Purpose of Review
Chronic kidney disease and end-stage kidney disease (ESKD) are well-established risk factors for cardiovascular disease (CVD), the leading cause of mortality in the dialysis population. Conventional therapies, such as statins, blood pressure control, and renin-angiotensin-aldosterone system blockade, have inadequately addressed this cardiovascular risk, highlighting the unmet need for effective treatment strategies. Sodium–glucose transporter 2 (SGLT2) inhibitors have demonstrated significant renal and cardiovascular benefits among patients with type 2 diabetes, heart failure, or CKD at risk of progression. Unfortunately, efficacy data in dialysis patients is lacking as ESKD was an exclusion criterion for all major clinical trials of SGLT2 inhibitors. This review explores the potential of SGLT2 inhibitors in improving cardiovascular outcomes among patients with ESKD, focusing on their direct cardiac effects.
Recent Findings
Recent clinical and preclinical studies have shown promising data for the application of SGLT2 inhibitors to the dialysis population. SGLT2 inhibitors may provide cardiovascular benefits to dialysis patients, not only indirectly by preserving the remaining kidney function and improving anemia but also directly by lowering intracellular sodium and calcium levels, reducing inflammation, regulating autophagy, and alleviating oxidative stress and endoplasmic reticulum stress within cardiomyocytes and endothelial cells.
Summary
This review examines the current clinical evidence and experimental data supporting the use of SGLT2 inhibitors, discusses its potential safety concerns, and outlines ongoing clinical trials in the dialysis population. Further research is needed to evaluate the safety and effectiveness of SGLT2 inhibitor use among patients with ESKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) and end-stage kidney disease (ESKD) are associated with an increased risk of CVD and mortality. CKD has the bidirectional relationship with cardiovascular disease (CVD). The manifestations of CVD in CKD can be broadly classified as myocardial remodeling (i.e., left ventricular hypertrophy, systolic and diastolic dysfunction) and vascular remodeling (i.e., atherosclerosis, arteriosclerosis, vascular calcification), which interact with each other [1]. CVD is the leading cause of mortality in the dialysis population, accounting for 45% of all deaths. The prevalence of coronary heart disease, heart failure, and left ventricular hypertrophy is reported as high as 40%, 43%, and 70%, respectively [2, 3]. Particularly, heart failure poses a significant challenge in the management of ESKD. It frequently develops after initiation of dialysis and is a prominent mortality risk factor among these patients [4]. Traditional therapies to prevent CVD complications in the general population have shown to be ineffective in CKD. To address the unmet need, further research is needed to evaluate novel therapeutic strategies to improve cardiovascular outcomes among patients on dialysis.
Sodium-glucose transporter type 2 (SGLT2) inhibitors have been shown to confer substantial kidney and cardiovascular benefits among patients with type 2 diabetes, heart failure, and/or high-risk CKD [5, 6]. In the current clinical landscape, SGLT2 inhibitors can be initiated among patients with eGFR 20 ml/min/1.73 m2 or more but need to be discontinued upon dialysis initiation for EKSD [7]. This practice likely stems from the diminished efficacy of SGLT2 inhibitors in promoting glucosuria and natriuresis as kidney function declines [8, 9], coupled with undetermined safety profiles among patients with advanced CKD or ESKD who were historically excluded from pivotal clinical trials. Nevertheless, recent emerging data indicate that SGLT2 inhibitors may provide cardiovascular benefits even among dialysis-dependent patients with low or absent kidney function. This evolving perspective may gain momentum now that the Food and Drug Administration (FDA) has removed dialysis dependency from the list of contraindications in the drug labels of SGLT2 inhibitors in 2023, after a multi-discipline review acknowledging the current data and evolution in the understanding of this class of agents [10, 11].
This article aims to comprehensively review the hypothesized clinical advantages, their postulated pathways, and potential safety issues associated with the use of SGLT2 inhibitors in ESKD, with a special focus on heart failure. Additionally, we outline ongoing clinical trials of this drug class in the dialysis population.
Current Clinical Evidence of SGLT2 Inhibitors among Non-Dialysis Patients
Sodium-glucose transporter type 2 (SGLT2) inhibitors are initially approved by the FDA for the management of type 2 diabetes. SGLT2 is mainly expressed in the kidneys, specifically in the apical membrane of the S1 and S2 segments of the proximal tubule. SGLT2 inhibitors induce glycosuria and natriuresis by inhibiting sodium and glucose reabsorption, leading to improved glycemic control, small reduction in blood pressure, and mild to modest weight loss among patients with type 2 diabetes [12, 13]. Interestingly, unlike traditional diuretics, SGLT2 inhibitor-induced diuresis is associated with fewer electrolyte abnormalities, a decreased risk of acute kidney injury, and less neurohormonal activation [8]. Additionally, SGLT2 inhibitor use lowers the risk of hyperkalemia [14], thereby facilitating the continuation of the combined regimen with renin-angiotensin-aldosterone system inhibitors [15]. Beyond the renal effects of glycosuria and natriuresis, SGLT2 inhibitors also offer broad metabolic benefits, including reduction in visceral, liver, and epicardial fat by shifting substrate utilization from carbohydrates to lipids and ketone bodies [16,17,18,19,20], decreased serum uric acid levels and lowered risk of gout flares via enhanced renal uric acid excretion [21, 22], reduced kidney stone formation by increasing urine citrate levels [23,24,25,26], and alleviation of anemia by increasing erythropoietin production and suppressing proinflammatory pathways [27]. Cardiovascular outcome trials revealed that SGLT2 inhibition among patients with type 2 diabetes reduced the risk of cardiovascular events, cardiovascular mortality, and all-cause mortality, with consistency of favorable heart failure and kidney outcomes across the drug class [5, 6].
It should be noted that SGLT2 inhibitors are the first drug class that has shown clear efficacy on clinical hard endpoints in both heart failure with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF). Furthermore, recent clinical trials have shown promising cardiac benefits of the drug regardless of diabetes status [28,29,30,31,32,33,34]. Additionally, recent meta-analyses of clinical trials showed that SGLT2 inhibitor use is associated with a lower risk of atrial fibrillation/flutter events [35, 36]. Observational studies suggest that SGL2 inhibitors may stabilize atherosclerotic plaque among patients with type 2 diabetes and ischemic heart disease [37, 38], thereby reducing major adverse cardiovascular events [39, 40], but meta-analyses showed their neutral effects on stroke or myocardial infarction [41, 42].
While SGLT inhibitors lead to improved glycemic control, better blood pressure management, and weight reduction, these factors alone do not fully explain the extensive cardiac benefits conferred by this drug class. Given the close relationship between the severity of CKD and the increased risk of CVD, the renoprotective effect of SGLT2 inhibitors is considered to play a significant role. This perspective is supported by multiple clinical trials demonstrating reduced albuminuria and a lowered risk of CKD progression by SLGT2 inhibition, benefits that are evident in both diabetic and non-diabetic patient populations [7, 43].
