Abstract
Purpose of Review
Genomic analyses have immensely advanced our conception of the heterogeneity of diffuse large B cell lymphoma (DLBCL), resulting in subgroups with distinct molecular profiles. In this review, we summarize our current knowledge of the biology of DLBCL complexity and discuss the potential implications for precision medicine.
Recent Findings
During the last two decades, gene expression profiling, copy number analysis, and high throughput sequencing enabled the identification of molecular subclasses of DLBCL that are biologically and clinically meaningful. The resulting classifications provided novel prospects of diagnosis, prognostication, and therapeutic strategies for this aggressive disease.
Summary
The molecular characterization of DLBCL offers unprecedented insights into the biology of these lymphomas that can guide precision medicine. The knowledge of the molecular setup of an individual DLBCL patients enables prognostication of patients and will be useful to stratify patients in clinical trials. Future direction should focus to implement the molecular classifications of DLBCL in the clinical practice to evaluate their significance and scope using real-world data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse large B cell lymphoma (DLBCL) is the most common type of B cell non-Hodgkin lymphoma [1]. This aggressive lymphoma has a high clinical heterogeneity manifesting in diverse responses to rituximab plus chemotherapy (R-CHOP). Early prognostic stratification of DLBCL was developed almost 30 years ago by Shipp and colleagues by combining several clinical parameters to divide patients into risk groups [2]. The resulting International Prognostic Index (IPI) has become the most commonly used prognostic score for aggressive lymphomas [2,3,4]. The first classification of DLBCL based on molecular traits dates back 20 years, when Alizadeh et al. analyzed 96 samples of normal and malignant lymphocytes by gene expression profiling (GEP) using DNA microarrays. This hallmark study identified two subtypes of DLBCL that were distinguished by the expression of genes typical for normal germinal center B cells or activated blood B cells prompting the cell-of-origin classification into ABC and GCB DLBCL [5]. Notably, 10–15% of DLBCL cannot be categorized into one of the two groups and are therefore termed unclassified DLBCL. Importantly, this gene expression-based concept was able to define prognostic categories, which allowed the identification of high-risk disease independently from the IPI. In the R-CHOP era, several GEP studies confirmed the prognostic impact and showed that ABC DLBCL encompass the highest risk for relapse and an inferior outcome [6, 7]. Consequentially, the 2016 revision of the World Health Organization classification of lymphoid neoplasms requires the identification of molecular subgroups of DLBCL [1].
In the recent past our knowledge of the biology and heterogeneity of DLBCL advanced enormously by the application of genomic technologies for high throughput analysis. Several mutations and other structural changes in the cancer genome have been characterized that can serve as diagnostic and prognostic markers. In this review, we will summarize our knowledge of the biology underlying the heterogeneity of DLBCL and illustrate how the classification of DLBCL subgroups using comprehensive molecular characterization can enhance diagnosis and prognostication of this aggressive lymphoma.
Biology of the Cell-of-Origin Classification
Gene expression profiling using DNA microarrays represents one of the earliest technologies for genomic high throughput analysis. About 20 years ago, this technique was used to characterize the abundance of transcripts of several thousand genes in subsets of normal B cells and DLBCL samples [5]. This comparison identified a group of DLBCL that express genes characteristic for normal germinal center (GC) B cells and a group of DLBCL that resembled in their gene expression program blood B cells activated by engagement of B cell receptor and stimulated with varying combination of CD40 ligand and IL4. Thus, due to the similarities of the gene expression profiles of these tumor to normal B cells, the two subgroups have been termed germinal center B cell like (GCB) and activated B cell like (ABC) DLBCL [5].
The gene expression patterns observed in a proportion of samples do not allow a classification of these lymphomas into the ABC or GCB subgroup. These cases are consequently designated as unclassified DLBCL, which is why unclassified DLBCL are often mistaken for a distinct, third group defined by gene expression. However, these cases represent an aggregation of cases that do not fit the model distinguishing ABC and GCB DLBCL [8]. Notably, recent analysis indicated that a substantial number of unclassified DLBCL bear a distinctive signature of mutations and structural gene aberration indicating the existence of a molecular subgroup within unclassified DLBCL (see below).
