Abstract
Intestinal helminth infections are some of world’s most common tropical diseases and cause significant impairments in pediatric growth and cognitive impairment as well as maternal health, particularly in areas lacking adequate access to safe water or sanitation. Routine mass drug administration (MDA) of anthelminthic medications to children living in endemic areas and interventions to improve water hygiene and sanitation form the basis of current control efforts. We review recent evidence on the effectiveness of these approaches and outline the limitations of MDA, including poor cure rates against hookworm and Trichuris trichiura, rapid post-MDA reinfection, and inadequate coverage of at-risk populations. Ultimately, alternative tools and strategies, including new drugs, drug combinations, and vaccines, will be needed to control or ultimately eliminate these infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intestinal helminth infections are some of the most common afflictions of world’s poorest people [1]. Over two billion individuals, most of whom survive on incomes of less than $1–2 per day, are chronically parasitized by worms living in their intestines [1]. These infections are among world’s most common chronic diseases, and based on the number of disability-adjusted life years (DALYs) lost, they are some of the most important neglected tropical diseases (NTDs) [1]. The most prevalent and important (in terms of global disease burden) intestinal helminths fall into two main categories: the soil-transmitted helminths (STH) and the foodborne trematodes. The hallmark of chronic infection with these parasites is the often insidious morbidity and disability that they can induce, as well as impairment of childhood nutrition and both physical and cognitive development. Mortality that is directly attributable to intestinal helminths is rare.
An estimated 1.45 billion people worldwide are infected with one of the three major STHs—Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), or one of the two species of human hookworm (Necator americanus and Ancylostoma duodenale)—with almost 70 % of infections occurring in Asia [2]. The global disease burden of these infections is estimated to result in the loss of 5.18 million DALYs annually. Globally, over the past two decades, there have been significant reductions in prevalence, with 140 million fewer people infected, much of which is attributable to China where STH prevalence declined from 57.5 to 11.4 % between 1990 and 2010, likely due to a number of factors including economic development and improved access to safe water and sanitation [2, 3].
Ascariasis, caused by A. lumbricoides, is the most prevalent STH, with around 890 million people infected [2]. Although less than 3000 deaths a year is directly attributable to A. lumbricoides, chronic infections nevertheless result in the loss of over 1.3 million DALYs [2]. T. trichiura occurs globally in humid regions of the tropics, where 465 million people are infected, and causes the loss of 0.64 million DALYs annually. Of the three major STHs, the two human hookworm species cause the majority (65 %) of Years Lived with Disability attributable to STHs, largely due to the iron-deficiency anemia that results from chronic infection [4]. Children with moderate and heavy intensity hookworm infections suffer from impaired growth and deficits in intellectual and cognitive development. Furthermore, up to a third of pregnant women in Africa are infected with hookworms, which can result in severe anemia, increased maternal morbidity and mortality, premature birth, and neonatal anemia [5, 6]. In the latest estimates, hookworms infect approximately 440 million people and result in the annual loss of 3.2 million DALYs [2].
Strongyloidiasis, mostly commonly caused by Strongyloides stercoralis, is the fourth major STH infection but is much less prevalent than the other three. It occurs worldwide in the tropics in areas with poor sanitation with a lower prevalence in temperate regions in rural areas. Although data are less reliable for this STH, estimates are that between 30 and 100 million people are infected in tropical and subtropical countries [7].
Although less common than the STHs, intestinal trematode and fluke infections are associated with significant disease burden in parts of the world [8•]. These so-called foodborne trematodiases are caused by ingestion of raw or undercooked freshwater fish, shellfish, reptiles, or aquatic plants that are contaminated with encysted forms of the parasites. The intestinal trematodes are a heterogeneous group of over 70 different species such as Fasciolopsis buski, the heterophyids, and Echinostoma species that affect a broad range of countries in the tropics. F. buski, the giant intestinal fluke, is one of the most common species and is most prevalent in the south and Southeast Asia. The most important liver flukes are Clonorchis sinensis and Opisthorchis viverrini, both of which inhabit the bile ducts. These are especially prevalent in parts of China and Southeast Asia, and chronic infection is strongly associated with the development cholangiocarcinoma [9]. Over 6.7 million individuals are infected with one of the foodborne trematodes worldwide, accounting for about 2.4 million DALYs lost yearly [1].
Mass Drug Administration (MDA)
The current approach to controlling the large disease burden due to intestinal helminth infections centers on mass drug administration (MDA) of anthelminthic drugs as well as improving water sanitation and supply. Each of the major intestinal helminths can be effectively targeted with safe, well-tolerated, and effective medications that are easily administered and integrated into national control programs in endemic areas (Table 1). The three soil-transmitted helminths—A. lumbricoides, T. trichiura, and the hookworms—are susceptible (to varying degrees, see below) to the benzimidazole class of drugs, of which albendazole and mebendazole are the most commonly used in MDA programs, whereas praziquantel is effective against most of the foodborne trematodiases and ivermectin for strongyloidiasis.