Potential Cardiovascular Benefits of SGLT2 Inhibitors among Dialysis Patients
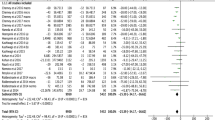
Urinary glucose excretion induced by SGLT2 inhibitors linearly diminishes with lower kidney function [44], and their plasma glucose-lowering effect is attenuated in patients with eGFR < 60 ml/min per 1.73 m2 and becomes negligible when eGFR is < 30 ml/min per 1.73 m2 [45]. Nevertheless, the benefits of SGLT2 inhibitors in kidney and cardiovascular outcomes are generally preserved among patients with CKD and are observed even among non-diabetic patients. For instance, the DAPA-CKD trial showed that dapagliflozin reduced the risk of kidney, cardiovascular and mortality endpoints even in a subgroup of patients with stage 4 CKD, which was consistent with those observed in the entire study [29, 46]. The EMPA-KIDNEY trial also demonstrated that empagliflozin significantly reduced the risk of CKD progression or cardiovascular death across eGFR levels extending to stage 4 CKD [47]. Such kidney function-independent benefits were confirmed in a recent meta-analysis of over 90,000 participants from randomized, placebo-controlled clinical trials [48]. Interestingly, the most substantial risk reduction for heart failure outcomes was observed among patients with lower eGFR levels. Collectively, these findings warrant clinical studies evaluating the effects of SGLT2 inhibitors on cardiovascular outcomes among dialysis patients, where these drugs may provide indirect and direct cardiovascular benefits (Fig. 1).
Potential direct and indirect cardiovascular benefit of SGLT2 inhibitors in the dialysis population. Potential indirect benefits include preservation of kidney function, which can lead to multiple benefits from various aspects including uremic toxin levels, volume and blood pressure (BP) control, and nutrition. SGLT2 inhibitors also improve anemia and iron utilization, leading to less requirement of erythropoietin stimulating agents (ESAs), which is known to increase the risk of cardiovascular events. SGLT2 inhibitors also directly act on cardiomyocytes and endothelial cells and lower intracellular sodium and calcium level, reduce inflammation, mitigate oxidative stress and endoplasmic reticulum (ER) stress, and regulate autophagy. Created using BioRender.com
Indirect Cardiovascular Benefits of SGLT2 Inhibitors
Recent clinical studies have shown that residual kidney function, even at such low levels observed among dialysis patients, is closely associated with better clinical outcomes. In addition to better clearance of uremic toxins, greater residual kidney function is associated with less inflammation, better quality of life, fewer episodes of intradialytic hypotension, better nutritional status, more effective control of phosphorus, less pill burden, less requirement of erythropoietin stimulating agents (ESAs), a lower risk of cardiovascular events, and a lower risk of death [49,50,51,52,53,54]. . The majority of incident ESKD patients still have some kidney function, with approximately 27% and 10% starting dialysis with an eGFR of 10–14 ml/min/1.73 m2 and ≥ 15 ml/min/1.73 m2, respectively [4]. SGLT2 inhibitors slows the progression of CKD, and hence, may help preserve residual kidney function even after dialysis initiation. This in turn could lower the risk of CVD including heart failure.
An additional indirect cardiovascular benefit of SGLT2 inhibitors is the mitigation of anemia and the improvement in iron utilization. Clinical trials have shown that these drugs can increase hematocrit levels by 1.9–2.4%, reduce the risk of developing anemia, and decrease the likelihood of needing iron supplements or ESA treatment [27, 55,56,57,58,59]. These effects are attributed to stimulation of ESA production and reduced hepcidin production by decreasing inflammation and activating nutrient deprivation signaling such as sirtuin-1 in the liver [60]. Notably, this benefit on anemia was consistently observed in moderate-to-severe CKD, where kidney erythropoietin production is impaired [55]. It is postulated that the activation of sirtuin-1 activation by SGLT2 inhibitors could stimulate hypoxia-inducible factor (HIF)-2α, leading to erythropoietin production in the liver [61]. Furthermore, unlike HIF prolyl hydroxylase inhibitors (HIF-PHI), experimental studies have shown that SGLT2 inhibitors suppressed the expression and activity of HIF-1α [62,63,64,65,66], albeit with some exceptions [67, 68]. This distinction could be an important property of this drug class because while HIF-1α does not significantly contribute to endogenous erythropoietin synthesis, it may enhance atherosclerotic plaque instability and promote cardiac fibrosis [69]. Additionally, HIF-2α stimulation by SGLT2 inhibitor use has been also reported in in vitro studies [70,71,72], indicating this effect is partly independent of glucosuria. Given the increased cardiovascular risk associated with ESA therapy with or HIF-PHI inhibitor [73], and considering the high prevalence and associated mortality risk of functional iron deficiency [74], SGLT2 inhibitors could become an attractive alternative in the management of anemia in the dialysis population.
Direct Cardiovascular Benefits of SGLT2 Inhibitors
Recent preclinical and translational research has provided data supporting direct benefits of SGLT2 inhibitors on the cardiovascular system, including cardiomyocytes, endothelial cells, and smooth muscle cells. Experimental studies using ex vivo isolated perfused hearts showed that empagliflozin mitigated ischemia-reperfusion injury and improved cardiac output, contractile dysfunction, and ventricular arrhythmia vulnerability [75, 76]. Given the minimal SGLT2 expression in the heart [77, 78], extensive research has been conducted to identify the mechanisms behind the direct cardiovascular effects of SGLT2 inhibitors. First, several clinical studies revealed increased SGLT2 expression in endomyocardial biopsy samples from patients with various heart conditions [79,80,81]. Second, molecular docking analysis indicated that empagliflozin could bind with other glucose transporters (i.e., facilitated-diffusion glucose transporters [GLUT], SGLT1, and NHE) with much higher affinity for GLUT1 and GLUT4 compared with SGLT1 and NHE [76]. It should also be noted that SGLT2 inhibitors have variable selectivity for SGLT2 vs. SGLT1, i.e., 2500× selectivity for empagliflozin, 1200× selectivity for dapagliflozin, 250× selectivity for canagliflozin, and 20x selectivity for sotagliflozin [82], and less selective SGLT2 inhibitors was associated with a lower risk of heart failure in network meta-analyses [83, 84]. Third, in vitro studies using cardiomyocytes have shown that SGLT2 inhibitors elicit cellular responses without glucose in the medium [85], suggesting glucose transporter-independent mechanisms. The exact pathways of the direct cardioprotective effects of SGLT2 inhibitors remain to be fully elucidated but appear to involve various processes in the pathophysiology of heart failure, such as regulation of intracellular electrolytes, inflammation, oxidative stress, mitochondrial function, and autophagic flux [24, 86] (Fig. 2).
Potential pathways of direct cardiovascular benefits via SGLT2 inhibitor use. SGLT2 inhibitors can prevent or improve cardiac dysfunction and remodeling by lowering intracellular sodium and calcium levels, reducing oxidative and endoplasmic reticulum (ER) stress, suppressing the inflammatory process, and regulating autophagy. These mechanisms are interrelated. Created using BioRender.com
-
1.
Intracellular electrolyte regulation.
Increases in myocardial intracellular sodium and calcium levels, coupled with a subsequent decrease in mitochondrial calcium levels, are recognized as early hallmarks and contributors of cardiovascular death and heart failure [86, 87]. Several preclinical studies have shown that SGLT2 inhibitors can counteract these adverse changes by directly inhibiting sodium-hydrogen exchanger 1 (NHE-1) in cardiomyocytes and endothelial cells [85,86,87,88]. This inhibition leads to reduced intracellular sodium levels, followed by a decrease in intracellular calcium levels alongside an increase in mitochondrial calcium levels, likely through the action of sodium-calcium exchangers. SGLT2 inhibitors also inhibit hydrogen peroxide-induced late sodium current in cardiomyocytes with little effect on peak sodium current, which may protect against arrhythmias associated with prolonged action potentials [75, 89].
Of note, a phase III randomized, placebo-controlled clinical trial evaluated the effect of NHE-1 inhibition by cariporide among 5761 patients undergoing high-risk coronary artery bypass graft surgery and found that cariporide significantly reduced the incidence of myocardial infarction but increased mortality from cerebrovascular events [90]. SGLT2 inhibitors may have an advantage on this regard because their use has been shown to have neutral effect on overall cerebrovascular events [41, 42]. However, the direct NHE-1 inhibition by SGLT2 inhibitors were not consistently observed in other studies [91,92,93], indicating the presence of unknown effect modifying factors.