Gene expression analysis offers a view into tumor phenotypes. These phenotypes are dictated by the accumulation of genetic and epigenetic lesions in the course of malignant transformation of a normal B cell into an aggressive lymphoma. Studies investigating the tumor genome of DLBCL validated this concept identifying several genetic lesions that are restricted to either subtype [9,10,11,12,13,14,15, 16••]. Frequent genetic alterations that are almost exclusively found in GCB DLBCL are chromosomal translocations of the BCL2 locus, oncogenic mutations in the EZH2 gene, amplification of the REL locus and mutations or deletions in PTEN [9,10,11, 17]. While loss of function of PTEN activates the PI3 kinase (PI3K) pathway, increased expression of REL due to amplification likely contributes to the GC B cell phenotype of GCB DLBCL as REL was found to be required for GC maintenance [18]. Likewise, the EZH2 protein, a subunit of the polycomb repressive complex, is involved in germinal center B cell biology. This gene that is required for GC formation contributes to the phenotype of GC B cells by repressing proliferation checkpoint genes and establishing bivalent chromatin domains thereby enabling a lineage specific (i.e., GC B cell) gene expression program [19, 20]. The oncogenic translocation t(14;18) leads to the transcriptional deregulation of BCL2 gene, positioning the coding exons next to regulatory elements of the immunoglobulin heavy chain locus [21]. Interestingly, although BCL2 translocations are almost exclusively found in GCB DLBCL, ABC tumors express high level of BCL2 transcripts, indicating other pathogenetic mechanisms e.g. amplification of the BCL2 locus observed in approximately 30% of ABC DLBCL [22, 23]. Other genetic events characteristic for ABC DLBCL involve components of the B cell receptor (CD79A and CD79B) and regulators of the NF-κB pathway (MYD88) [12, 13]. Recent studies revealed that both mutations collaborate in forming a multiprotein complex that promotes the constitutive activation of the NF-κB transcription factor complex through chronic B cell receptor (BCR) signaling [24, 25]. The central relevance of the BCR signaling in the biology of ABC DLBCL, explains the phenotype of activated B cells and further validates the biologic concept of the cell-of-origin classification.
Clinical Significance of the Cell-of-Origin Classification
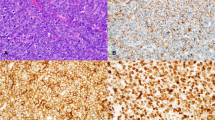
The initial classification of DLBCL based on gene expression profiling revealed a significant survival difference between the subgroups, indicating an inferior outcome for patients with ABC DLBCL versus GCB DLBCL. Unclassified cases showed an intermediate survival rate [5, 8, 23]. These results prompted several investigations as to how the cell-of-origin classification could be implemented in clinical practice using techniques widely available in routine diagnostics. Hence, alternative methods using immunohistochemical markers as surrogates for the expression programs distinguishing DLBCL subgroups have been developed [26,27,28,29]. The method that became the most widely accepted was described by Hans and colleagues, classifying DLBCL by immunohistochemistry staining of CD10, BCL6, and MUM1 into a GCB and a non-GCB subgroup. However, besides variable concordance to gene expression profiling for the tested algorithms, these methods showed highly variable results for interlaboratory comparisons [26, 28, 30,31,32]. To overcome these issues, Scott and colleagues presented a novel, commercially available assay for subclassification based on gene expression of 20 genes that is applicable to formalin-fixed paraffin-embedded tissue [31]. Tests of the Lymph2Cx assay showed high concordance when compared to gene expression profiling (GEP) using DNA microarray analysis on RNA derived from frozen DLBCL biopsies.
Given its major biological and clinical significance, several clinical trials integrated the cell-of-origin classification [33,34,35,36,37]. While some studies confirmed the survival difference observed for patients with ABC, GCB, or UC DLBCL [33, 34], other analyses achieved varying results. In 2013, a UK trial observed no survival differences of patients treated with R-CHOP using the immunohistochemistry based classifier [35]. However, a subsequent reanalysis with microarray-based subclassification revealed that the ABC subtype of DLBCL is independently associated with inferior survival than GCB DLBCL [36]. In 2017, the Lymph2Cx assay was used to classify more than 400 DLBCL patients from two German clinical trials treated chemotherapy and/or immunochemotherapy [37]. While the cell-of-origin classification disclosed prognostic subgroups in patients treated with CHOP, no such survival difference was observed for R-CHOP–treated patients. The stark contrast of these results and the conclusions from population-based studies might be explained by different patient cohorts analyzed [38]. Although rigorously supervised, patient enrolled in randomized controlled trials might not always fully represent the overall patient population and have a lower risk profile than real-world populations [39].
Risk Stratification Using Structural Genetic Lesions: High Grade B Cell Lymphoma
The majority of recurrent genetic alterations in DLBCL differs significantly in their prevalence in ABC and GCB DLBCL, suggesting that the biological and clinical phenotype of DLBCL can be dictated by genetic variants. Chromosomal translocations juxtaposing the oncogenes MYC, BCL2, or BCL6 and one of the immunoglobulin loci are hallmarks in the genesis of lymphomas [21]. Thus, several studies investigated whether these structural aberrations could serve as biomarkers for DLBCL prognostication. MYC rearrangements occur in approximately 10% in DLBCL [40•]. In contrast to Burkitt lymphoma (BL), where MYC is almost exclusively fused to an immunoglobulin locus, up to 50% of MYC translocations in DLBCL involve non-immunoglobulin genes, including among others BCL6, PAX5, and IKZF1 [41, 42]. Several studies indicated that a translocation of MYC is a strong adverse prognostic factor demonstrating an inferior overall (OS) and progression free survival (PFS) compared to patients without MYC rearrangement [43,44,45]. A recent study resolved the role of MYC rearrangements as a biomarker for predicting outcome of DLBCL. The negative prognostic impact of MYC rearrangements in DLBCL is largely observed in patients with translocations of MYC in combination with BCL2 and/or BCL6 in which MYC is translocated to an IG partner [40•]. Co-occurrence of rearrangements of MYC and BCL2 and/or BCL6 translocations was reported in 2–8% of all DLBCL including patients from clinical trials and a population-based registries [40•, 46]. These so-called “double-hit” or “triple-hit” (DH/TH) lymphomas have been included in the 2016 updated WHO classification in the new category of high-grade B cell lymphoma (HGBL) with rearrangements of MYC and BCL2 and/or BCL6 [1]. HGBL-DH/TH lymphoma primarily have a GCB DLBCL phenotype, perhaps not surprising given that BCL2 translocations are almost exclusively found in GCB DLBCL [46].