Recently, global efforts have focused on expanding the reach of MDA programs. In 2013, the World Health Assembly passed a resolution (WHA 66.12) calling for further scale-up of MDA through development of national integrated NTD programs, as well as provision of safe drinking water and improved sanitation [10]. Furthermore, in 2012, the London Declaration on Neglected Tropical Diseases set specific goals for the control of intestinal helminths and committed several multinational pharmaceutical companies to donating the drugs used in MDA programs in endemic areas [11].
To date, much remains to be done to increase the coverage of MDA to those most in need. Although an estimated 900 million children are at risk for intestinal helminth infections, only approximately 30 % are being reached by MDA programs [12]. Recent progress has been made, however, due to the coordinated efforts prompted by the London Declaration, national NTD programs, and funding agencies such as the Bill & Melinda Gates Foundation. According to the most recent update on the London Declaration, in 2012, there was a net increase of 60 million MDA treatments over the previous year, with most of the increase due to drugs targeting the intestinal nematodes; almost 1.35 billion treatments were donated and distributed to endemic countries in 2013 [13••].
Repeated and regular administration of MDA has had a significant impact in reducing the prevalence of infection in endemic countries [14•, 15–18]. For example, after 5 years of administration of single-dose albendazole every 6 months to one million preschool children in India, the prevalence of intestinal nematode eggs (Ascaris and hookworm) on fecal examinations was 16 % in randomly selected communities compared to 35 % in control (no MDA) communities [14•]. To date, however, these reductions in infection prevalence have not been shown to have significant impact on the chronic sequelae of infection such as growth, school attendance, or school performance, although some studies have demonstrated modest improvements in weight gain [14•, 19•].
In addition to reducing the prevalence of the helminths that are being targeted by MDA, it has been suggested that it would also have ancillary positive impacts on other diseases. For example, several studies have suggested associations between progression of HIV disease and co-infection with other endemic organisms [20, 21]. Initial results from a trial conducted in Kenya indicated that treatment with albendazole delayed decreases in CD4 cell counts in those co-infected with HIV and A. lumbricoides [22]. However, in a subsequent large randomized, controlled trial in which HIV-infected individuals received empiric albendazole plus praziquantel every 3 months for 2 years compared to no treatment, there was no difference in the rate of people reaching a CD4 count of less than 350 cells/μl [23].
Although the overall benefits of MDA are considered to be positive, some investigators have cautioned that it may have some unintended negative effects. For example, it has been postulated that instead of improving the health of children, repeatedly administering MDA in areas where the intestinal helminths are endemic may lead to paradoxical increases in morbidity, in particular due to the allergic diseases. Intestinal nematodes typically induce a downregulated immune response that may protect the host not only from the strong inflammatory effects of helminth infections but also against the effects of allergic disorders such as atopy and asthma [24]. Reduced allergic responses have been shown in studies of mice infected with various helminths [25], and children born to mothers infected with hookworm during pregnancy had lower incidence of eczema compared to those born of uninfected women [26]. Population-based studies suggest that intestinal nematode infections are associated with reduced skin reactivity to common allergens and a lowered risk of asthma [27, 28]. Furthermore, in a small study of patients with multiple sclerosis, those who were infected with a STH had reduced risk of relapse due to their autoimmune disease, and administering anthelminthic treatment was associated with a worsening of symptoms [29].
Shortcomings of MDA
While MDA for other NTDs such as trachoma, lymphatic filariasis, and onchocerciasis has resulted in the elimination of these diseases in several regions, the same has not occurred for the STHs [30]. The reasons for this failure are several. According to a meta-analysis of randomized, controlled trials, single-dose mebendazole was very effective at treating A. lumbricoides but cured a mean of only 15 % of hookworm infections [31]. Reported egg count reduction rates (a surrogate measure of reduction in worm burden) were quite variable, ranging from 0 % to as high as 68 % for N. americanus infection. Similarly, MDA for STHs using single-dose mebendazole has not been shown to improve anemia prevalence [6, 19•]. Rates of cure for T. trichiura are even worse for single or multiple doses of mebendazole and albendazole [31]. As an example, a recent trial in Gabon reported a cure rate of only 83 % for trichuriasis even after three consecutive daily doses of albendazole [32••].