-
2.
Oxidative stress and inflammation.
Oxidative stress and inflammation are interdependently involved in the pathogenesis of CVD, perpetuating a chronic and vicious cycle with heart failure. Oxidative stress, caused by reactive oxygen species (ROS), induces the inflammation pathway through the activation of nucleotide-binding domain, Leucine-rich-containing family, pyrin domain-containing-3 (NLRP3) inflammasome [94]. The subsequent release of inflammatory cytokines, if excessive, can lead to inflammatory cell death, known as pyroptosis [95]. In turn, inflammation also induces oxidative stress via various cellular signaling pathways involving mediators such as protein kinase C and calcium. These mediators activate sources of reactive oxygen species (ROS) such as nicotinamide adenine dinucleotide phosphate (NADPH) oxidase and the mitochondrial electron transport chain. Chronic inflammation and oxidative stress promote proinflammatory macrophage infiltration and augment interstitial collagen deposition, which creates areas of replacement fibrosis, eventually leading to progressive left ventricular remodeling and dysfunction [96, 97]. ROS reduces nitric oxide-cyclic guanosine monophosphate-protein kinase G (NO-cGMP-PKG) signaling, leading to myocardial hypertrophy and increased stiffness by diminishing myofilament phosphorylation [98]. Proinflammatory macrophage infiltration and decreased NO production in the endothelial cells play a significant role in the progression of atherosclerosis [99].
In the myocardium of HFrEF, myocardial injury or death is triggered by oxidative stress from various stimuli such as ischemia, pressure overload, or toxicity, followed by inflammatory responses. Activation of sympathetic nervous system and renin-angiotensin-aldosterone system can also induce sustained myocardial inflammation [100]. Conversely, among patients with HFpEF, comorbid conditions such as aging, overweight/obesity, diabetes, sleep apnea, atherosclerotic disease, and smoking/chronic obstructive pulmonary disease are commonly present and known to cause chronic and systemic inflammation, which then induces oxidative stress [96, 97].
SGLT2 inhibitors have been shown to reduce the expression of various circulating inflammatory molecules (e.g., Interleukin [IL]-1β, IL-6, and IL-18, tumor necrosis factor-α [TNF-α], monocyte chemoattractant protein-1 [MCP-1]) and cell adhesion molecules across different studies [101, 102]. Potential mechanisms underlying the anti-inflammatory effects of SGLT2 inhibitors include the reduction in intracellular calcium levels via NHE-1 inhibition and activation of 5’ adenosine monophosphate-activated protein kinase (AMPK), both leading to the suppression of the NLRP3 inflammasome activation [103]. In murine models of doxorubicin-induced cardiomyopathy, empagliflozin reduced ferroptpsis, fibrosis, apoptosis, and inflammation through the involvement of NLRP3 and myddosome-related pathways, leading to improved cardiac functions [104]. Additionally, empagliflozin was shown to suppress the increase in the expression of proinflammatory makers induced by doxorubicin in vitro.
The cardiovascular benefits of SGLT2 inhibitors are further seen through oxidative stress reduction. For instance, empagliflozin attenuated cardiomyocyte hypertrophy, diminished interstitial fibrosis, and reduced myocardial oxidative stress in non-diabetic rats with left ventricular dysfunction post-myocardial infarction [105]. Furthermore, in an in vitro study, empagliflozin restored the endothelium-mediated cardiomyocyte relaxation and contraction, which was impaired due to decreased nitric oxide availability and increased mitochondrial ROS following exposure to uremic serum from patients with ESKD [106]. Such anti-inflammatory and anti-oxidative properties of SGLT2 inhibitors can also lead to improvements in endothelial function and arterial wall stiffness as shown in both animal and clinical models [92, 107, 108] and may mitigate the development of cardiac fibrosis and atherosclerosis by inhibiting macrophage infiltration, reducing foam cell formation, and promoting macrophage polarization from pro-inflammatory M1 subtype to anti-inflammatory M2 subtype [38, 101, 109, 110].
-
3.
Autophagy Regulation.
Autophagy-lysosome pathway is primarily a catabolic process that maintains cellular homeostasis. It captures misfolded proteins, damaged organelles, and pathogens in autophagosomes for degradation by lysosomal proteases [111]. This process plays an important role in facilitating metabolic adaptation, preventing cellular damage, and preserving genomic stability. This catabolic process is activated in response to various stressors—such as shear stress, hypoxia, ischemia, and mitochondrial damage—via crucial signaling networks such as mTOR, AMPK, glycogen synthase kinase 3 beta (GSK-3β), and the Hippo pathway [112]. Impaired autophagy can contribute to the accumulation of cellular debris, dysfunctional mitochondria, and NLRP3 inflammasome activators and components, leading to cellular stress and inflammation [113]. Autophagy is particularly important for cardiomyocytes, the terminally differentiated cells that infrequently undergo cell division.
While essential for cardiac function and limiting disease progression post-injury, an imbalance in autophagy levels—either suppression or excessive activation—can lead to or exacerbate pathological outcomes [114]. For instance, autophagy plays an adaptive role in progressive heart failure and protects myocardial cells, and autophagy activity was associated with left ventricular reverse remodeling among patients with dilated cardiomyopathy [80]. In the late period of heart failure, however, substances and injury myocardial cells can be overly removed via autophagic pathway. Excessive autophagy activation may also occur with pressure overload or ischemia/reperfusion injury [115,116,117]. Therefore, maintaining an “optimal window” of autophagy activity according to disease conditions is crucial for cellular homeostasis [114].
SGLT2 inhibitors have been shown to “modulate” cardiac autophagy and lysosomal degradation. These drugs promote autophagy through glucosuria-induced upregulation of nutrient deprivation signals such as AMPK, sirtuins, and peroxisome proliferator–activated receptor-γ coactivator (PGC)-1α, while downregulating nutrient surplus signals, including mTOR [118]. Consequently, this contributes to the improvement of mitochondrial morphology, function, and biogenesis in the heart, as shown in several in vivo studies [119, 120]. Another in vivo study showed that empagliflozin ameliorated sunitinib-induced cardiac dysfunction by restoring AMPK-mTOR mediated autophagy in mice [121]. Conversely, Jiang, et al. showed that empagliflozin reduced cardiac infarct size and fibrosis and resulted in improved cardiac function and survival in mouse models and reported that those cardioprotective effects were at least in part through downregulation, not upregulation, of excessive autophagic flux through NHE-1 inhibition [122]. Empagliflozin also inhibited hyperactivation of autophagy in murine diabetic cardiomyopathy by inhibiting GSK-3β, resulting in reversal of cardiac dysfunction [123]. Importantly, such autophagy upregulation via AMPK activation and downregulation via NHE-1 or GSK-3β inhibition were also confirmed in accompanying in vitro studies [121,122,123]. Those findings indicate that the anti-inflammatory and anti-oxidative effects on SGLT2 inhibitors are at least partly independent of their effects on the kidneys (i.e., glucosuria and natriuresis), suggesting a potential role in ESKD.
-
4.
Endoplasmic reticulum stress.
Endoplasmic reticulum (ER) is a critical cellular organelle involved in protein folding and secretion, calcium storage, and lipid and carbohydrate metabolism [124]. ER stress is a response to proteostasis imbalance such as the accumulation of misfolded or unfolded proteins. ER stress-induced inflammation can help limit tissue damage and promote tissue repair; however, the effects of ER stress-induced inflammation depend on the type of ER stressor, the disease stage, and the target cell type [125]. Oxidative stress also occurs alongside ER stress as the misfolded proteins produce ROS during attempts to refold, which disturbs cellular redox balance. This oxidative stress can further exacerbate ER stress, creating a vicious cycle that can lead to cell damage and disease [125, 126]. The disruption in ER homeostasis intricately activates the unfolded protein response (UPR) and autophagy to restore normal function by halting protein translation, degrading misfolded proteins, and activating the signaling pathways that increase the production of molecular chaperones [124, 127].