Two recent studies extended the definition of HGBL using gene expression profiling to identify DLBCL with inferior prognosis beyond the survival distinctions associated with the cell-of-origin classification [47••, 48••]. The study by Sha et al. used a gene expression signature composed of genes highly expressed in BL compared to DLBCL to define cases of molecular HGBL. Whereas, Ennishi et al. focused on GCB DLBCL to develop a signature derived from genes differentially expressed between MYC/BCL2 double-hit and non-double-hit GCB-DLBCLs. Notably, both signatures were capable of identifying most double-hit lymphomas. However, about half of the DLBCL from the identified the high risk group did not harbor gene rearrangements of MYC and BCL2, suggesting the existence of alternative genetic or epigenetic alterations causing a high-grade lymphoma phenotype.
A number of studies have indicated that patients with DLBCL that lack MYC and BCL2 rearrangements, but have high expression of both MYC and BCL2 proteins have an inferior outcome [37, 45, 49]. These so called double expressor (DE) DLBCL are primarily found to be of ABC DLBCL phenotype, suggesting alternative mechanisms responsible for upregulation of BCL2 and MYC protein expression (e.g., chromosomal amplification of the gene BCL2 locus or the activation of the NF-κB pathway) [24]. Compared to HGBL-DH DLBCL, DE-DLBCL have a better overall survival with R-CHOP therapy. Variable clinical outcomes have been reported for DE-DLBCL when compared to non-DE DLBCL. While in elderly patients DE-DLBCL status versus non-DE DLBCL was associated with inferior prognosis [37], other studies did not confirm a prognostic significance of this classification [50], including studies investigating a survival difference in young patients [51], and in patients with stage I/II DLBCL [52].
Genetic Subclasses of DLBCL
The molecular classification of DLBCL based on phenotypic features such as characteristic gene expression signatures or specific chromosomal translocations deconstructed some heterogeneity of clinical outcome. However, while some of the designated high-risk patients are cured, other patients with a predicted positive prognosis succumb to the disease, indicating that these models do not fully account for the heterogeneous responses to chemotherapy. These considerations provided the rationale for multiplatform genomic analyses integrating DNA copy number alterations, chromosomal translocations, recurrent mutations and gene expression profiling that resulted in a novel genetic subclassification of this disease. Remarkably, two independent studies presented a very similar genetic taxonomy although largely distinct mathematic algorithms were used to group DLBCL tumors into genetic subtypes [16••, 53••].
To distinguish molecular subtypes Chapuy and colleagues analyzed 304 DLBCL biopsies to identify candidate cancer driver genes. To this end, the study combined algorithms that classify mutations occurring more often than expected by chance (MutSigCV), mathematical models that identify clustering of missense mutations in 3-dimensional protein structures (CLUMPS), and a model to identify significant copy number variants and structural aberrations [54,55,56]. Using clustering of the 158 identified genetic driver alterations resulted in five clusters, termed C1–C5, each with a discrete genetic signature, as well as a cluster without any detectable alterations [53••]. In contrast, the parallel genomic DLBCL analysis classified 574 tumors into genetic subtypes using the GenClass algorithm that starts with an initial set of genetic aberrations and then iteratively examines all possibly re-assortments of cases into classes to optimize for genetic distinctiveness [16••]. The genetic alterations that define the seed classes of this taxonomy were significantly more prevalent in either ABC, GCB, or unclassified DLBCL. This approach distinguished four genetic subtypes, termed MCD, BN2, N1, and EZB. This terminology refers to the seed alterations that define the genetic subgroups: MYD88L265P and CD79B mutations in MCD, BCL6 translocations and NOTCH2 mutations in BN2, NOTCH1 mutations in N1, and EZH2 mutations and BCL2 translocations in EZB. A subsequent study extending the GenClass algorithm on genomic data from more than 1200 DLBCL added two novel genetic subclasses [57••]: A53 defined by cases with TP53 inactivation associated with aneuploidy and the ST2 subgroup for tumors characterized by the seed class harboring mutations in SGK1 and TET2. The two different algorithmic models used (i.e. consensus clustering and GenClass) resulted in genetic subgroups that had similar genetic signatures (Table 1). Remarkably, both classifications revealed that DLBCL patients subdivided into molecular groups had significantly different clinical outcomes, highlighting that this novel molecular taxonomy is biologically and clinically meaningful [16••, 53••].