The reasons for such drug failures are unclear, but the observation that repeated use of mebendazole in the same communities is associated with diminishing efficacy has led some investigators to suggest the possibility of emerging drug resistance, although this remains controversial [33]. However, drug resistance to benzimidazoles used in animal husbandry has been described in intestinal nematodes infecting livestock. This resistance has been associated with point mutations in the parasite gene encoding β-tubulin, the target of this class of drug [34]. “Although the same mutations have not yet been associated with drug failure in humans, efforts are underway to determine whether benzimidazole failures for hookworm and other helminths result from similar resistance mechanisms” [35].
Studies using single or triple doses of albendazole have reported higher rates of cure than with mebendazole for hookworm, although drug failures have been seen, and in some areas of Africa, reinfection with this STH following MDA can occur in under a year [36–38]. Rapid post-treatment reinfection in areas of high transmission should prompt more frequent MDA as recommended by the WHO, even up to three times a year [39]. However, administering MDA with such regularity is often cost prohibitive and impractical. Currently, MDA is most often administered on an annual basis at the community level [39]. In addition, MDA programs target mostly preschool and school-aged children. However, this leaves out other affected populations, particularly women of childbearing age who are at increased risk of disease due to hookworm infection due to their already low iron stores [40]. Furthermore, whereas for ascariasis and trichuriasis, children are the main reservoir of infections, for hookworm, adults also have high prevalence and intensity of infection. Therefore, while repeated rounds of MDA have been shown to interrupt transmission of A. lumbricoides in endemic communities [41], hookworm transmission would be expected to continue unchecked if only children are targeted with MDA [42•]. These observations suggest the need for universal MDA that includes targeting adults in addition to children, if hookworm elimination is to be achievable through use of MDA alone.
Due to the low efficacy of the benzimidazoles against T. trichiura and the worry about development of drug resistance in all of the intestinal nematodes, recent emphasis has been given to testing combinations of anthelminthics, particularly those of drugs that have different mechanisms of action. This strategy mimics those for the treatment of such infections as malaria with artemisinin-based combination therapies, as well as HIV and tuberculosis.
For example, a recently published study in Tanzanian children showed significantly improved efficacy against T. trichiura when single-dose albendazole was combined with single-dose oxantel pamoate, a veterinary drug that is an orthologue of pyrantel pamoate, a nicotinic acetylcholine receptor agonist, although even this improvement resulted in cure rates of only 31.2 % compared to 11.8 % for single-dose mebendazole [43•]. The addition of ivermectin to albendazole or mebendazole has also been shown to significantly improve cure rates against T. trichiura (55 vs. 19 % for mebendazole alone) [44]. Of note, single-dose ivermectin is also an effective treatment for uncomplicated strongyloidiasis. Additionally, nitazoxanide has been proposed as a component of combination MDA based on in vitro evidence of synergism with albendazole and pyrantel pamoate with the laboratory nematode Caenorhabditis elegans [45]. However, a clinical trial in which single-dose nitazoxanide was added to albendazole showed no improvement in cure or egg reduction rates for T. trichiura yet resulted in increased reporting of adverse events [46]. Efficacy of this drug against the liver fluke Fasciola hepatica, however, has been shown to be equivalent to that of triclabendazole, the present drug of choice for chronic fascioliasis [47].
Integrated Control of NTDs
In much of sub-Saharan Africa and elsewhere in developing countries, A. lumbricoides, T. trichiura, hookworm, and S. stercoralis are co-endemic with each other and also with several other NTDs, including schistosomiasis, lymphatic filariasis, onchocerciasis, and trachoma. The January 2012 London Declaration on the NTDs emphasized the importance of targeting the STHs through increased control efforts, as well as integrating these efforts with the control or elimination of several other NTDs. The major emphasis of such efforts is based on MDA using a “rapid impact package” of drugs that has been donated by several of world’s large pharmaceutical companies, which includes albendazole (GlaxoSmithKline) and mebendazole (Johnson&Johnson), but also ivermectin (onchocerciasis and lymphatic filariasis), praziquantel (schistosomiasis), and azithromycin (trachoma) [48•]. Large pharmacovigilance studies have shown that the benzimidazoles, praziquantel, and ivermectin can be safely co-administered with no increase in adverse effects or reduction in efficacy of the individual drugs, whereas safety data for the addition of azithromycin to these drugs is less extensive but nevertheless encouraging [49, 50].
To date, liver and intestinal fluke infections have not been specifically targeted with MDA despite the high burdens of disease due to these helminths in parts of Southeast Asia and China. The addition of single-dose praziquantel to existing MDA programs for the STHs would effectively treat all of these platyhelminthes, with the exception of the liver fluke F. hepatica. Additionally, tribendimidine has recently been shown to have equivalent efficacy against C. sinensis as praziquantel with fewer adverse events, albeit using a three-day course of treatment that would not facilitate seamless integration into current MDA programs [51].