Recent studies have shown that SGLT2 inhibitors have protective effects against ER stress in cardiomyocytes. Treatment with SGLT2 inhibitors has been shown to reduce the expression of key ER stress markers such as cleaved caspase 3, Bax, activating transcription factor 4, C/EBP homologous protein, and glucose-regulated protein78 in cardiomyocytes exposed to high glucose [128], hydrogen peroxide [129], angiotensin II [130], or doxorubicin [131, 132] in both in vivo and in vitro studies. These findings suggest that SGLT2 inhibitors may directly prevent the initiation of cell death pathways triggered by ER stress in the heart.
Safety Considerations in the Use of SGLT2i in ESKD
Previous pharmacokinetic studies showed that among patients with advanced CKD and ESRD, when compared to those with normal kidney function, a single-dose administration generally resulted in similar peak plasma levels, a mildly prolonged half-life time, and approximately 1.5-times larger AUC [133]. There appeared to be no clinically meaningful difference in those pharmacokinetic parameters from stage 4 CKD through ESRD. Additionally, 7 days of dapagliflozin 10 mg/day among dialysis patients resulted in no significant drug accumulation but peak concentrations similar to those observed among the age- and sex-matched control patients with normal kidney function [134].
From a clinical safety standpoint, the EMPA-REG Renal trial showed the risk of mild to moderate urinary tract infection associated with empagliflozin use was more pronounced among patients with more advanced CKD (i.e., 18.9% in the empagliflozin group vs. 8.1% in the placebo group in stage 4 CKD; no acute pyelonephritis or urosepsis was reported) [135]. This warrants caution in the use of SGLT2 inhibitors among oliguric dialysis patients. However, in the DAPA-CKD trial, dapagliflozin did not show increased risk of adverse events across subgroups including CKD stage 4, despite continuation of dapagliflozin even when eGFR declined to < 15 ml/min per 1.73m2 [46].
Ongoing Clinical Trials
Several clinical trials are underway to investigate the effects of SGLT2 inhibitors in the dialysis population (Table 1). Such trials registered in CliniclTrials.gov include RENAL LIFECYCLES (NCT05374291), DAPA-HD (NCT05179668), and SIP-AkiD (NCT05309785). RENAL LIFECYCLES aims to enroll 1500 patients with either advanced CKD (eGFR < 25 ml/min per 1.73 m2), ESKD requiring dialysis with residual diuresis > 500 ml/day, or transplant kidney allograft with eGFR < 25 ml/min per 1.73 m2 and to evaluate a composite endpoint of hard clinical outcomes, i.e., all-cause mortality, kidney failure, and hospitalization for heart failure. Many other studies have cardiac imaging parameters or brain natriuretic peptide levels as the primary outcomes. New trials include CANARY (NCT05715814), CARe-MRI (NCT06182839), SEED (NCT05786443), EMPA-PRED (NCT06249945), and EMPA-RRED (NCT06249932) which are expected to begin early 2024. The results of these trials are expected to provide proof-of-concept evidence on the efficacy and safety of SGLT2 inhibitors, a potentially important step towards the better management of cardiovascular disease among dialysis patients.
Conclusions
The pleiotropic effects of SGLT2 inhibitors, including their benefits on preserving kidney function and improving cardiovascular health, make this drug class a promising therapeutic agent in the management of dialysis patients with ESKD. Clinical trials have demonstrated the cardiovascular benefits of SGLT2 inhibitors even among patients with advanced CKD, where its primary glycosuric effect is substantially diminished. Additionally, preclinical studies suggest potential direct actions of SGLT2 inhibitors in the cardiovascular system, where SGLT2 expression is minimal or negligible. These findings underscore the potential of SGLT2 inhibitors in preventing cardiovascular complications among dialysis patients. Ongoing pilot clinical trials are expected to provide preliminary results to evaluate whether larger clinical trials would be warranted from both safety and efficacy standpoint.
Data Availability
No datasets were generated or analysed during the current study.
References
Jankowski J, Floege J, Fliser D, Bohm M, Marx N. Cardiovascular Disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157–72.
Cozzolino M, Galassi A, Pivari F, Ciceri P, Conte F. The Cardiovascular Burden in End-Stage Renal Disease. Contrib Nephrol. 2017;191:44–57.
House AA, Wanner C, Sarnak MJ, Pina IL, McIntyre CW, Komenda P, et al. Heart failure in chronic kidney disease: conclusions from a kidney disease: improving global outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95(6):1304–17.
USE. 2020 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD 2020.
McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, et al. Association of SGLT2 inhibitors with Cardiovascular and kidney outcomes in patients with type 2 diabetes: a Meta-analysis. JAMA Cardiol. 2021;6(2):148–58.
Odutayo A, da Costa BR, Pereira TV, Garg V, Iskander S, Roble F, et al. Sodium-glucose cotransporter 2 inhibitors, all-cause mortality, and Cardiovascular outcomes in adults with type 2 diabetes: a bayesian Meta-analysis and Meta-regression. J Am Heart Assoc. 2021;10(18):e019918.
Kidney Disease. Improving global outcomes CKDWG. KDIGO 2024 Clinical Practice Guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105(4S):S117–314.
Griffin M, Rao VS, Ivey-Miranda J, Fleming J, Mahoney D, Maulion C, et al. Empagliflozin Heart Failure: Diuret Cardiorenal Eff Circulation. 2020;142(11):1028–39.
Thomson SC, Vallon V. Effects of SGLT2 inhibitor and dietary NaCl on glomerular hemodynamics assessed by micropuncture in diabetic rats. Am J Physiol Ren Physiol. 2021;320(5):F761–71.
Center for Drug Evaluation and Research. Approval Package for APPLICATION NUMBER 202293Orig1s026. 2023 [ https://www.accessdata.fda.gov/drugsatfda_docs/nda/2023/202293Orig1s026.pdf
Center for Drug Evaluation and Research. SUPPLEMENT APPROVAL for NDA 204042/S-040. 2023 [ https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2023/204042Orig1s040ltr.pdf
Mazidi M, Rezaie P, Gao HK, Kengne AP. Effect of sodium-glucose Cotransport-2 inhibitors on blood pressure in people with type 2 diabetes Mellitus: a systematic review and Meta-analysis of 43 randomized control trials with 22 528 patients. J Am Heart Assoc. 2017;6(6).
Teo YH, Teo YN, Syn NL, Kow CS, Yoong CSY, Tan BYQ, et al. Effects of Sodium/Glucose cotransporter 2 (SGLT2) inhibitors on Cardiovascular and metabolic outcomes in patients without diabetes Mellitus: a systematic review and Meta-analysis of randomized-controlled trials. J Am Heart Assoc. 2021;10(5):e019463.
Neuen BL, Oshima M, Agarwal R, Arnott C, Cherney DZ, Edwards R, et al. Sodium-glucose cotransporter 2 inhibitors and risk of Hyperkalemia in people with type 2 diabetes: a Meta-analysis of individual Participant Data from Randomized, controlled trials. Circulation. 2022;145(19):1460–70.
Luo X, Xu J, Zhou S, Xue C, Chen Z, Mao Z. Influence of SGLT2i and RAASi and their combination on risk of Hyperkalemia in DKD: A Network Meta-Analysis. Clin J Am Soc Nephrol. 2023;18(8):1019–30.