The MCD genetic subtype (and its corresponding cluster C5) is primarily composed of ABC DLBCL. Within ABC DLBCL, MCD subtypes had significantly inferior survival as compared with other genetic subgroups or with patients with ABC tumors that were not genetically classified due to lack of sufficient distinguishing genetic events. Genetic hallmarks of the MCD subtype are MYD88L265P and CD79B mutations, which cooperatively activate NF-κB signaling [25]. Tumors of this subtype frequently delete the CDKN2A locus, which encodes the cell cycle inhibitor p16, which likely accelerates proliferation in MCD tumors [56]. Frequent chromosomal amplification of the BCL2 locus induces upregulation of this anti-apoptotic protein contributing to the sustained viability. About 7 out of 10 MCD DLBCL harbor genetic aberrations affecting one or more genes encoding immune regulators, which enables immune evasion. These genetic lesion include inactivation of MHC class I genes, inhibiting MHC class antigen presentation, gene fusions that elevate expression of CD274 and PDCD1LG2 (encoding PD-L1 and PD-L2) thereby decreasing T cell activation, and mutations and deletions of CD58, causing diminished NK cell activation [58]. A number of genetic alterations that define the MCD genetic subtype are also recurrently mutated in primary extranodal lymphomas originating in the CNS, skin, testis, breast and intravascular space [57••]. Interestingly, many MCD DLBCL (as well as C5 cases) are associated with extranodal involvement, affecting particularly the CNS and testis [16••, 53••, 57••]. The CNS and the testis are classical sites of immunologic privilege, raising the possibility that the tropism of MCD tumors to these sites is one mechanism of escape from immunologic surveillance that is amplified by the acquisition of genetic lesions affecting immune recognition (Table 1).
The A53 subtype (and the corresponding cluster C2) is characterized by mutations and deletions of TP53. A53 tumors also frequently inactivate TP53BP1, which encodes a sensor of DNA damage that synergizes with p53 to suppress genomic instability [59]. Interestingly, lymphomas of this genetic subtype harbor gains and losses of multiple chromosomal regions, including copy number changes of the whole arm of various chromosomes. Focal deletions target the tumor suppressors TP73, a p53 family member, and ING1, a component of the p53 signaling pathway [60]. The A53 subtype is enriched for homozygous deletions and truncating mutations targeting the MHC class I subunit, B2M, providing a mechanism of escape from immune surveillance [58]. The A53 genetic subtype is dominated by ABC DLBCL. Compared with tumors of this molecular subclass, A53 had an inferior survival than the BN2 group, but no significant survival difference to MCD or N1 was observed (Table 1).
The least prevalent subtype, N1, which does not have an equivalent in the molecular classification using consensus clustering, is characterized by gain-of-function NOTCH1 mutations that remove all or part of the C-terminal PEST domain. These NOTCH1 variants appear to have similar function to those observed in chronic lymphocytic leukemia and mantle cell lymphoma, but are distinct from the membrane-proximal NOTCH1 mutations in T-cell acute lymphoblastic leukemia [61]. This subtype is almost exclusively comprised of ABC DLBCL. Within this subgroup patients with N1 have significantly inferior survival as compared with patients with BN2 or ABC tumors that were not genetically classified.
The BN2 subtype (and the C1 cluster) is characterized by BCL6 translocations, activating mutations of NOTCH2, and by inactivating of SPEN, a nuclear repressor that antagonizes NOTCH-dependent gene activation. Further prominent genetic features of this subgroup were mutations in genes encoding regulators of B cell receptor (BCR) signaling such as PRKCB and BCL10, as well as inactivating lesions in TNFAIP3 and TNIP1, encoding inhibitors of the NF-κB pathway [62]. BN2 has a relatively equal contributions from unclassified and ABC DLBCL, but also, to lesser extent, from GCB DLBCL. Remarkably, BN2 is the genetic subtype that represents most of the DLBCL that were unclassified by gene expression profiling. Comparing all cases, survival of BN2 was favorable in relation to MCD and N1, but not significantly different to any other genetic subtypes (Table 1). However, when comparing within ABC, BN2 was favorable compared all non-BN2 [57••]. Several mutations characteristic of BN2 subtype occur frequently in marginal zone lymphomas. This includes mutations in NOTCH2 and SPEN, which are involved in differentiation of follicular B cells into marginal zone B cells, as well as aberrations in BCL10, TNFAIP3, and TNIP1 [63].
The ST2 genetic subtype is characterized by mutations in SGK1 and TET2. TET2 is an epigenetic regulatory enzyme that catalyzes the hydroxylation of methylated cytosine residues in DNA. ST2 tumors harbor inactivating mutations in this gene in keeping with its ability to promote germinal centers when disabled in mice [64]. Mutations in SGK1, a kinase in the AKT family that is activated by many cellular responses, likely modulates PI3K signaling in these tumors. Although SGK1 is a target for SHM, preferential acquisition of loss-of-function mutation suggests that it may function as a tumor suppressor in ST2. JAK/STAT signaling is likely the target of several ST2-defining lesions, including inactivation of SOCS1, a negative regulator of JAK signaling as well as activating mutations in STAT3 and inactivation of DUSP2, a phosphatase that controls the activity of STAT3 [65]. The ST2 genetic subtype is predominantly composed of GCB DLBCL. Compared to GCB DLBCL the survival of this subtype is favorable to the EZB group (Table 1).
