Abstract
Purpose of Review
The purpose of this article is to perform a systematic review over the past 5 years on the role and effectiveness of clinical decision support systems (CDSSs) on antibiotic stewardship.
Recent Findings
CDDS interventions found a significant impact on multiple outcomes relevant to antibiotic stewardship. There are various types of CDSS implementations, both active and passive (provider initiated). Passive interventions were associated with more significant outcomes; however, both interventions appeared effective. In the reviewed literature, CDSSs were consistently associated with decreasing antibiotic consumption and narrowing the spectrum of antibiotic usage. Generally, guideline adherence was improved with CDSS, although this was not universal. The effect on other outcomes, such as mortality, Clostridiodes difficile infections, length of stay, and cost, inconsistently showed a significant difference.
Summary
Overall, CDDS implementation has effectively decreased antibiotic consumption and improved guideline adherence across the various types of CDSS. Other positive outcomes were noted in certain settings, but were not universal. When creating a new intervention, it is important to identify the optimal structure and deployment of a CDSS for a specific setting.



Similar content being viewed by others
References
Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA. 2016;315(17):1864–73. https://doi.org/10.1001/jama.2016.4151.
Camins BC, King MD, Wells JB, et al. Impact of an antimicrobial utilization program on antimicrobial use at a large teaching hospital: a randomized controlled trial. Infect Control Hosp Epidemiol :Off J Soc Hosp Epidemiol Am. 2009;30(10):931–8.
Ingram PR, Seet JM, Budgeon CA, Murray R. Point-prevalence study of inappropriate antibiotic use at a tertiary Australian hospital. Intern Med J. Jun 2012;42(6):719–21.
Levin PD, Idrees S, Sprung CL, et al. Antimicrobial use in the ICU: indications and accuracy–an observational trial. J Hosp Med :Off Publ Soc Hosp Med. 2012;7(9):672–8.
Patel SJ, Oshodi A, Prasad P, Delamora P, Larson E, Zaoutis T, et al. Antibiotic use in neonatal intensive care units and adherence with centers for disease control and prevention 12 step campaign to prevent antimicrobial resistance. Pediatr Infect Dis J. 2009;28(12):1047–51.
Dellit TH, Owens RC, McGowan JE Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2007;44(2):159–77.
Fridkin SK, Baggs J, Fagan R, et al. Vital signs: improving antibiotic use among hospitalized patients. Morb Mortal Wkly Rep. 2014;63.
Centers for disease control and prevention, Office of infectious disease antibiotic resistance threats in the United States, 2013. Apr, 2013: http://www.cdc.gov/drugresistance/threat-report-2013. Accessed January 28, 2015.
Pollack LA, Srinivasan A, Core elements of hospital antibiotic stewardship programs from the centers for disease control and prevention, Clin Infect Dis, Volume 59, Issue suppl_3, 15 October 2014, Pages S97–S100, https://doi.org/10.1093/cid/ciu542
Dellit TH, Owens RC, McGowan JE, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 15 January 2007;44(2):159–77. https://doi.org/10.1086/510393.
Payne TH. Computer decision support. Chest 2000 Aug; 118 (2 Suppl):47S–52S doi: https://www.ncbi.nlm.nih.gov/pubmed/10939999.
Heard KL, Hughes S, Mughal N, Azadian BS, Moore LSP. Evaluating the impact of the ICNET® clinical decision support system for antimicrobial stewardship. Antimicrob Resist Infect Control 2019;8:51. Published 2019 Mar 6. doi:https://doi.org/10.1186/s13756-019-0496-4.
MacFadden DR, Coburn B, Shah N, Robicsek A, Savage R, Elligsen M, Daneman N. Decision-support models for empiric antibiotic selection in Gram-negative bloodstream infections. Clin Microbiol Infect 2019 Jan;25(1):108.e1–108.e7. doi: https://doi.org/10.1016/j.cmi.2018.03.029
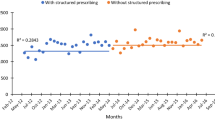
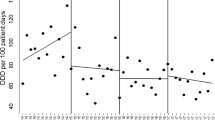
Gulliford MC, Prevost AT, Charlton J, Juszczyk D, Soames J, McDermott L, et al. Effectiveness and safety of electronically delivered prescribing feedback and decision support on antibiotic use for respiratory illness in primary care: REDUCE cluster randomised trial. BMJ. 2019;364:l236. Published 2019 Feb 13. https://doi.org/10.1136/bmj.l236.