Liu X, Chen Y, Liu T, Cai L, Yang X, Mou C. The effects of Sodium-glucose cotransporter 2 inhibitors on adipose tissue in patients with type 2 diabetes: a meta-analysis of randomized controlled trials. Front Endocrinol (Lausanne). 2023;14:1115321.
Wang X, Wu N, Sun C, Jin D, Lu H. Effects of SGLT-2 inhibitors on adipose tissue distribution in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Diabetol Metab Syndr. 2023;15(1):113.
Bechmann LE, Emanuelsson F, Nordestgaard BG, Benn M. SGLT2-inhibition increases total, LDL, and HDL cholesterol and lowers triglycerides: Meta-analyses of 60 randomized trials, overall and by dose, ethnicity, and drug type. Atherosclerosis. 2023:117236.
Szekeres Z, Toth K, Szabados E. The effects of SGLT2 inhibitors on lipid metabolism. Metabolites. 2021;11(2).
Sato T, Aizawa Y, Yuasa S, Kishi S, Fuse K, Fujita S, et al. The effect of dapagliflozin treatment on epicardial adipose tissue volume. Cardiovasc Diabetol. 2018;17(1):6.
Suijk DLS, van Baar MJB, van Bommel EJM, Iqbal Z, Krebber MM, Vallon V, et al. SGLT2 inhibition and uric acid excretion in patients with type 2 diabetes and normal kidney function. Clin J Am Soc Nephrol. 2022;17(5):663–71.
McCormick N, Yokose C, Wei J, Lu N, Wexler DJ, Avina-Zubieta JA, et al. Comparative effectiveness of sodium-glucose Cotransporter-2 inhibitors for recurrent gout flares and gout-primary Emergency Department visits and hospitalizations: a General Population Cohort Study. Ann Intern Med. 2023;176(8):1067–80.
Balasubramanian P, Wanner C, Ferreira JP, Ofstad AP, Elsaesser A, Zinman B, Inzucchi SE. Empagliflozin and decreased risk of Nephrolithiasis: a potential New Role for SGLT2 inhibition? J Clin Endocrinol Metab. 2022;107(7):e3003–7.
Paik JM, Tesfaye H, Curhan GC, Zakoul H, Wexler DJ, Patorno E. Sodium-glucose cotransporter 2 inhibitors and nephrolithiasis risk in patients with type 2 diabetes. JAMA Intern Med. 2024;184(3):265–74.
Harmacek D, Pruijm M, Burnier M, Muller ME, Ghajarzadeh-Wurzner A, Bonny O, Zanchi A. Empagliflozin Changes urine supersaturation by decreasing pH and increasing citrate. J Am Soc Nephrol. 2022;33(6):1073–5.
Bletsa E, Filippas-Dekouan S, Kostara C, Dafopoulos P, Dimou A, Pappa E, et al. Effect of Dapagliflozin on urine metabolome in patients with type 2 diabetes. J Clin Endocrinol Metab. 2021;106(5):1269–83.
Packer M. Alleviation of Anemia by SGLT2 inhibitors in patients with CKD: mechanisms and results of long-term placebo-controlled trials. Clin J Am Soc Nephrol. 2023.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306.
Heerspink HJL, Stefansson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46.
Zannad F, Ferreira JP, Pocock SJ, Zeller C, Anker SD, Butler J, et al. Cardiac and kidney benefits of Empagliflozin in Heart failure across the spectrum of kidney function: insights from EMPEROR-Reduced. Circulation. 2021;143(4):310–21.
Santos-Gallego CG, Vargas-Delgado AP, Requena-Ibanez JA, Garcia-Ropero A, Mancini D, Pinney S, et al. Randomized Trial of Empagliflozin in nondiabetic patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2021;77(3):243–55.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Bohm M, et al. Empagliflozin in Heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61.
Borlaug BA, Reddy YNV, Braun A, Sorimachi H, Omar M, Popovic D, et al. Cardiac and Metabolic effects of Dapagliflozin in Heart failure with preserved ejection fraction: the CAMEO-DAPA trial. Circulation. 2023;148(10):834–44.
Spertus JA, Birmingham MC, Nassif M, Damaraju CV, Abbate A, Butler J, et al. The SGLT2 inhibitor canagliflozin in heart failure: the CHIEF-HF remote, patient-centered randomized trial. Nat Med. 2022;28(4):809–13.
Zheng RJ, Wang Y, Tang JN, Duan JY, Yuan MY, Zhang JY. Association of SGLT2 inhibitors with risk of Atrial Fibrillation and Stroke in patients with and without type 2 diabetes: a systemic review and Meta-analysis of Randomized controlled trials. J Cardiovasc Pharmacol. 2022;79(2):e145–52.
Pandey AK, Okaj I, Kaur H, Belley-Cote EP, Wang J, Oraii A, et al. Sodium-glucose co-transporter inhibitors and Atrial Fibrillation: a systematic review and Meta-analysis of Randomized controlled trials. J Am Heart Assoc. 2021;10(17):e022222.
Kurozumi A, Shishido K, Yamashita T, Sato D, Uchida S, Koyama E, et al. Sodium-glucose Cotransporter-2 inhibitors stabilize coronary plaques in Acute Coronary Syndrome with Diabetes Mellitus. Am J Cardiol. 2024;214:47–54.
Sardu C, Trotta MC, Sasso FC, Sacra C, Carpinella G, Mauro C, et al. SGLT2-inhibitors effects on the coronary fibrous cap thickness and MACEs in diabetic patients with inducible myocardial ischemia and multi vessels non-obstructive coronary artery stenosis. Cardiovasc Diabetol. 2023;22(1):80.
Zhu J, Yu X, Zheng Y, Li J, Wang Y, Lin Y, et al. Association of glucose-lowering medications with cardiovascular outcomes: an umbrella review and evidence map. Lancet Diabetes Endocrinol. 2020;8(3):192–205.
Zheng SL, Roddick AJ, Aghar-Jaffar R, Shun-Shin MJ, Francis D, Oliver N, Meeran K. Association between Use of Sodium-glucose cotransporter 2 inhibitors, glucagon-like Peptide 1 agonists, and Dipeptidyl Peptidase 4 inhibitors with all-cause mortality in patients with type 2 diabetes: a systematic review and Meta-analysis. JAMA. 2018;319(15):1580–91.
Tsai WH, Chuang SM, Liu SC, Lee CC, Chien MN, Leung CH, et al. Effects of SGLT2 inhibitors on stroke and its subtypes in patients with type 2 diabetes: a systematic review and meta-analysis. Sci Rep. 2021;11(1):15364.
Patel SM, Kang YM, Im K, Neuen BL, Anker SD, Bhatt DL et al. Sodium Glucose Co-transporter 2 Inhibitors and Major Adverse Cardiovascular Outcomes: A SMART-C Collaborative Meta-Analysis. Circulation. 2024. •The most comprehensive meta-analysis to date showing that SGLT2 inhibitors reduce the risk of major adverse cardiovascular events irrespective of diabetes, kidney function or other major clinical characteristics at baseline.
Chun KJ, Jung HH. SGLT2 inhibitors and kidney and Cardiac outcomes according to estimated GFR and Albuminuria levels: a Meta-analysis of Randomized controlled trials. Kidney Med. 2021;3(5):732–44. e1.
Hu S, Lin C, Cai X, Zhu X, Lv F, Nie L, Ji L. The urinary glucose excretion by sodium-glucose cotransporter 2 inhibitor in patients with different levels of renal function: a systematic review and Meta-analysis. Front Endocrinol (Lausanne). 2021;12:814074.
Cherney DZI, Cooper ME, Tikkanen I, Pfarr E, Johansen OE, Woerle HJ, et al. Pooled analysis of Phase III trials indicate contrasting influences of renal function on blood pressure, body weight, and HbA1c reductions with empagliflozin. Kidney Int. 2018;93(1):231–44.