The genetic subgroup of EZB DLBCL, as well as the corresponding cluster C3, is almost exclusively composed of GCB DLBCL. Consequentially, the defining features of the EZB genetic subgroup are enriched in GCB DLBC, including translocations of BCL2, amplification of the REL locus, inactivation of PTEN, and activating mutations of the histone methyltransferase EZH2. Remarkably, mutations of several other epigenetic regulators such as KMT2D, CREBBP, EP300, and ARID1A are significant features of the genetic signature of this subtype [16••, 53••, 57••]. The perturbation of the epigenetic homeostasis in EZB tumors likely cooperates with mutations in genes encoding factors controlling germinal center B cell development such as IRF8, MEF2B, S1PR2, and GNA13, thus enabling a GC B cell transcriptional profile [66,67,68]. Among GCB cases, EZB had an inferior survival compared with all non-EZB patients.
Predictive Genetic Biomarkers Using Serial Tumor Sampling in Patients with DLBCL
The afore discussed models predicting survival based on the molecular characterization of DLBCL utilize phenotypic and genetic traits available solely at diagnosis. However, recent technical progress enabled the detection of cell-free circulating tumor DNA (ctDNA) that is shed into the blood of lymphoma patients by tumor cells undergoing cell death [69]. This method captures the individual sequence variants of a DLBCL and tracks the specific genetic profile by targeted deep sequencing before, during and after therapy to quantitatively monitor treatment response, clonal evolution, and relapse of this aggressive lymphoma [70, 71, 72•, 73, 74••]. Studies using ctDNA profiling in DLBCL patients receiving immunochemotherapy demonstrated that the highly sensitive quantification of ctDNA level detected in blood of these patients was prognostic of the clinical outcomes [72•]. Notably, patients that showed a substantial decrease in ctDNA quantity after 1 cycle of therapy and/or after 2 cycles had superior outcomes compared to patients, for which a significant decline of ctDNA was not observed. These results prompted a novel survival prediction algorithm for DLBCL patients that integrated IPI, cell-of-origin classification, interim imaging as well as the analysis of pretreatment ctDNA levels and ctDNA decrease after the first and second cycle of therapy [74••]. Importantly, the combined survival prediction significantly improved on the individual risk predictors such as the established risk-factors (i.e., IPI, imaging, cell-of-origin classification). Future analyses combining the risk stratification including ctDNA analysis and genetic subclassification of DLBCL will likely elucidate further biological factors that dictate phenotype and clinical outcome of this aggressive disease.
Conclusions
Over the last two decades, technical advances in genomic analyses allowed deep insights into the biology of DLBCL. In particular, tremendous progress was achieved decoding the vast heterogeneity of this aggressive lymphoma yielding in molecular subclasses that are biologically and clinically meaningful. The profound understanding of the molecular determinants that govern these varying phenotypes will enable the development of precision therapies. While many of these therapeutic strategies will be implemented in the future, the molecular subclassification allows prognostication of the clinical outcome already in current therapeutic settings. With genomics techniques becoming more widely available in clinical routine, the immediate task of next years will be to apply and test the applicable molecular prognostication methods in a real-world setting.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Swerdlow SH, Campo E, Pileri SA, Harris NL, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–90.
International Non-Hodgkin’s Lymphoma Prognostic Factors P. A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 1993;329(14):987–94.
Sehn LH, Berry B, Chhanabhai M, Fitzgerald C, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109(5):1857–61.
Ziepert M, Hasenclever D, Kuhnt E, Glass B, et al. Standard International prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28(14):2373–80.
Alizadeh AA, Eisen MB, Davis RE, Ma C, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403(6769):503–11.
Lenz G, Wright G, Dave SS, Xiao W, et al. Stromal gene signatures in large-B-cell lymphomas. N Engl J Med. 2008;359(22):2313–23.
Roschewski M, Staudt LM, Wilson WH. Diffuse large B-cell lymphoma-treatment approaches in the molecular era. Nat Rev Clin Oncol. 2014;11(1):12–23.
Wright G, Tan B, Rosenwald A, Hurt EH, et al. A gene expression-based method to diagnose clinically distinct subgroups of diffuse large B cell lymphoma. Proc Natl Acad Sci U S A. 2003;100(17):9991–6.
Morin RD, Johnson NA, Severson TM, Mungall AJ, et al. Somatic mutations altering EZH2 (Tyr641) in follicular and diffuse large B-cell lymphomas of germinal-center origin. Nat Genet. 2010;42(2):181–5.
Morin RD, Mendez-Lago M, Mungall AJ, Goya R, et al. Frequent mutation of histone-modifying genes in non-Hodgkin lymphoma. Nature. 2011;476(7360):298–303.
Lenz G, Wright GW, Emre NC, Kohlhammer H, et al. Molecular subtypes of diffuse large B-cell lymphoma arise by distinct genetic pathways. Proc Natl Acad Sci U S A. 2008;105(36):13520–5.
