Primary headache epidemiology in children and adolescents: a systematic review and meta-analysis. J Headache Pain. 2023;24(1):8. https://doi.org/10.1186/s10194-023-01541-0.
Nieswand V, Richter M, Gossrau G. Epidemiology of headache in children and adolescents-another type of pandemia. Curr Pain Headache Rep. 2020;24(10):62. https://doi.org/10.1007/s11916-020-00892-6.
Lateef TM, Merikangas KR, He J, et al. Headache in a national sample of American children: prevalence and comorbidity. J Child Neurol. 2009;24(5):536–43. https://doi.org/10.1177/0883073808327831.
Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol. 2010;52(12):1088–97. https://doi.org/10.1111/j.1469-8749.2010.03793.x.
Yang Y, Cao Y. Rising trends in the burden of migraine and tension-type headache among adolescents and young adults globally, 1990 to 2019. J Headache Pain. 2023;24(1):94. https://doi.org/10.1186/s10194-023-01634-w.
Orr SL, Kabbouche MA, O’Brien HL, Kacperski J, Powers SW, Hershey AD. Paediatric migraine: evidence-based management and future directions. Nat Rev Neurol. 2018;14(9):515–27. https://doi.org/10.1038/s41582-018-0042-7.
Leung S, Bulloch B, Young C, et al. Effectiveness of standardized combination therapy for migraine treatment in the pediatric emergency department. Headache. 2013;53(3):171–7. https://doi.org/10.1111/head.12042.
Falla K, Kuziek J, Mahnaz SR, Noel M, Ronksley PE, Orr SL. Anxiety and depressive symptoms and disorders in children and adolescents with migraine: a systematic review and meta-analysis. JAMA Pediatr. 2022;176(12):1176–87. https://doi.org/10.1001/jamapediatrics.2022.3940.
Powers SW, Coffey CS, Chamberlin LA, et al. Prevalence of headache days and disability 3 years after participation in the childhood and adolescent migraine prevention medication trial. JAMA Netw Open. 2021;4(7):1–14. https://doi.org/10.1001/jamanetworkopen.2021.14712.
Canfora M, Pallotto IK, Davis JK, et al. More than a headache: lived experience of migraine in youth. Pediatr Neurol. 2023;146:79–84. https://doi.org/10.1016/j.pediatrneurol.2023.05.019.
Abu-Arafeh I. Headache and psychological comorbidities: an appraisal of the evidence. J Clin Med. 2023;12(7). https://doi.org/10.3390/jcm12072683.
Brainstorm Consortium, Anttila V, Bulik-Sullivan B, et al. Analysis of shared heritability in common disorders of the brain. Science. 2018;360(6395):eaap8757. https://doi.org/10.1126/science.aap8757.
Stovner LJ, Nichols E, Steiner TJ, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–76. https://doi.org/10.1016/S1474-4422(18)30322-3.
Wöber-Bingöl C. Epidemiology of migraine and headache in children and adolescents. Curr Pain Headache Rep. 2013;17(6):341. https://doi.org/10.1007/s11916-013-0341-z.
Perry MC, Yaeger SK, Toto RL, Suresh S, Hickey RW. A modern epidemic: increasing pediatric emergency department visits and admissions for headache. Pediatr Neurol. 2018;89:19–25. https://doi.org/10.1016/j.pediatrneurol.2018.07.015.
Gelfand AA, Goadsby PJ. Treatment of pediatric migraine in the emergency room. Pediatr Neurol. 2012;47(4):233–41. https://doi.org/10.1016/j.pediatrneurol.2012.06.001.
Raucci U, Della Vecchia N, Ossella C, et al. Management of childhood headache in the emergency department. Review of the literature. Front Neurol. 2019;10:886. https://doi.org/10.3389/fneur.2019.00886. Published 2019 Aug 23.
Dooley JM, Augustine HF, Brna PM, Digby AM. The prognosis of pediatric headaches - A 30-year follow-up study. Pediatr Neurol. 2014;51(1):85–7. https://doi.org/10.1016/j.pediatrneurol.2014.02.022.
Galinski M, Sidhoum S, Cimerman P, Perrin O, Annequin D, Tourniaire B. Early diagnosis of migraine necessary in children: 10-year follow-up. Pediatr Neurol. 2015;53(4):319–23. https://doi.org/10.1016/j.pediatrneurol.2015.05.013.
Orr SL, Shapiro RE. The elephant in the room: How the underfunding of headache research stunts the field. Headache. 2022;62(9):1234–8. https://doi.org/10.1111/head.14396.
Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine. Drugs. 2000;60(6):1259–87. https://doi.org/10.2165/00003495-200060060-00003.
Humphrey PPA. The discovery and development of the triptans, a major therapeutic breakthrough. Headache. 2008;48(5):685–7. https://doi.org/10.1111/J.1526-4610.2008.01097.X.