Chertow GM, Vart P, Jongs N, Toto RD, Gorriz JL, Hou FF, et al. Effects of Dapagliflozin in Stage 4 chronic kidney disease. J Am Soc Nephrol. 2021;32(9):2352–61.
The E-KCG, Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388(2):117–27.
Maddaloni E, Cavallari I, La Porta Y, Appetecchia A, D’Onofrio L, Grigioni F, et al. Impact of baseline kidney function on the effects of sodium-glucose co-transporter-2 inhibitors on kidney and heart failure outcomes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2023;25(5):1341–50.
Shafi T, Jaar BG, Plantinga LC, Fink NE, Sadler JH, Parekh RS, et al. Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the choices for healthy outcomes in caring for end-stage renal disease (CHOICE) study. Am J Kidney Dis. 2010;56(2):348–58.
Eriguchi R, Obi Y, Streja E, Tortorici AR, Rhee CM, Soohoo M, et al. Longitudinal associations among renal urea clearance-corrected normalized protein Catabolic Rate, serum albumin, and mortality in patients on Hemodialysis. Clin J Am Soc Nephrol. 2017;12(7):1109–17.
Wang M, Obi Y, Streja E, Rhee CM, Lau WL, Chen J, et al. Association of Parameters of Mineral Bone Disorder with mortality in patients on Hemodialysis according to level of residual kidney function. Clin J Am Soc Nephrol. 2017;12(7):1118–27.
Kimura H, Sy J, Okuda Y, Wenziger C, Hanna R, Obi Y, et al. A faster decline of residual kidney function and erythropoietin stimulating agent hyporesponsiveness in incident hemodialysis patients. Hemodial Int. 2021;25(1):60–70.
Obi Y, Rhee CM, Mathew AT, Shah G, Streja E, Brunelli SM, et al. Residual kidney function decline and Mortality in Incident Hemodialysis patients. J Am Soc Nephrol. 2016;27(12):3758–68.
Okazaki M, Obi Y, Shafi T, Rhee CM, Kovesdy CP, Kalantar-Zadeh K. Residual kidney function and cause-specific mortality among Incident Hemodialysis patients. Kidney Int Rep. 2023;8(10):1989–2000.
Koshino A, Schechter M, Chertow GM, Vart P, Jongs N, Toto RD, et al. Dapagliflozin and Anemia in patients with chronic kidney disease. NEJM Evid. 2023;2(6):EVIDoa2300049.
Ferreira JP, Anker SD, Butler J, Filippatos G, Iwata T, Salsali A, et al. Impact of anaemia and the effect of empagliflozin in heart failure with reduced ejection fraction: findings from EMPEROR-Reduced. Eur J Heart Fail. 2022;24(4):708–15.
Docherty KF, Curtain JP, Anand IS, Bengtsson O, Inzucchi SE, Kober L, et al. Effect of dapagliflozin on anaemia in DAPA-HF. Eur J Heart Fail. 2021;23(4):617–28.
Oshima M, Neuen BL, Jardine MJ, Bakris G, Edwards R, Levin A, et al. Effects of canagliflozin on anaemia in patients with type 2 diabetes and chronic kidney disease: a post-hoc analysis from the CREDENCE trial. Lancet Diabetes Endocrinol. 2020;8(11):903–14.
Mazer CD, Hare GMT, Connelly PW, Gilbert RE, Shehata N, Quan A, et al. Effect of Empagliflozin on erythropoietin levels, Iron Stores, and red blood cell morphology in patients with type 2 diabetes Mellitus and Coronary Artery Disease. Circulation. 2020;141(8):704–7.
Packer M. How can sodium-glucose cotransporter 2 inhibitors stimulate erythrocytosis in patients who are iron-deficient? Implications for understanding iron homeostasis in heart failure. Eur J Heart Fail. 2022;24(12):2287–96.
Packer M. Mechanistic and clinical comparison of the Erythropoietic effects of SGLT2 inhibitors and prolyl hydroxylase inhibitors in patients with chronic kidney disease and renal Anemia. Am J Nephrol. 2024;55(2):255–9.
Bessho R, Takiyama Y, Takiyama T, Kitsunai H, Takeda Y, Sakagami H, Ota T. Hypoxia-inducible factor-1alpha is the therapeutic target of the SGLT2 inhibitor for diabetic nephropathy. Sci Rep. 2019;9(1):14754.
Cai T, Ke Q, Fang Y, Wen P, Chen H, Yuan Q, et al. Sodium-glucose cotransporter 2 inhibition suppresses HIF-1alpha-mediated metabolic switch from lipid oxidation to glycolysis in kidney tubule cells of diabetic mice. Cell Death Dis. 2020;11(5):390.
Wang YH, Chang DY, Zhao MH, Chen M. Dapagliflozin alleviates Diabetic kidney Disease via Hypoxia Inducible Factor 1alpha/Heme oxygenase 1-Mediated ferroptosis. Antioxid Redox Signal. 2024;40(7–9):492–509.
Li J, Liu H, Takagi S, Nitta K, Kitada M, Srivastava SP et al. Renal protective effects of empagliflozin via inhibition of EMT and aberrant glycolysis in proximal tubules. JCI Insight. 2020;5(6).
Huang X, Guo X, Yan G, Zhang Y, Yao Y, Qiao Y, et al. Dapagliflozin attenuates contrast-induced acute kidney Injury by regulating the HIF-1alpha/HE4/NF-kappaB pathway. J Cardiovasc Pharmacol. 2022;79(6):904–13.
Ndibalema AR, Kabuye D, Wen S, Li L, Li X, Fan Q. Empagliflozin protects against proximal renal tubular cell Injury Induced by high glucose via regulation of Hypoxia-Inducible factor 1-Alpha. Diabetes Metab Syndr Obes. 2020;13:1953–67.
Inada A, Inada O, Yasunami Y, Arakawa K, Nabeshima YI, Fukatsu A. Amelioration of Murine Diabetic Nephropathy with a SGLT2 inhibitor is Associated with suppressing abnormal expression of Hypoxia-Inducible factors. Am J Pathol. 2022;192(7):1028–52.
Yang Z, Li T, Xian J, Chen J, Huang Y, Zhang Q, et al. SGLT2 inhibitor dapagliflozin attenuates cardiac fibrosis and inflammation by reverting the HIF-2alpha signaling pathway in arrhythmogenic cardiomyopathy. FASEB J. 2022;36(7):e22410.
He L, Li Y, Zhang D, Song H, Xu D, Song Z. Dapagliflozin improves endothelial cell dysfunction by regulating mitochondrial production via the SIRT1/PGC-1alpha pathway in obese mice. Biochem Biophys Res Commun. 2022;615:123–30.
Faridvand Y, Kazemzadeh H, Vahedian V, Mirzajanzadeh P, Nejabati HR, Safaie N, et al. Dapagliflozin attenuates high glucose-induced endothelial cell apoptosis and inflammation through AMPK/SIRT1 activation. Clin Exp Pharmacol Physiol. 2022;49(6):643–51.
Tian G, Yu Y, Deng H, Yang L, Shi X, Yu B. Empagliflozin alleviates ethanol-induced cardiomyocyte injury through inhibition of mitochondrial apoptosis via a SIRT1/PTEN/Akt pathway. Clin Exp Pharmacol Physiol. 2021;48(6):837–45.
Babitt JL, Eisenga MF, Haase VH, Kshirsagar AV, Levin A, Locatelli F et al. Controversies in optimal anemia management: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Conference. Kidney Int. 2021;99(6):1280-95.