Davis RE, Ngo VN, Lenz G, Tolar P, et al. Chronic active B-cell-receptor signalling in diffuse large B-cell lymphoma. Nature. 2010;463(7277):88–92.
Ngo VN, Young RM, Schmitz R, Jhavar S, et al. Oncogenically active MYD88 mutations in human lymphoma. Nature. 2011;470(7332):115–9.
Pasqualucci L, Trifonov V, Fabbri G, Ma J, et al. Analysis of the coding genome of diffuse large B-cell lymphoma. Nat Genet. 2011;43(9):830–7.
Reddy A, Zhang J, Davis NS, Moffitt AB, et al. Genetic and Functional Drivers of Diffuse Large B Cell Lymphoma. Cell. 2017;171(2):481–494 e15.
Schmitz R, Wright GW, Huang DW, Johnson CA, et al. Genetics and Pathogenesis of Diffuse Large B-Cell Lymphoma. N Engl J Med. 2018;378(15):1396–1407 Multiplatform genomic analysis elucidating the heterogeneity of DLBCL resulting in a genetic taxonomy of DLBCL that provided unexpected biological and clinical insights
Iqbal J, Sanger WG, Horsman DE, Rosenwald A, et al. BCL2 Translocation Defines a Unique Tumor Subset within the Germinal Center B-Cell-Like Diffuse Large B-Cell Lymphoma. Am J Pathol. 2004;165(1):159–66.
Heise N, De Silva NS, Silva K, Carette A, et al. Germinal center B cell maintenance and differentiation are controlled by distinct NF-kappaB transcription factor subunits. J Exp Med. 2014;211(10):2103–18.
Beguelin W, Popovic R, Teater M, Jiang Y, et al. EZH2 is required for germinal center formation and somatic EZH2 mutations promote lymphoid transformation. Cancer Cell. 2013;23(5):677–92.
Beguelin W, Teater M, Gearhart MD, Calvo Fernandez MT, et al. EZH2 and BCL6 cooperate to assemble CBX8-BCOR complex to repress bivalent promoters, mediate germinal center formation and lymphomagenesis. Cancer Cell. 2016;30(2):197–213.
Kuppers R, Dalla-Favera R. Mechanisms of chromosomal translocations in B cell lymphomas. Oncogene. 2001;20(40):5580–94.
Iqbal J, Neppalli VT, Wright G, Dave BJ, et al. BCL2 expression is a prognostic marker for the activated B-cell-like type of diffuse large B-cell lymphoma. J Clin Oncol. 2006;24(6):961–8.
Rosenwald A, Wright G, Chan WC, Connors JM, et al. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med. 2002;346(25):1937–47.
Young RM, Wu T, Schmitz R, Dawood M, et al. Survival of human lymphoma cells requires B-cell receptor engagement by self-antigens. Proc Natl Acad Sci U S A. 2015;112(44):13447–54.
Phelan JD, Young RM, Webster DE, Roulland S, et al. A multiprotein supercomplex controlling oncogenic signalling in lymphoma. Nature. 2018;560(7718):387–91.
Choi WW, Weisenburger DD, Greiner TC, Piris MA, et al. A new immunostain algorithm classifies diffuse large B-cell lymphoma into molecular subtypes with high accuracy. Clin Cancer Res. 2009;15(17):5494–502.
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103(1):275–82.
Meyer PN, Fu K, Greiner TC, Smith LM, et al. Immunohistochemical methods for predicting cell of origin and survival in patients with diffuse large B-cell lymphoma treated with rituximab. J Clin Oncol. 2011;29(2):200–7.
Colomo L, Lopez-Guillermo A, Perales M, Rives S, et al. Clinical impact of the differentiation profile assessed by immunophenotyping in patients with diffuse large B-cell lymphoma. Blood. 2003;101(1):78–84.
de Jong D, Rosenwald A, Chhanabhai M, Gaulard P, et al. Immunohistochemical prognostic markers in diffuse large B-cell lymphoma: validation of tissue microarray as a prerequisite for broad clinical applications–a study from the Lunenburg Lymphoma Biomarker Consortium. J Clin Oncol. 2007;25(7):805–12.
Scott DW, Wright GW, Williams PM, Lih CJ, et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood. 2014;123(8):1214–7.
Gutierrez-Garcia G, Cardesa-Salzmann T, Climent F, Gonzalez-Barca E, et al. Gene-expression profiling and not immunophenotypic algorithms predicts prognosis in patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Blood. 2011;117(18):4836–43.
Vitolo U, Trneny M, Belada D, Burke JM, et al. Obinutuzumab or Rituximab Plus Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone in Previously Untreated Diffuse Large B-Cell Lymphoma. J Clin Oncol. 2017;35(31):3529–37.
Sehn LH, Martelli M, Trneny M, Liu W, et al. A randomized, open-label, Phase III study of obinutuzumab or rituximab plus CHOP in patients with previously untreated diffuse large B-Cell lymphoma: final analysis of GOYA. J Hematol Oncol. 2020;13(1):71.
Cunningham D, Hawkes EA, Jack A, Qian W, et al. Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: a phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet. 2013;381(9880):1817–26.