Mostaghim M, Snelling T, McMullan B, Ewe YH, Bajorek B. Impact of clinical decision support on empirical antibiotic prescribing for children with community-acquired pneumonia. J Paediatr Child Health 2019 Mar;55(3):305–311. doi: https://doi.org/10.1111/jpc.14191. Epub 2018 Aug 30.
Jones BE, Collingridge DS, Vines CG, Post H, Holmen J, Allen TL, et al. CDS in a learning health care system: identifying physicians’ reasons for rejection of best-practice recommendations in pneumonia through computerized clinical decision support. Appl Clin Inform. 2019 Jan;10(1):1–9. https://doi.org/10.1055/s-0038-1676587.
Downing NL, Rolnick J, Poole SF, Hall E, Wessels AJ, Heidenreich P, Shieh L Electronic health record-based clinical decision support alert for severe sepsis: a randomised evaluation. BMJ Qual Saf Published Online First: 14 March 2019. doi: https://doi.org/10.1136/bmjqs-2018-008765
- Ozkaynak M, Wu DTY, Hannah K, Dayan PS, Mistry RD. Examining workflow in a pediatric emergency department to develop a clinical decision support for an antimicrobial stewardship program. Appl Clin Inform 2018;9(2):248–260. doi: https://doi.org/10.1055/s-0038-1641594
Wang F, Prier B, Bauer KA, Mellett J. Pharmacist-driven initiative for management of Staphylococcus aureus bacteremia using a clinical decision support system. Am J Health Syst Pharm. 2018;75(11 Supplement 2):S35–41. https://doi.org/10.2146/ajhp170087.
Jung AD, Baker J, Droege CA, Nomellini V, Johannigman J, Holcomb JB, et al. Sooner is better: use of a real-time automated bedside dashboard improves sepsis care. J Surg Res. 2018 Nov;231:373–9. https://doi.org/10.1016/j.jss.2018.05.078. Epub 2018 Jun 29.
Simões AS, Maia MR, Gregório J, Couto I, Asfeldt AM, Simonsen GS, et al. Participatory implementation of an antibiotic stewardship programme supported by an innovative surveillance and clinical decision-support system. J Hosp Infect. 2018;100.3:257–64 Web.
Keller SC, Feldman L, Smith J, Pahwa A, Cosgrove SE, Chida N The use of clinical decision support in reducing diagnosis of and treatment of asymptomatic bacteriuria. J Hosp Med 2018;13(6):392–395. doi: https://doi.org/10.12788/jhm.2892.
Akhloufi H, Hulscher M, van der Hoeven CP, Prins JM, van der Sijs H, Melles DC, et al. A clinical decision support system algorithm for intravenous to oral antibiotic switch therapy: validity, clinical relevance and usefulness in a three-step evaluation study. J Antimicrob Chemother. 2018 Aug 1;73(8):2201–6. https://doi.org/10.1093/jac/dky141.
Young H, Shihadeh K, Skinner A, Knepper B, Sankoff J, Voros J, et al. Implementation of an institution-specific antimicrobial stewardship smartphone application. Infect Control Hosp Epidemiol. 2018;39(8):986–8. https://doi.org/10.1017/ice.2018.135.
Blanco N, O'Hara LM, Robinson GL, Brown J, Heil E, Brown CH, Stump BD, Sigler BW, Belani A, Miller HL, Chiplinski AN, Perlmutter R, Wilson L, Morgan DJ, Leekha S. Health care worker perceptions toward computerized clinical decision support tools for Clostridium difficile infection reduction: a qualitative study at 2 hospitals. Am J Infect Control 2018 Oct;46(10):1160–1166. doi: https://doi.org/10.1016/j.ajic.2018.04.204
- Gunn LR, Tunney R, Kelly K. Nonmodal clinical decision support and antimicrobial restriction effects on rates of fluoroquinolone use in uncomplicated infections. Appl Clin Inform 2018;9(1):149–155. doi:https://doi.org/10.1055/s-0038-1626726.
Giuliano CA, Binienda J, Kale-Pradhan PB, Fakih MG. “I never would have caught that before”: pharmacist perceptions of using clinical decision support for antimicrobial stewardship in the United States. Qual Health Res. 2018;28(5):745–55.
Messacar K, Hurst AL, Child J, Campbell K, Palmer C, Hamilton S, et al. Clinical impact and provider acceptability of real-time antimicrobial stewardship decision support for rapid diagnostics in children with positive blood culture results. J Pediatric Infect Dis Soc. 2016;6(3):267–74. https://doi.org/10.1093/jpids/piw047.
Nault V, Pepin J, Beaudoin M, Perron J, Moutquin JM, Valiquette L. Sustained impact of a computer-assisted antimicrobial stewardship intervention on antimicrobial use and length of stay. J Antimicrob Chemother. 2017;72(3):933–40 Web.