Mapping of Intestinal Nematode Prevalence
Ensuring that MDA reaches those who need it requires a detailed understanding of where those populations live. Unfortunately, since intestinal helminth infections are most common in rural, resource-limited areas of the tropics that do not have well-developed healthcare infrastructure or systems, this information is often lacking. To remedy this deficiency, an open-access platform called Global Atlas of Helminth Infections (GAHI) was launched in 2010 to improve the accuracy of the epidemiology of worm infections, including the soil-transmitted helminths (www.thiswormyworld.org). Additionally, a concerted effort has been launched to link dynamic mathematical models of helminth infection, developed using data from sampling protocols from large-scale MDA programs, with geostatistical mapping techniques [52].
Water and Sanitation
MDA requires augmentation with improved water quality, sanitation, and hygiene (WASH) in order to be effective and sustainable. Water and sanitation are critical to preventing reinfections or new infections given the significant current prevalence of STHs [53•]. Specifically, research has supported the utility of using treated water, piped water, latrine access, hand hygiene, and footwear use. WASH improvements have been associated with between 33 and 49 % reduced probability of STH infection based on pooled odds ratios in recent meta-analyses [54]. Access to sanitation has been found to be particularly important in reducing rates of A. lumbricoides and T. trichiura infection whereas footwear use has been more strongly associated with reduction of hookworm infections. Although these results show the advantageous effects of WASH interventions on the prevalence of STH infection, most studies have been cross-sectional, and there is a need for more randomized, controlled trials to guide program implementation. Prior success in developed countries, including the USA, with water and sanitation improvements in coordination with deworming policies also supports the value of WASH interventions [53•].
Development of New Control Tools
New Anthelminthic Drugs
Concerns about the reliance on a single class of anthelminthic medications—the benzimidazoles—for the treatment and control of intestinal nematodes have prompted renewed interest in developing new classes of treatment. Unfortunately, given the “neglected” nature of the intestinal helminths, development of new drugs targeting these parasites is not a high priority of the major pharmaceutical companies. Nevertheless, some promising leads have been reported recently. Tribendimidine has been licensed in China since 2004 for the treatment of intestinal helminths and acts as a nicotinic acetylcholine receptor agonist. To date, good cure and egg reduction rates have been shown with a single dose of tribendimidine in human clinical trials against A. lumbricoides (>90 %) and hookworm (>80 %), although efficacy against T. trichiura and S. stercoralis is less promising [55].
An interesting drug under development comes from a completely new class of compounds, the pore-forming crystal (Cyr) proteins expressed by Bacillus thuringiensis [56]. In particular, Cry5B has been shown to have in vivo activity against the pig ascarid Ascaris suum [57•] and the zoonotic hookworm species Ancylostoma ceylanicum [58]. Of interest, Cry5B has been shown to have synergistic activity against intestinal nematodes when combined with a nicotinic acetylcholine receptor agonist drug [56].
Another new anthelminthic drug from a completely new class of compounds is monepantel, an amino-acetonitrile derivative [59]. This class of drugs has a novel mechanism of action involving a unique, nematode-specific clade of nicotinic acetylcholine receptor subunits that leads to spastic paralysis of the worm pharynx and ultimately worm death. Although monepantel displays in vitro and in vivo activity against some zoonotic intestinal nematodes, elimination of N. americanus and A. suum worms was minimal in preclinical testing, and therefore, this product is not currently being considered for human clinical development.
Anthelminthic Vaccines
Given the shortcomings of current approaches to the control of the intestinal helminths as outlined above, alternative strategies such as preventative vaccines are needed. Since hookworm causes the highest burden of disease of these parasitic infections, and the fact that MDA may be less effective for hookworm than other intestinal helminth infections, it is currently the main focus of vaccine development efforts, to date.
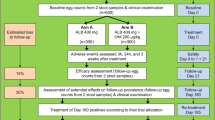
Currently, there are no licensed anthelminthic vaccines for humans. Of the major intestinal helminth pathogens, candidate vaccines are in clinical trials only for hookworm. The Human Hookworm Vaccine is currently being developed by the Sabin Vaccine Institute Product Development Partnership [42•]. Since hookworms are complex multicellular parasites, producing an efficacious vaccine against them is an even more formidable challenge than developing vaccines for malaria or other unicellular parasites. To date, three candidate hookworm vaccines have been tested in phase 1 clinical trials in the USA and in Brazil. The first candidate—the Na-ASP-2 vaccine containing an antigen produced by the larval stage of N. americanus—induced urticarial reactions when administered to adults living in a hookworm-endemic area due to preexisting IgE antibodies to the vaccine antigen, likely resulting from prior infections [60]. Further development of this candidate vaccine was subsequently halted. Instead, two vaccine products based on the Na-APR-1 (N. americanus aspartic protease-1) and Na-GST-1 (N. americanus glutathione-S-transferase-1) antigens are currently being tested in a series of phase 1 trials in both hookworm-naïve and hookworm-exposed volunteers [61]. Both of these antigens are involved in the hemoglobin digestion pathway of adult N. americanus hookworms, and extensive seroepidemiologic surveys in endemic areas of Brazil have shown a lack of IgE antibodies against them in previously infected individuals, regardless of age. Therefore, the risk of allergic reactions developing upon vaccination with these products is low.