Gleeson M, Jack A, Cunningham D, Counsell N, et al. The activated B-cell subtype of diffuse large B-cell lymphoma as determined by whole genome expression profiling on paraffin embedded tissue is independently associated with reduced overall and progression free survival in the rituximab era: results from the UK NCRI R-CHOP 14 v 21 Phase III Trial. Blood. 2016;128(22):1746–1746.
Staiger AM, Ziepert M, Horn H, Scott DW, et al. Clinical impact of the cell-of-origin classification and the MYC/ BCL2 dual expresser status in diffuse large B-cell lymphoma treated within prospective clinical trials of the German high-grade non-Hodgkin’s lymphoma study group. J Clin Oncol. 2017;35(22):2515–26.
Scott DW, Mottok A, Ennishi D, Wright GW, et al. Prognostic significance of diffuse large B-cell lymphoma cell of origin determined by digital gene expression in formalin-fixed paraffin-embedded tissue biopsies. J Clin Oncol. 2015;33(26):2848–56.
Kennedy-Martin T, Curtis S, Faries D, Robinson S, et al. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials. 2015;16:495.
Rosenwald A, Bens S, Advani R, Barrans S, et al. Prognostic significance of MYC rearrangement and translocation partner in diffuse large B-cell lymphoma: a study by the Lunenburg Lymphoma Biomarker Consortium. J Clin Oncol. 2019;37(35):3359–68 To date, the largest study determining the prognostic significance of MYC rearrangement in DLBCL establishing an adverse prognostic impact of MYC-R only evident in patients with a concurrent rearrangement of BCL2 and/or BCL6 and an IG partner
Bertrand P, Bastard C, Maingonnat C, Jardin F, et al. Mapping of MYC breakpoints in 8q24 rearrangements involving non-immunoglobulin partners in B-cell lymphomas. Leukemia. 2007;21(3):515–23.
Copie-Bergman C, Cuilliere-Dartigues P, Baia M, Briere J, et al. MYC-IG rearrangements are negative predictors of survival in DLBCL patients treated with immunochemotherapy: a GELA/LYSA study. Blood. 2015;126(22):2466–74.
Savage KJ, Johnson NA, Ben-Neriah S, Connors JM, et al. MYC gene rearrangements are associated with a poor prognosis in diffuse large B-cell lymphoma patients treated with R-CHOP chemotherapy. Blood. 2009;114(17):3533–7.
Barrans S, Crouch S, Smith A, Turner K, et al. Rearrangement of MYC is associated with poor prognosis in patients with diffuse large B-cell lymphoma treated in the era of rituximab. J Clin Oncol. 2010;28(20):3360–5.
Green TM, Young KH, Visco C, Xu-Monette ZY, et al. Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30(28):3460–7.
Scott DW, King RL, Staiger AM, Ben-Neriah S, et al. High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements with diffuse large B-cell lymphoma morphology. Blood. 2018;131(18):2060–4.
Sha C, Barrans S, Cucco F, Bentley MA, et al. Molecular High-Grade B-Cell Lymphoma: Defining a Poor-Risk Group That Requires Different Approaches to Therapy. J Clin Oncol, 2019;37(3):202–212 The study defined a gene expression signature focusing on double hit lymphomas and identified subsets of DLBCL patients with an inferior prognosis, beyond the survival distinctions associated with the COO classification
Sha C, Barrans S, Cucco F, Bentley MA, et al. Molecular High-Grade B-Cell Lymphoma: Defining a Poor-Risk Group That Requires Different Approaches to Therapy. J Clin Oncol. 2019;37(3):202-212 Gene expression study that defined a Molecular High Grade expression signature containing genes highly expressed in BL that identified DLBCL patients with an inferior prognosis, beyond the survival distinctions associated with the COO classification
Johnson NA, Slack GW, Savage KJ, Connors JM, et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30(28):3452–9.
Davies A, Cummin TE, Barrans S, Maishman T, et al. Gene-expression profiling of bortezomib added to standard chemoimmunotherapy for diffuse large B-cell lymphoma (REMoDL-B): an open-label, randomised, phase 3 trial. Lancet Oncol. 2019;20(5):649–62.
Horn H, Ziepert M, Wartenberg M, Staiger AM, et al. Different biological risk factors in young poor-prognosis and elderly patients with diffuse large B-cell lymphoma. Leukemia. 2015;29(7):1564–70.
Barraclough A, Alzahrani M, Ettrup MS, Bishton M, et al. COO and MYC/BCL2 status do not predict outcome among patients with stage I/II DLBCL: a retrospective multicenter study. Blood Adv. 2019;3(13):2013–21.
Chapuy B, Stewart C, Dunford AJ, Kim J, et al. Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat Med. 2018;24(5):679–690 Multiplatform genomic analysis elucidating the heterogeneity of DLBCL resulting in a genetic taxonomy of DLBCL that provided unexpected biological and clinical insights
Lawrence MS, Stojanov P, Polak P, Kryukov GV, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499(7457):214–8.
Kamburov A, Lawrence MS, Polak P, Leshchiner I, et al. Comprehensive assessment of cancer missense mutation clustering in protein structures. Proc Natl Acad Sci U S A. 2015;112(40):E5486–95.