Ahn AH, Basbaum AI. Where do triptans act in the treatment of migraine? Pain. 2005;115(1–2):1–4. https://doi.org/10.1016/j.pain.2005.03.008.
Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol. 1993;33(1):48–56. https://doi.org/10.1002/ana.410330109.
Juhasz G, Zsombok T, Jakab B, Nemeth J, Szolcsanyi J, Bagdy G. Sumatriptan causes parallel decrease in plasma calcitonin gene-related peptide (CGRP) concentration and migraine headache during nitroglycerin induced migraine attack. Cephalalgia. 2005;25(3):179–83. https://doi.org/10.1111/J.1468-2982.2005.00836.X.
Puledda F, Silva EM, Suwanlaong K, Goadsby PJ. Migraine: from pathophysiology to treatment. J Neurol. 2023;270(7):3654–66. https://doi.org/10.1007/s00415-023-11706-1.
Vila-Pueyo M. Targeted 5-HT1F therapies for migraine. Neurotherapeutics. 2018;15(2):291–303. https://doi.org/10.1007/S13311-018-0615-6.
Goadsby PJ, Akerman S, Storer RJ. Evidence for postjunctional serotonin (5-HT1) receptors in the trigeminocervical complex. Ann Neurol. 2001;50(6):804–7. https://doi.org/10.1002/ana.10066.
Wiggers A, Ashina H, Hadjikhani N, et al. Brain barriers and their potential role in migraine pathophysiology. J Headache Pain. 2022;23(1):1–10. https://doi.org/10.1186/s10194-021-01365-w.
Pleș H, Florian IA, Timis TL, et al. Migraine: advances in the pathogenesis and treatment. Neurol Int. 2023;15(3):1052–105. https://doi.org/10.3390/neurolint15030067.
Humphrey PPA, Feniuk W, Perren MJ, Connor HE, Oxford AW. The pharmacology of the novel 5-HT1-like receptor agonist, GR43175. Cephalalgia. 1989;9(SUPPL. 9):23–33. https://doi.org/10.1111/J.1468-2982.1989.TB00069.X.
Humphrey PPA. 5-Hydroxytryptamine and the pathophysiology of migraine. J Neurol. 1991;238(1 Supplement). https://doi.org/10.1007/BF01642905.
Humphrey PP, Feniuk W, Perren MJ, et al. GR43175, a selective agonist for the 5-HT1-like receptor in dog isolated saphenous vein. Br J Pharmacol. 1988;94(4):1123–32. https://doi.org/10.1111/j.1476-5381.1988.tb11630.x.
Pini LA, Brovia D. Different characteristics of triptans. J Headache Pain. 2004;5(SUPPL. 2). https://doi.org/10.1007/s10194-004-0122-5.
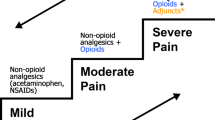
•• Oskoui M, Pringsheim T, Holler-Managan Y, et al. Practice guideline update summary: acute treatment of migraine in children and adolescents: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2019;93:487–99. https://doi.org/10.1212/WNL.0000000000008095. Updated guidelines on acute care, thoughtful systematic review, and endorsed by the American Academy of Pediatrics and Child Neurology Society.
Endorsement SOF. Acute treatment of migraine in children and adolescents. Pediatrics. 2019;144(5):20192762. https://doi.org/10.1542/peds.2019-2762.
Practice guideline update: acute treatment of migraine in children and adolescents. https://www.aan.com/Guidelines/home/GuidelineDetail/966. Accessed 30 Jan 2024.
Olesen J. Headache Classification Committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. https://doi.org/10.1177/0333102417738202.
Dodick D, Lipton RB, Martin V, et al. Consensus statement: Cardiovascular safety profile of triptans (5-HT 1B/1D agonists) in the acute treatment of migraine. Headache. 2004;44(5):414–25. https://doi.org/10.1111/j.1526-4610.2004.04078.x.
GlaxoSmithKline. Imitrex Tablets (Sumatriptan succinate) [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2013. www.fda.gov/medwatch.
Maxalt Tablets (Rizatriptan Benzoate). [package insert]. Whitehouse Station, NJ: Merck & Co. Inc; 2007
Hershey AD. Current approaches to the diagnosis and management of paediatric migraine. Lancet Neurol. 2010;9(2):190–204. https://doi.org/10.1016/S1474-4422(09)70303-5.
Stovner LJ, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210. https://doi.org/10.1111/J.1468-2982.2007.01288.X.
Lewis DW, Winner P, Wasiewski W. The placebo responder rate in children and adolescents. Headache. 2005;45(3):232–9. https://doi.org/10.1111/j.1526-4610.2005.05050.x.