Berrevoets MAH, Pot JHLW, Houterman AE, et al. An electronic trigger tool to optimise intravenous to oral antibiotic switch: a controlled, interrupted time series study. Antimicrob Resist Infect Control 2017;6:81. Published 2017 Aug 15. doi:https://doi.org/10.1186/s13756-017-0239-3.
Bond SE, Chubaty AJ, Adhikari S, Miyakis S, Boutlis CS, Yeo WW, Batterham MJ, Dickson C, McMullan BJ, Mostaghim M, Li-Yan Hui S, Clezy KR, Konecny P. Outcomes of multisite antimicrobial stewardship programme implementation with a shared clinical decision support system. Journal of Antimicrobial Chemotherapy 72.7 (2017): 2110–118. Web.
Huh K, Chung DR, Park HJ, Kim MJ, Lee NY, Ha YE, Kang CI, Peck KR, Song JH. Impact of monitoring surgical prophylactic antibiotics and a computerized decision support system on antimicrobial use and antimicrobial resistance Am J Infect Control: 44.9 (2016): E145–E152. Web.
Okumura LM, Veroneze I, Burgardt CI, Fragoso MF. Effects of a computerized provider order entry and a clinical decision support system to improve cefazolin use in surgical prophylaxis: a cost saving analysis. Pharm Pract (Granada). 2016;14(3):717. https://doi.org/10.18549/PharmPract.2016.03.717.
Caplinger C, Smith G, Remington R, Madaras-Kelly K. Evaluation of a computerized decision support intervention to decrease use of anti-pseudomonal carbapenems in penicillin allergic patients. Antibiotics (Basel) 2016;5(1):7. Published 2016 Jan 15. doi:https://doi.org/10.3390/antibiotics5010007.
Beaudoin M, Kabanza F, Nault V, Valiquette L. Evaluation of a machine learning capability for a clinical decision support system to enhance antimicrobial stewardship programs. Artif Intell Med. 2016;68(1):29–36 Web.
Chow AL, Ang A, Chow CZ, Ng TM, Teng C, Ling LM, et al. Implementation hurdles of an interactive, integrated, point-of-care computerised decision support system for hospital antibiotic prescription. Int J Antimicrob Agents. 2016;47(2):132–9 Web.
Chow AL, Lye DC, Arah OA. Patient and physician predictors of patient receipt of therapies recommended by a computerized decision support system when initially prescribed broad-spectrum antibiotics: a cohort study. J Am Med Inform Assoc. 2015;23(e1):e58–70. https://doi.org/10.1093/jamia/ocv120.
Tsoukalas A, Albertson T, Tagkopoulos I. From data to optimal decision making: a data-driven, probabilistic machine learning approach to decision support for patients with sepsis. JMIR Med Inform. 2015;3(1):e11. Published 2015 Feb 24. https://doi.org/10.2196/medinform.3445.
Dean NC, Jones BE, Jones JP, Ferraro JP, Post HB, Aronsky D, Vines CG, Allen TL, Haug PJ.. Impact of an electronic clinical decision support tool for emergency department patients with pneumonia. Ann Emerg Med 66.5 (2015): 511–520. Web.
Chow AL, Lye DC, Arah OA. Mortality benefits of antibiotic computerised decision support system: modifying effects of age. Sci Rep. 2015;5:17346. Published 2015 Nov 30. https://doi.org/10.1038/srep17346.
Faine B, Mohr N, Harland KK, Rolfes K, Porter B, Fuller BM. Importance of decision support implementation in emergency department vancomycin dosing. West J Emerg Med. 2015;16(4):557–64. https://doi.org/10.5811/westjem.2015.4.25760.
Diasinos N, Baysari M, Kumar S, Day RO. Does the availability of therapeutic drug monitoring, computerised dose recommendation and prescribing decision support services promote compliance with National Gentamicin Prescribing Guidelines? Intern Med J. 2015;45(1):55–62 Web.
Michaelidis CI, Kern MS, Smith KJ. Cost-effectiveness of decision support strategies in acute bronchitis. J Gen Intern Med. 2015;30(10):1505–10. https://doi.org/10.1007/s11606-015-3289-3.
- Kannry J, McCullagh L, Kushniruk A, Mann D, Edonyabo D, McGinn T. A Framework for usable and effective clinical decision support: experience from the iCPR randomized clinical trial. EGEMS (Wash DC). 2015;3(2):1150. Published 2015 Jul 9. doi:https://doi.org/10.13063/2327-9214.1150
Payne KF, Weeks L, Dunning P. A mixed methods pilot study to investigate the impact of a hospital-specific iPhone application (iTreat) within a British junior doctor cohort. Health Informatics Journal. 2013;20(1):59–73. https://doi.org/10.1177/1460458213478812.