Monti S, Chapuy B, Takeyama K, Rodig SJ, et al. Integrative analysis reveals an outcome-associated and targetable pattern of p53 and cell cycle deregulation in diffuse large B cell lymphoma. Cancer Cell. 2012;22(3):359–72.
Wright GW, Huang DW, Phelan JD, Coulibaly ZA, et al. A Probabilistic Classification Tool for Genetic Subtypes of Diffuse Large B Cell Lymphoma with Therapeutic Implications. Cancer Cell. 2020;37(4):551–568 e14 Development of the LymphGen algorithm that defined of seven genetic subtypes of DLBCL using genomic data from 1200 DLBCL. Publicly available classification tool to categorize a single DLBCL biopsy into genetic subtypes using whole exome or targeted sequencing data
Challa-Malladi M, Lieu YK, Califano O, Holmes AB, et al. Combined genetic inactivation of beta2-Microglobulin and CD58 reveals frequent escape from immune recognition in diffuse large B cell lymphoma. Cancer Cell. 2011;20(6):728–40.
Morales JC, Franco S, Murphy MM, Bassing CH, et al. 53BP1 and p53 synergize to suppress genomic instability and lymphomagenesis. Proc Natl Acad Sci U S A. 2006;103(9):3310–5.
Tallen G, Riabowol K. Keep-ING balance: tumor suppression by epigenetic regulation. FEBS Lett. 2014;588(16):2728–42.
Rosati E, Baldoni S, De Falco F, Del Papa B, et al. NOTCH1 Aberrations in Chronic Lymphocytic Leukemia. Front Oncol. 2018;8:229.
Young RM, Shaffer AL 3rd, Phelan JD, Staudt LM. B-cell receptor signaling in diffuse large B-cell lymphoma. Semin Hematol. 2015;52(2):77–85.
Bertoni F, Rossi D, Zucca E. Recent advances in understanding the biology of marginal zone lymphoma. F1000Res. 2018;7:406.
Dominguez PM, Ghamlouch H, Rosikiewicz W, Kumar P, et al. TET2 Deficiency Causes Germinal Center Hyperplasia, Impairs Plasma Cell Differentiation, and Promotes B-cell Lymphomagenesis. Cancer Discov. 2018;8(12):1632–53.
Lu D, Liu L, Ji X, Gao Y, et al. The phosphatase DUSP2 controls the activity of the transcription activator STAT3 and regulates TH17 differentiation. Nat Immunol. 2015;16(12):1263–73.
Brescia P, Schneider C, Holmes AB, Shen Q, et al. MEF2B Instructs Germinal Center Development and Acts as an Oncogene in B Cell Lymphomagenesis. Cancer Cell. 2018;34(3):453-465 e9.
Muppidi JR, Schmitz R, Green JA, Xiao W, et al. Loss of signalling via Galpha13 in germinal centre B-cell-derived lymphoma. Nature. 2014;516(7530):254–8.
Wang H, Jain S, Li P, Lin JX, et al. Transcription factors IRF8 and PU.1 are required for follicular B cell development and BCL6-driven germinal center responses. Proc Natl Acad Sci U S A. 2019;116(19):9511–20.
Lakhotia R, Roschewski M. Circulating tumour DNA in B-cell lymphomas: current state and future prospects. Br J Haematol. 2021;193(5):867–81.
Roschewski M, Dunleavy K, Pittaluga S, Moorhead M, et al. Circulating tumour DNA and CT monitoring in patients with untreated diffuse large B-cell lymphoma: a correlative biomarker study. Lancet Oncol. 2015;16(5):541–9.
Scherer F, Kurtz DM, Newman AM, Stehr H, et al. Distinct biological subtypes and patterns of genome evolution in lymphoma revealed by circulating tumor DNA. Sci Transl Med. 2016;8(364):364ra155.
Kurtz DM, Scherer F, Jin MC, Soo J, et al. Circulating Tumor DNA Measurements As Early Outcome Predictors in Diffuse Large B-Cell Lymphoma. J Clin Oncol. 2018;36(28):2845-2853 Study demonstrating the prognostic impact of ctDNA measurements using liquid biopsies from DLBCL patients before and during immunochemotherapy
Rossi D, Diop F, Spaccarotella E, Monti S, et al. Diffuse large B-cell lymphoma genotyping on the liquid biopsy. Blood. 2017;129(14):1947–57.
Kurtz DM, Esfahani MS, Scherer F, Soo J, et al. Dynamic Risk Profiling Using Serial Tumor Biomarkers for Personalized Outcome Prediction. Cell. 2019;178(3):699-713 e19 Definition of risk prediction model integrating ctDNA analysis and established risk-factors to quantitatively estimate the risk for individual DLBCL patients throughout their disease
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Lymphomas
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weber, T., Schmitz, R. Molecular Subgroups of Diffuse Large B Cell Lymphoma: Biology and Implications for Clinical Practice. Curr Oncol Rep 24, 13–21 (2022). https://doi.org/10.1007/s11912-021-01155-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-021-01155-2