Ho TW, Fan X, Rodgers A, Lines CR, Winner P, Shapiro RE. Age effects on placebo response rates in clinical trials of acute agents for migraine: Pooled analysis of rizatriptan trials in adults. Cephalalgia. 2009;29(7):711–8. https://doi.org/10.1111/j.1468-2982.2008.01788.x.
• Chanchlani R, Agrawal A, Janjua D, Hafsa SN. The efficacy of different triptans for the treatment of acute headache in pediatric migraine: a systematic review. Indian Pediatr. 2023;60:663–71. Most recent systematic review incorporating most recent studies on triptans in pediatric migraine.
Sun H, Bastings E, Temeck J, et al. Migraine therapeutics in adolescents: a systematic analysis and historic perspectives of triptan trials in adolescents. JAMA Pediatr. 2013;167(3):243–9. https://doi.org/10.1001/jamapediatrics.2013.872.
Rothner AD, Wasiewski W, Winner P, Lewis D, Stankowski J. Zolmitriptan oral tablet in migraine treatment: high placebo responses in adolescents. Headache. 2006;46(1):101–9. https://doi.org/10.1111/J.1526-4610.2006.00313.X.
Bendtsen L, Mattsson P, Zwart JA, Lipton RB. Placebo response in clinical randomized trials of analgesics in migraine. Cephalalgia. 2003;23(7):487–90. https://doi.org/10.1046/j.1468-2982.2003.00528.x.
Winner P, Lewis D, Visser WH, et al. Rizatriptan 5 mg for the acute treatment of migraine in adolescents: a randomized, double-blind, placebo-controlled study. Headache. 2002;42(1):49–55. https://doi.org/10.1046/j.1526-4610.2002.02013.x.
Wang G, Tan T, Liu Y, Hong P. Drugs for acute attack of pediatric migraine: a network meta-analysis of randomized controlled trials. Clin Neurol Neurosurg. 2020;195:105853. https://doi.org/10.1016/j.clineuro.2020.105853.
Evers S. The efficacy of triptans in childhood and adolescence migraine. Curr Pain Headache Rep. 2013;17(7):342. https://doi.org/10.1007/s11916-013-0342-y.
Wöber-Bingöl Ç. Pharmacological treatment of acute migraine in adolescents and children. Pediatric Drugs. 2013;15(3):235–46. https://doi.org/10.1007/s40272-013-0019-3.
Richer L, Billinghurst L, Linsdell MA, et al. Drugs for the acute treatment of migraine in children and adolescents. Cochrane Database Syst Rev. 2016;4(4):CD005220. https://doi.org/10.1002/14651858.CD005220.pub2.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed). 2008;336(7650):924–6. https://doi.org/10.1136/bmj.39489.470347.AD.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:4–10. https://doi.org/10.1136/bmj.i4919.
AAN (American Academy of Neurology). Clinical practice guideline process manual. 2011th ed. St. Paul, MN: The American Academy of Neurology; 2011.
Hong P, Wu X, Liu Y. Calcitonin gene-related peptide monoclonal antibody for preventive treatment of episodic migraine: a meta analysis. Clin Neurol Neurosurg. 2017;154:74–8. https://doi.org/10.1016/j.clineuro.2017.01.009.
•• Yonker ME, McVige J, Zeitlin L, Visser H. A multicenter, randomized, double-blind, placebo-controlled, crossover trial to evaluate the efficacy and safety of zolmitriptan nasal spray for the acute treatment of migraine in patients aged 6 to 11 years, with an open-label extension. Headache. 2022;62(9):1207–17. https://doi.org/10.1111/head.14391. First trial in children 6–11 to study zolmitriptan. Notable findings include evidence for headache relief with zolmitriptan in children 6-11, although this was a secondary endpoint and no statistical different found in primary outcome of pain freedom influenced by early termination with slow enrollment during COVID-19 pandemic.
Bachur RG, Monuteaux MC, Neuman MI. A comparison of acute treatment regimens for migraine in the emergency department. Pediatrics. 2015;135(2):232–8. https://doi.org/10.1542/peds.2014-2432.
Richer LP, Laycock K, Millar K, et al. Treatment of children with migraine in emergency departments: national practice variation study. Pediatrics. 2010;126(1):e150–5. https://doi.org/10.1542/PEDS.2009-2337.
Legault G, Eisman H, Shevell MI. Treatment of pediatric status migrainosus: can we prevent the “bounce back.” J Child Neurol. 2011;26(8):949–55. https://doi.org/10.1177/0883073810397631.
Trottier ED, Bailey B, Lucas N, Lortie A. Prochlorperazine in children with migraine: a look at its effectiveness and rate of akathisia. Am J Emerg Med. 2012;30(3):456–63. https://doi.org/10.1016/j.ajem.2010.12.020.