Mani S, Ozdas A, Aliferis C, Varol HA, Chen Q, Carnevale R, et al. Medical decision support using machine learning for early detection of late-onset neonatal sepsis. J Am Med Inform Assoc. 2013;21(2):326–36. https://doi.org/10.1136/amiajnl-2013-001854.
Fonzo-Christe C, Guignard B, Zaugg C, Coehlo A, Posfay-Barbe KM, Gervaix A, et al. Impact of clinical decision support guidelines on therapeutic drug monitoring of gentamicin in newborns. Ther Drug Monit. 2014;36(5):656–62 Web.
Rodriguez-Maresca M, Sorlozano A, Grau M, Rodriguez-Castaño R, Ruiz-Valverde A, Gutierrez-Fernandez J. Implementation of a computerized decision support system to improve the appropriateness of antibiotic therapy using local microbiologic data. Biomed Res Int. 2014;2014:395434. https://doi.org/10.1155/2014/395434.
Arboe, Laub, Kronborg, and Knudsen. Evaluation of the decision support system for antimicrobial treatment, TREAT, in an acute medical ward of a university hospital. Int J Infect Dis (2014): 156–161, 29.
Gulliford MC, van Staa T, Dregan A, et al. Electronic health records for intervention research: a cluster randomized trial to reduce antibiotic prescribing in primary care (eCRT study). Ann Fam Med 2014;12(4):344–351. doi: https://doi.org/10.1370/afm.1659 .
Hum RS, Cato K, Sheehan B, Patel S, Duchon J, DeLaMora P, et al. Developing clinical decision support within a commercial electronic health record system to improve antimicrobial prescribing in the neonatal ICU. Appl Clin Inform. 2014;5(2):368–87. Published 2014 Apr 9. https://doi.org/10.4338/ACI-2013-09-RA-0069.
May LJ, Longhurst CA, Pageler NM, Wood MS, Sharek PJ, Zebrack CM. Optimizing care of adults with congenital heart disease in a pediatric cardiovascular ICU using electronic clinical decision support*. Pediatr Crit Care Med. 2014 Jun;15(5):428–34. https://doi.org/10.1097/PCC.0000000000000124.
Demonchy E, Dufour JC, Gaudart J, Cervetti E, Michelet P, Poussard N, et al. Impact of a computerized decision support system on compliance with guidelines on antibiotics prescribed for urinary tract infections in emergency departments: a multicentre prospective before-and-after controlled interventional study. J Antimicrob Chemother. 2014;69.10:2857–63 Web.
Nachtigall I, Tafelski S, Deja M, Halle E, Grebe MC, Tamarkin A, et al. Long-term effect of computer-assisted decision support for antibiotic treatment in critically ill patients: a prospective ‘before/after’ cohort study. BMJ Open. 2014;4(12):e005370. Published 2014 Dec 22. https://doi.org/10.1136/bmjopen-2014-005370.
Gulliford MC, Juszczyk D, Prevost AT, et al. Electronically delivered interventions to reduce antibiotic prescribing for respiratory infections in primary care: cluster RCT using electronic health records and cohort study. Southampton (UK): NIHR Journals Library; 2019 Mar. (Health Technology Assessment, No. 23.11.)
Haque F, Ball RL, Khatun S, Ahmed M, Kache S, Chisti MJ, et al. Evaluation of a smartphone decision-support tool for diarrheal disease management in a resource-limited setting. PLoS Negl Trop Dis. 2017;11(1):e0005290. Published 2017 Jan 19. https://doi.org/10.1371/journal.pntd.0005290.
Gifford J, Vaeth E, Richards K, Siddiqui T, Gill C, Wilson L, et al. Decision support during electronic prescription to stem antibiotic overuse for acute respiratory infections: a long-term, quasi-experimental study. BMC Infect Dis. 2017;17(1):528. Published 2017 Jul 31. doi:. https://doi.org/10.1186/s12879-017-2602-7.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Barry Rittmann and Michael Stevens declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
Rights and permissions
About this article
Cite this article
Rittmann, B., Stevens, M.P. Clinical Decision Support Systems and Their Role in Antibiotic Stewardship: a Systematic Review. Curr Infect Dis Rep 21, 29 (2019). https://doi.org/10.1007/s11908-019-0683-8
Published:
DOI: https://doi.org/10.1007/s11908-019-0683-8