Plans are underway to develop an experimental controlled infection model to test the proof-of-concept that candidate hookworm vaccines can impact infection with N. americanus. In this model, healthy, hookworm-naïve adult volunteers will be vaccinated and then challenged with infectious larvae. An initial feasibility study will soon be started at the George Washington University in Washington, DC. Provided proof-of-concept is demonstrated with the current antigens under development; the clinical development plan for the Human Hookworm Vaccine is to eventually combine Na-APR-1 and Na-GST-1 into a single, co-formulated product. This co-formulated product will be tested in phase 2b and 3 studies in hookworm-endemic regions of Brazil and sub-Saharan Africa to evaluate its efficacy in preventing moderate and heavy infections and the resulting intestinal blood loss and anemia. The eventual licensed vaccine will be targeted to children living in endemic areas, as well as other high-risk groups such as females of childbearing age.
Vaccine development for the other intestinal helminths is not nearly as advanced as it is for hookworm, although a multicomponent vaccine targeting ascariasis and trichuriasis as well as hookworm has been mooted [62]. Although no products for these two helminthiases have reached the stage of clinical trials, several potential vaccine antigens have been proposed for both. Several A. lumbricoides homologues of antigens discovered in A. suum have shown efficacy in animal models of infection, whereas vaccine feasibility has also been demonstrated in preclinical testing for T. trichiura [62, 63].
Conclusions
Intestinal helminth infections are some of the most common of world’s poorest people. MDA is an essential tool for achieving the Millennium Development Goals, especially those linked to maternal and child health and to help reduce poverty in the poorest regions of Africa, Asia, and Latin America. MDA is currently being used to control the major three STH infections but as yet has not been extensively implemented for strongyloidiasis or the foodborne trematodiases. In addition, several obstacles exist to the adequate control of these infections through MDA. These include lack of access to the anthelminthic drugs that form the basis of MDA, inadequate funding to expand existing MDA programs or to implement new ones in areas that do not currently have them, deficient geospatial and population prevalence data to guide focused targeting of MDA, potential development of drug resistance to existing anthelminthics used for MDA, and a paucity of new anthelminthic drugs or drug combinations that are under development. However, efforts are underway to address all of these shortcomings, led by such organizations as the World Health Organization, the Bill & Melinda Gates Foundation, and national governments. Finally, in order to move beyond the current goal of the control of intestinal helminth infections and target elimination of these parasites, new tools such as vaccines will need to be developed and implemented.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223.
Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasitol Vectors. 2014;7:37.
Yang GJ, Liu L, Zhu HR, Griffiths SM, Tanner M, Bergquist R, et al. China’s sustained drive to eliminate neglected tropical diseases. Lancet Infect Dis. 2014;14:881–92.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96.
McClure EM, Meshnick SR, Mungai P, Malhotra I, King CL, Goldenberg RL, et al. The association of parasitic infections in pregnancy and maternal and fetal anemia: a cohort study in coastal Kenya. PLoS Negl Trop Dis. 2014;8:e2724.
Brooker S, Hotez PJ, Bundy DA. Hookworm-related anaemia among pregnant women: a systematic review. PLoS Negl Trop Dis. 2008;2:e291.
Furst T, Keiser J, Utzinger J. Global burden of human food-borne trematodiasis: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:210–21.
Furst T, Sayasone S, Odermatt P, Keiser J, Utzinger J. Manifestation, diagnosis, and management of foodborne trematodiasis. BMJ. 2012;344:e4093. Excellent review of the foodborne trematodes, including the major intestinal and hepatobiliary flukes.
Petney TN, Andrews RH, Saijuntha W, Wenz-Mucke A, Sithithaworn P. The zoonotic, fish-borne liver flukes Clonorchis sinensis, Opisthorchis felineus and Opisthorchis viverrini. Int J Parasitol. 2013;43:1031–46.