Macdougall IC, White C, Anker SD, Bhandari S, Farrington K, Kalra PA et al. Intravenous Iron in patients undergoing maintenance hemodialysis. N Engl J Med. 2018.
Azam MA, Chakraborty P, Si D, Du B, Masse S, Lai PFH, et al. Anti-arrhythmic and inotropic effects of empagliflozin following myocardial ischemia. Life Sci. 2021;276:119440.
Li X, Lu Q, Qiu Y, do Carmo JM, Wang Z, da Silva AA, et al. Direct cardiac actions of the Sodium glucose co-transporter 2 inhibitor Empagliflozin improve myocardial oxidative phosphorylation and attenuate pressure-overload heart failure. J Am Heart Assoc. 2021;10(6):e018298. •This study provided compelling evidence that empagliflozin, the most selective SGLT2 inhibitor, directly acts on multiple pathways in the heat and attenuates adverse cardiac remodeling and progression of heart failure induced by pressure-overload using ex vivo isolated perfused hearts from non-diabetic mellitus mice.
Chen J, Williams S, Ho S, Loraine H, Hagan D, Whaley JM, Feder JN. Quantitative PCR tissue expression profiling of the human SGLT2 gene and related family members. Diabetes Ther. 2010;1(2):57–92.
Vrhovac I, Balen Eror D, Klessen D, Burger C, Breljak D, Kraus O, et al. Localizations of na(+)-D-glucose cotransporters SGLT1 and SGLT2 in human kidney and of SGLT1 in human small intestine, liver, lung, and heart. Pflugers Arch. 2015;467(9):1881–98.
Marfella R, Scisciola L, D’Onofrio N, Maiello C, Trotta MC, Sardu C, et al. Sodium-glucose cotransporter-2 (SGLT2) expression in diabetic and non-diabetic failing human cardiomyocytes. Pharmacol Res. 2022;184:106448.
Kanamori H, Yoshida A, Naruse G, Endo S, Minatoguchi S, Watanabe T, et al. Impact of autophagy on prognosis of patients with dilated cardiomyopathy. J Am Coll Cardiol. 2022;79(8):789–801.
Mroueh A, Fakih W, Gong DS, Auger C, Pieper MP, Morel O et al. SGLT2 expression in the left ventricle of cardiac patients is correlated with low-grade inflammation involving the pro-oxidant AT1R/NADPH oxidases/SGLT2 crosstalk: potential role in heart failure. Eur Heart J. 2023;44(Supplement_2).
Pitt B, Bhatt DL, Metra M. Does SGLT1 inhibition add to the benefits of SGLT2 inhibition in the prevention and treatment of heart failure? Eur Heart J. 2022;43(45):4754–7.
Li J, Zhu C, Liang J, Hu J, Liu H, Wang Z, et al. Cardiovascular benefits and safety of sotagliflozin in type 2 diabetes mellitus patients with heart failure or cardiovascular risk factors: a bayesian network meta-analysis. Front Pharmacol. 2023;14:1303694.
Chen JY, Pan HC, Shiao CC, Chuang MH, See CY, Yeh TH, et al. Impact of SGLT2 inhibitors on patient outcomes: a network meta-analysis. Cardiovasc Diabetol. 2023;22(1):290.
Baartscheer A, Schumacher CA, Wust RC, Fiolet JW, Stienen GJ, Coronel R, Zuurbier CJ. Empagliflozin decreases myocardial cytoplasmic na(+) through inhibition of the cardiac na(+)/H(+) exchanger in rats and rabbits. Diabetologia. 2017;60(3):568–73.
Chen S, Coronel R, Hollmann MW, Weber NC, Zuurbier CJ. Direct cardiac effects of SGLT2 inhibitors. Cardiovasc Diabetol. 2022;21(1):45.
Uthman L, Baartscheer A, Schumacher CA, Fiolet JWT, Kuschma MC, Hollmann MW, et al. Direct cardiac actions of Sodium glucose cotransporter 2 inhibitors Target pathogenic mechanisms underlying heart failure in Diabetic patients. Front Physiol. 2018;9:1575.
Uthman L, Li X, Baartscheer A, Schumacher CA, Baumgart P, Hermanides J, et al. Empagliflozin reduces oxidative stress through inhibition of the novel inflammation/NHE/[Na(+)](c)/ROS-pathway in human endothelial cells. Biomed Pharmacother. 2022;146:112515.
Philippaert K, Kalyaanamoorthy S, Fatehi M, Long W, Soni S, Byrne NJ, et al. Cardiac late Sodium Channel current is a molecular target for the Sodium/Glucose Cotransporter 2 inhibitor Empagliflozin. Circulation. 2021;143(22):2188–204.
Mentzer RM Jr., Bartels C, Bolli R, Boyce S, Buckberg GD, Chaitman B, et al. Sodium-hydrogen exchange inhibition by cariporide to reduce the risk of ischemic cardiac events in patients undergoing coronary artery bypass grafting: results of the EXPEDITION study. Ann Thorac Surg. 2008;85(4):1261–70.
Pabel S, Wagner S, Bollenberg H, Bengel P, Kovacs A, Schach C, et al. Empagliflozin directly improves diastolic function in human heart failure. Eur J Heart Fail. 2018;20(12):1690–700.
Cappetta D, De Angelis A, Ciuffreda LP, Coppini R, Cozzolino A, Micciche A, et al. Amelioration of diastolic dysfunction by dapagliflozin in a non-diabetic model involves coronary endothelium. Pharmacol Res. 2020;157:104781.
Chung YJ, Park KC, Tokar S, Eykyn TR, Fuller W, Pavlovic D, et al. Off-target effects of sodium-glucose co-transporter 2 blockers: empagliflozin does not inhibit Na+/H + exchanger-1 or lower [Na+]i in the heart. Cardiovasc Res. 2021;117(14):2794–806.
Minutoli L, Puzzolo D, Rinaldi M, Irrera N, Marini H, Arcoraci V, et al. ROS-Mediated NLRP3 inflammasome activation in brain, heart, kidney, and Testis Ischemia/Reperfusion Injury. Oxid Med Cell Longev. 2016;2016:2183026.
Toldo S, Mezzaroma E, Buckley LF, Potere N, Di Nisio M, Biondi-Zoccai G, et al. Targeting the NLRP3 inflammasome in cardiovascular diseases. Pharmacol Ther. 2022;236:108053.
Aimo A, Castiglione V, Borrelli C, Saccaro LF, Franzini M, Masi S, et al. Oxidative stress and inflammation in the evolution of heart failure: from pathophysiology to therapeutic strategies. Eur J Prev Cardiol. 2020;27(5):494–510.
Glezeva N, Baugh JA. Role of inflammation in the pathogenesis of heart failure with preserved ejection fraction and its potential as a therapeutic target. Heart Fail Rev. 2014;19(5):681–94.
Elrakaybi A, Laubner K, Zhou Q, Hug MJ, Seufert J. Cardiovascular protection by SGLT2 inhibitors - do anti-inflammatory mechanisms play a role? Mol Metab. 2022;64:101549.
Wu J, He S, Song Z, Chen S, Lin X, Sun H, et al. Macrophage polarization states in atherosclerosis. Front Immunol. 2023;14:1185587.
Adamo L, Rocha-Resende C, Prabhu SD, Mann DL. Reappraising the role of inflammation in heart failure. Nat Rev Cardiol. 2020;17(5):269–85.
Scisciola L, Cataldo V, Taktaz F, Fontanella RA, Pesapane A, Ghosh P, et al. Anti-inflammatory role of SGLT2 inhibitors as part of their anti-atherosclerotic activity: data from basic science and clinical trials. Front Cardiovasc Med. 2022;9:1008922.