• Genadry KC, Monuteaux MC, Neuman MI, Lowe DA, Lee LK. Disparities and trends in migraine management in pediatric emergency departments, 2009–19. Acad Pediatr. 2022. https://doi.org/10.1016/j.acap.2022.04.007. Most recent investigation of trends of medication use for the treatment of migraine in pediatric emergency departments.
Akpunonu BE, Mutgi AB, Federman DJ, et al. Subcutaneous sumatriptan for treatment of acute migraine in patients admitted to the emergency department: a multicenter study. Ann Emerg Med. 1995;25(4):464–9. https://doi.org/10.1016/s0196-0644(95)70259-8.
Meredith JT, Wait S, Brewer KL. A prospective double-blind study of nasal sumatriptan versus IV ketorolac in migraine. Am J Emerg Med. 2003;21(3):173–5. https://doi.org/10.1016/S0735-6757(02)42256-5.
• Hauser Chatterjee J, Hartford EA, Law E, Barry D, Blume H. Sumatriptan as a first-line treatment for headache in the pediatric emergency department. Pediatr Neurol. 2023;142:68–75. https://doi.org/10.1016/j.pediatrneurol.2023.01.016. Retrospective study summarizing single-center experience using triptan in the pediatric emergency department. Results suggest there may be a reduced need for IV management, shorter length of stays, and decrease in charges with IN sumatriptan as a first line treatment in the ED.
Yang CP, Liang CS, Chang CM, et al. Comparison of new pharmacologic agents with triptans for treatment of migraine: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(10):1–15. https://doi.org/10.1001/jamanetworkopen.2021.28544.
Curran MP, Evans HC, Wagstaff AJ. Intranasal sumatriptan: in adolescents with migraine. CNS Drugs. 2005;19(4):335–6. https://doi.org/10.2165/00023210-200519040-00006.
Lindkvist J, Airaksinen M, Kaukonen AM, Klaukka T, Hoppu K. Evolution of paediatric off-label use after new significant medicines become available for adults: a study on triptans in Finnish children 1994–2007. Br J Clin Pharmacol. 2011;71(6):929–35. https://doi.org/10.1111/j.1365-2125.2010.03881.x.
Johnson A, Bickel J, Lebel A. Pediatric migraine prescription patterns at a large academic hospital. Pediatr Neurol. 2014;51(5):706–12. https://doi.org/10.1016/j.pediatrneurol.2014.06.018.
Lai LL, Koh L, Ho JAC, Ting A, Obi A. Off-label prescribing for children with migraines in U.S. ambulatory care settings. J Manag Care Spec Pharm. 2017;23(3):382–7. https://doi.org/10.18553/JMCP.2017.23.3.382.
Winner P, Rothner AD, Saper J, et al. A randomized, double-blind, placebo-controlled study of sumatriptan nasal spray in the treatment of acute migraine in adolescents. Pediatrics. 2000;106(5):989–97. https://doi.org/10.1542/peds.106.5.989.
Winner P, Rothner AD, Wooten JD, et al. Sumatriptan nasal spray in adolescent migraineurs: A randomized, double-blind, placebo-controlled, acute study. Headache. 2006;46(2):212–22. https://doi.org/10.1111/j.1526-4610.2006.00339.x.
Ahonen K, Hämäläinen ML, Rantala H, Hoppu K. Nasal sumatriptan is effective in treatment of migraine attacks in children: a randomized trial. Neurology. 2004;62(6):883–7. https://doi.org/10.1212/01.wnl.0000115105.05966.a7.
Sacco S, Lampl C, Amin FM, et al. European Headache Federation (EHF) consensus on the definition of effective treatment of a migraine attack and of triptan failure. J Headache Pain. 2022;23(1):1–10. https://doi.org/10.1186/s10194-022-01502-z.
Vanderpluym JH, Victorio MCC, Oakley CB, Rastogi RG, Orr SL. Beyond the guidelines: a narrative review of treatments on the horizon for migraine in children and adolescents. Neurology. 2023;101(18):788–97. https://doi.org/10.1212/WNL.0000000000207677.
Olesen A, Schytz HW, Ostrowski SR, et al. Low adherence to the guideline for the acute treatment of migraine. Sci Rep. 2022;12(1):8487. https://doi.org/10.1038/s41598-022-12545-2.
Szperka C. Headache in children and adolescents. CONTINUUM Lifelong Learn Neurol. 2021;27(3):703–31. https://doi.org/10.1212/CON.0000000000000993.
US Food and Drug Administration. Pediatric research equity act of 2003. Public Law. 2017;108155. https://congress.gov/108/plaws/publ155/PLAW-108publ155.pdf. Accessed 20 Dec 2023.
Author information
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chatterjee, J.H., Blume, H.K. Triptans in the Acute Migraine Management of Children and Adolescents: An Update. Curr Pain Headache Rep (2024). https://doi.org/10.1007/s11916-024-01213-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-024-01213-x