WHA 66.12 Neglected tropical diseases. Sixty-Sixth World Health Assembly. Geneva: 27 May 2013. World Health Organization; http://www.who.int/neglected_diseases/mediacentre/WHA_66.12_Eng.pdf?ua=1. [Accessed 25 Sept 2014].
London Declaration on Neglected Tropical Diseases. London; January 2013. United to Combat Neglected Tropical Diseases; http://unitingtocombatntds.org/sites/default/files/resource_file/london_declaration_on_ntds.pdf [Accessed 20 Sept 2014].
Barry MA, Simon GG, Mistry N, Hotez PJ. Global trends in neglected tropical disease control and elimination: impact on child health. Arch Dis Child. 2013;98:635–41.
London Declaration on Neglected Tropical Diseases: delivering on promises and driving progress. London: Uniting to Combat NTDs; http://unitingtocombatntds.org/sites/default/files/document/NTD_report_04102014_v4_singles.pdf [Accessed 20 Sept 2014]. Update on most recent progress made in expanding mass drug administration for neglected tropical diseases to at-risk areas.
Awasthi S, Peto R, Read S, Richards SM, Pande V, Bundy D, et al. Population deworming every 6 months with albendazole in 1 million pre-school children in North India: DEVTA, a cluster-randomised trial. Lancet 2013;381:1478–1486. Large longitudinal study demonstrating significant impact of regular mass drug administration on intestinal nematode infections.
Supali T, Djuardi Y, Bradley M, Noordin R, Ruckert P, Fischer PU. Impact of six rounds of mass drug administration on Brugian filariasis and soil-transmitted helminth infections in eastern Indonesia. PLoS Negl Trop Dis. 2013;7:e2586.
Knopp S, Stothard JR, Rollinson D, Mohammed KA, Khamis IS, Marti H, et al. From morbidity control to transmission control: time to change tactics against helminths on Unguja Island, Zanzibar. Acta Trop. 2013;128:412–22.
Tun A, Myat SM, Gabrielli AF, Montresor A. Control of soil-transmitted helminthiasis in Myanmar: results of 7 years of deworming. Trop Med Int Health. 2013;18:1017–20.
Ruxin J, Negin J. Removing the neglect from neglected tropical diseases: the Rwandan experience 2008–2010. Glob Public Health. 2012;7:812–22.
Taylor-Robinson DC, Maayan N, Soares-Weiser K, Donegan S, Garner P. Deworming drugs for soil-transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin and school performance. Cochrane Database Syst Rev 2012;11:CD000371. Systematic review of the impact of routine mass drug administration on nutritional and cognitive outcomes as well as school attendance and performance.
Modjarrad K, Vermund SH. Effect of treating co-infections on HIV-1 viral load: a systematic review. Lancet Infect Dis. 2010;10:455–63.
Walson JL, Herrin BR, John-Stewart G. Deworming helminth co-infected individuals for delaying HIV disease progression. Cochrane Database Syst Rev 2009;CD006419.
Walson JL, John-Stewart G. Treatment of helminth co-infection in HIV-1 infected individuals in resource-limited settings. Cochrane Database Syst Rev 2008;CD006419.
Walson J, Singa B, Sangare L, Naulikha J, Piper B, Richardson B, et al. Empiric deworming to delay HIV disease progression in adults with HIV who are ineligible for initiation of antiretroviral treatment (the HEAT study): a multi-site, randomised trial. Lancet Infect Dis. 2012;12:925–32.
Yazdanbakhsh M, Kremsner PG, van Ree R. Allergy, parasites, and the hygiene hypothesis. Science. 2002;296:490–4.
Erb KJ. Helminths, allergic disorders and IgE-mediated immune responses: where do we stand? Eur J Immunol. 2007;37:1170–3.
Mpairwe H, Ndibazza J, Webb EL, Nampijja M, Muhangi L, Apule B, et al. Maternal hookworm modifies risk factors for childhood eczema: results from a birth cohort in Uganda. Pediatr Allergy Immunol. 2014;25:481–8.
Leonardi-Bee J, Pritchard D, Britton J. Asthma and current intestinal parasite infection: systematic review and meta-analysis. Am J Respir Crit Care Med. 2006;174:514–23.
Ponte EV, Rasella D, Souza-Machado C, Stelmach R, Barreto ML, Cruz AA. Reduced asthma morbidity in endemic areas for helminth infections: a longitudinal ecological study in Brazil. J Asthma;2014:1–6.
Correale J, Farez MF. The impact of parasite infections on the course of multiple sclerosis. J Neuroimmunol. 2011;233:6–11.
Hotez P. Enlarging the “Audacious Goal”: elimination of the world’s high prevalence neglected tropical diseases. Vaccine. 2011;29 Suppl 4:D104–10.
Keiser J, Utzinger J. Efficacy of current drugs against soil-transmitted helminth infections: systematic review and meta-analysis. JAMA. 2008;299:1937–48.
Adegnika AA, Zinsou JF, Issifou S, Ateba-Ngoa U, Kassa RF, Feugap EN, et al. Randomized, controlled, assessor-blind clinical trial to assess the efficacy of single- versus repeated-dose albendazole to treat Ascaris lumbricoides, Trichuris trichiura, and hookworm infection. Antimicrob Agents Chemother. 2014;58:2535–40. Excellent recent randomized, controlled study that reports the efficacy of the most commonly used agent for mass drug administration programs.
Albonico M, Bickle Q, Ramsan M, Montresor A, Savioli L, Taylor M. Efficacy of mebendazole and levamisole alone or in combination against intestinal nematode infections after repeated targeted mebendazole treatment in Zanzibar. Bull World Health Organ. 2003;81:343–52.
Demeler J, Kruger N, Krucken J, von der Heyden VC, Ramunke S, Kuttler U, et al. Phylogenetic characterization of beta-tubulins and development of pyrosequencing assays for benzimidazole resistance in cattle nematodes. PLoS One. 2013;8:e70212.
Diawara A, Halpenny CM, Churcher TS, Mwandawiro C, Kihara J, Kaplan RM, et al. Association between response to albendazole treatment and beta-tubulin genotype frequencies in soil-transmitted helminths. PLoS Negl Trop Dis. 2013;7:e2247.
Soukhathammavong PA, Sayasone S, Phongluxa K, Xayaseng V, Utzinger J, Vounatsou P, et al. Low efficacy of single-dose albendazole and mebendazole against hookworm and effect on concomitant helminth infection in Lao PDR. PLoS Negl Trop Dis. 2012;6:e1417.
Albonico M, Smith PG, Ercole E, Hall A, Chwaya HM, Alawi KS, et al. Rate of reinfection with intestinal nematodes after treatment of children with mebendazole or albendazole in a highly endemic area. Trans R Soc Trop Med Hyg. 1995;89:538–41.
Yap P, Du ZW, Wu FW, Jiang JY, Chen R, Zhou XN, et al. Rapid re-infection with soil-transmitted helminths after triple-dose albendazole treatment of school-aged children in Yunnan, People’s Republic of China. Am J Trop Med Hyg. 2013;89:23–31.
WHO: preventive chemotherapy in human helminthiasis. Coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. Geneva: World Health Organization; 2006.
Gyorkos TW, Gilbert NL, Larocque R, Casapia M. Trichuris and hookworm infections associated with anaemia during pregnancy. Trop Med Int Health. 2011;16:531–7.
Thein H, Thane T, Than S, Myat Lay K, Myint L. A controlled chemotherapeutic intervention trial on the relationship between Ascaris lumbricoides infection and malnutrition in children. Trans R Soc Trop Med Hyg. 1991;85:523–8.
Hotez PJ, Diemert D, Bacon KM, Beaumier C, Bethony JM, Bottazzi ME, et al. The human hookworm vaccine. Vaccine. 2013;31 Suppl 2:B227–32. Update on the development of a vaccine for hookworm infection due to Necator americanus.
Speich B, Ame SM, Ali SM, Alles R, Huwyler J, Hattendorf J, et al. Oxantel pamoate-albendazole for Trichuris trichiura infection. N Engl J Med. 2014;370:610–20. Randomized, double-blind trial demonstrating significant improvement in cure rate of T. trichiura with addition of oxantel pamoate to albendazole.
Knopp S, Mohammed KA, Speich B, Hattendorf J, Khamis IS, Khamis AN, et al. Albendazole and mebendazole administered alone or in combination with ivermectin against Trichuris trichiura: a randomized controlled trial. Clin Infect Dis. 2010;51:1420–8.
Somvanshi VS, Ellis BL, Hu Y, Aroian RV. Nitazoxanide: nematicidal mode of action and drug combination studies. Mol Biochem Parasitol. 2014;193:1–8.
Speich B, Ame SM, Ali SM, Alles R, Hattendorf J, Utzinger J, et al. Efficacy and safety of nitazoxanide, albendazole, and nitazoxanide-albendazole against Trichuris trichiura infection: a randomized controlled trial. PLoS Negl Trop Dis. 2012;6:e1685.
Zumaquero-Rios JL, Sarracent-Perez J, Rojas-Garcia R, Rojas-Rivero L, Martinez-Tovilla Y, Valero MA, et al. Fascioliasis and intestinal parasitoses affecting schoolchildren in Atlixco, Puebla State, Mexico: epidemiology and treatment with nitazoxanide. PLoS Negl Trop Dis. 2013;7:e2553.
Webster JP, Molyneux DH, Hotez PJ, Fenwick A. The contribution of mass drug administration to global health: past, present and future. Philos Trans R Soc Lond B Biol Sci. 2014;369:20130434. Summary of trends in mass drug administration, particularly the integration of different vertical programs that target various neglected tropical diseases.
Mohammed KA, Haji HJ, Gabrielli AF, Mubila L, Biswas G, Chitsulo L, et al. Triple co-administration of ivermectin, albendazole and praziquantel in Zanzibar: a safety study. PLoS Negl Trop Dis. 2008;2:e171.
Coulibaly YI, Dicko I, Keita M, Keita MM, Doumbia M, Daou A, et al. A cluster randomized study of the safety of integrated treatment of trachoma and lymphatic filariasis in children and adults in Sikasso, Mali. PLoS Negl Trop Dis. 2013;7:e2221.
Qian MB, Yap P, Yang YC, Liang H, Jiang ZH, Li W, et al. Efficacy and safety of tribendimidine against Clonorchis sinensis. Clin Infect Dis. 2013;56:e76–82.
Basanez MG, McCarthy JS, French MD, Yang GJ, Walker M, Gambhir M, et al. A research agenda for helminth diseases of humans: modelling for control and elimination. PLoS Negl Trop Dis. 2012;6:e1548.
Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC. Water, sanitation, hygiene, and soil-transmitted helminth infection: a systematic review and meta-analysis. PLoS Med. 2014;11:e1001620. Excellent systematic review demonstrating reduced likelihood of intestinal helminth infection with improvements in water, sanitation and hygiene.
Ziegelbauer K, Speich B, Mausezahl D, Bos R, Keiser J, Utzinger J. Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLoS Med. 2012;9:e1001162.
Xiao SH, Utzinger J, Tanner M, Keiser J, Xue J. Advances with the Chinese anthelminthic drug tribendimidine in clinical trials and laboratory investigations. Acta Trop. 2013;126:115–26.
Hu Y, Platzer EG, Bellier A, Aroian RV. Discovery of a highly synergistic anthelmintic combination that shows mutual hypersusceptibility. Proc Natl Acad Sci U S A. 2010;107:5955–60.
Urban Jr JF, Hu Y, Miller MM, Scheib U, Yiu YY, Aroian RV. Bacillus thuringiensis-derived Cry5B has potent anthelmintic activity against Ascaris suum. PLoS Negl Trop Dis. 2013;7:e2263. Description of a new investigational anthelminthic agent with activity against intestinal nematodes.
Hu Y, Zhan B, Keegan B, Yiu YY, Miller MM, Jones K, et al. Mechanistic and single-dose in vivo therapeutic studies of Cry5B anthelmintic action against hookworms. PLoS Negl Trop Dis. 2012;6:e1900.
Lecova L, Stuchlikova L, Prchal L, Skalova L. Monepantel: the most studied new anthelmintic drug of recent years. Parasitology 2014:1–13.
Diemert DJ, Pinto AG, Freire J, Jariwala A, Santiago H, Hamilton RG, et al. Generalized urticaria induced by the Na-ASP-2 hookworm vaccine: implications for the development of vaccines against helminths. J Allergy Clin Immunol. 2012;130:169–76.
Hotez PJ, Bethony JM, Diemert DJ, Pearson M, Loukas A. Developing vaccines to combat hookworm infection and intestinal schistosomiasis. Nat Rev Microbiol. 2010;8:814–26.
Zhan B, Beaumier CM, Briggs N, Jones KM, Keegan BP, Bottazzi ME, et al. Advancing a multivalent ‘Pan-anthelmintic’ vaccine against soil-transmitted nematode infections. Exp Rev Vaccines. 2014;13:321–31.
Dixon H, Johnston CE, Else KJ. Antigen selection for future anti-Trichuris vaccines: a comparison of cytokine and antibody responses to larval and adult antigen in a primary infection. Parasite Immunol. 2008;30:454–61.
Acknowledgments
DD is supported by grants from the European Commission FP-7 Programme and the Sabin Vaccine Institute. The latter receives funding from the Bill & Melinda Gates Foundation and the Dutch Ministry of Foreign Affairs to develop a human hookworm vaccine.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Paul Blair and David Diemert have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by either of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Intra-abdominal Infections, Hepatitis, and Gastroenteritis
Rights and permissions
About this article
Cite this article
Blair, P., Diemert, D. Update on Prevention and Treatment of Intestinal Helminth Infections. Curr Infect Dis Rep 17, 12 (2015). https://doi.org/10.1007/s11908-015-0465-x
Published:
DOI: https://doi.org/10.1007/s11908-015-0465-x