Theofilis P, Sagris M, Oikonomou E, Antonopoulos AS, Siasos G, Tsioufis K, Tousoulis D. The impact of SGLT2 inhibitors on inflammation: a systematic review and meta-analysis of studies in rodents. Int Immunopharmacol. 2022;111:109080.
Byrne NJ, Matsumura N, Maayah ZH, Ferdaoussi M, Takahara S, Darwesh AM, et al. Empagliflozin blunts worsening Cardiac Dysfunction Associated with reduced NLRP3 (nucleotide-Binding domain-like receptor protein 3) inflammasome activation in Heart failure. Circ Heart Fail. 2020;13(1):e006277.
Quagliariello V, De Laurentiis M, Rea D, Barbieri A, Monti MG, Carbone A, et al. The SGLT-2 inhibitor empagliflozin improves myocardial strain, reduces cardiac fibrosis and pro-inflammatory cytokines in non-diabetic mice treated with doxorubicin. Cardiovasc Diabetol. 2021;20(1):150.
Yurista SR, Sillje HHW, Oberdorf-Maass SU, Schouten EM, Pavez Giani MG, Hillebrands JL, et al. Sodium-glucose co-transporter 2 inhibition with empagliflozin improves cardiac function in non-diabetic rats with left ventricular dysfunction after myocardial infarction. Eur J Heart Fail. 2019;21(7):862–73.
Juni RP, Al-Shama R, Kuster DWD, van der Velden J, Hamer HM, Vervloet MG et al. Empagliflozin restores chronic kidney disease-induced impairment of endothelial regulation of cardiomyocyte relaxation and contraction. Kidney Int. 2021;99(5):1088 – 101. •This in vitro study demonstrated two important findings supporting the use of SGLT2 inhibitors in the dialysis population; (1) uremic serum induced impairment of endothelial regulation of cardiomyocyte relaxation and contraction and (2) empagliflozin restored those cardiomyocyte impairments.
Soares RN, Ramirez-Perez FI, Cabral-Amador FJ, Morales-Quinones M, Foote CA, Ghiarone T, et al. SGLT2 inhibition attenuates arterial dysfunction and decreases vascular F-actin content and expression of proteins associated with oxidative stress in aged mice. Geroscience. 2022;44(3):1657–75.
Mone P, Varzideh F, Jankauskas SS, Pansini A, Lombardi A, Frullone S, Santulli G. SGLT2 inhibition via Empagliflozin improves endothelial function and reduces mitochondrial oxidative stress: insights from Frail Hypertensive and Diabetic patients. Hypertension. 2022;79(8):1633–43.
D’Onofrio N, Sardu C, Trotta MC, Scisciola L, Turriziani F, Ferraraccio F, et al. Sodium-glucose co-transporter2 expression and inflammatory activity in diabetic atherosclerotic plaques: effects of sodium-glucose co-transporter2 inhibitor treatment. Mol Metab. 2021;54:101337.
Pahud de Mortanges A, Salvador D Jr., Laimer M, Muka T, Wilhelm M, Bano A. The role of SGLT2 inhibitors in atherosclerosis: a narrative Mini-review. Front Pharmacol. 2021;12:751214.
Choi AM, Ryter SW, Levine B. Autophagy in human health and disease. N Engl J Med. 2013;368(7):651–62.
Santovito D, Steffens S, Barachini S, Madonna R. Autophagy, innate immunity, and cardiac disease. Front Cell Dev Biol. 2023;11:1149409.
Biasizzo M, Kopitar-Jerala N. Interplay between NLRP3 inflammasome and autophagy. Front Immunol. 2020;11:591803.
Fukushima K, Kitamura S, Tsuji K, Wada J. Sodium-glucose cotransporter 2 inhibitors work as a Regulator of Autophagic Activity in Overnutrition diseases. Front Pharmacol. 2021;12:761842.
Nah J, Sung EA, Zhai P, Zablocki D, Sadoshima J. Tfeb-mediated transcriptional regulation of Autophagy induces autosis during Ischemia/Reperfusion in the heart. Cells. 2022;11(2).
Zhang X, Wei M, Fan J, Yan W, Zha X, Song H, et al. Ischemia-induced upregulation of autophagy preludes dysfunctional lysosomal storage and associated synaptic impairments in neurons. Autophagy. 2021;17(6):1519–42.
Zhu H, Tannous P, Johnstone JL, Kong Y, Shelton JM, Richardson JA, et al. Cardiac autophagy is a maladaptive response to hemodynamic stress. J Clin Invest. 2007;117(7):1782–93.
Packer M. SGLT2 inhibitors: role in protective reprogramming of cardiac nutrient transport and metabolism. Nat Rev Cardiol. 2023;20(7):443–62.
Aragon-Herrera A, Feijoo-Bandin S, Otero Santiago M, Barral L, Campos-Toimil M, Gil-Longo J, et al. Empagliflozin reduces the levels of CD36 and cardiotoxic lipids while improving autophagy in the hearts of Zucker diabetic fatty rats. Biochem Pharmacol. 2019;170:113677.
Li X, Flynn ER, do Carmo JM, Wang Z, da Silva AA, Mouton AJ, et al. Direct cardiac actions of sodium-glucose cotransporter 2 inhibition improve mitochondrial function and attenuate oxidative stress in pressure overload-Induced Heart failure. Front Cardiovasc Med. 2022;9:859253.
Ren C, Sun K, Zhang Y, Hu Y, Hu B, Zhao J, et al. Sodium-glucose CoTransporter-2 inhibitor Empagliflozin ameliorates Sunitinib-Induced Cardiac Dysfunction via Regulation of AMPK-mTOR Signaling pathway-mediated autophagy. Front Pharmacol. 2021;12:664181.
Jiang K, Xu Y, Wang D, Chen F, Tu Z, Qian J, et al. Cardioprotective mechanism of SGLT2 inhibitor against myocardial infarction is through reduction of autosis. Protein Cell. 2022;13(5):336–59.
Madonna R, Moscato S, Cufaro MC, Pieragostino D, Mattii L, Del Boccio P, et al. Empagliflozin inhibits excessive autophagy through the AMPK/GSK3beta signalling pathway in diabetic cardiomyopathy. Cardiovasc Res. 2023;119(5):1175–89.
Lemmer IL, Willemsen N, Hilal N, Bartelt A. A guide to understanding endoplasmic reticulum stress in metabolic disorders. Mol Metab. 2021;47:101169.
Chaudhari N, Talwar P, Parimisetty A, Lefebvre d’Hellencourt C, Ravanan P. A molecular web: endoplasmic reticulum stress, inflammation, and oxidative stress. Front Cell Neurosci. 2014;8:213.
Bhattarai KR, Riaz TA, Kim HR, Chae HJ. The aftermath of the interplay between the endoplasmic reticulum stress response and redox signaling. Exp Mol Med. 2021;53(2):151–67.
Chipurupalli S, Samavedam U, Robinson N. Crosstalk between ER stress, autophagy and inflammation. Front Med (Lausanne). 2021;8:758311.
Shih JY, Lin YW, Fisch S, Cheng JT, Kang NW, Hong CS, et al. Dapagliflozin suppresses ER stress and improves subclinical myocardial function in diabetes: from Bedside to Bench. Diabetes. 2021;70(1):262–7.
Wang CC, Li Y, Qian XQ, Zhao H, Wang D, Zuo GX, Wang K. Empagliflozin alleviates myocardial I/R injury and cardiomyocyte apoptosis via inhibiting ER stress-induced autophagy and the PERK/ATF4/Beclin1 pathway. J Drug Target. 2022;30(8):858–72.
Ren FF, Xie ZY, Jiang YN, Guan X, Chen QY, Lai TF, Li L. Dapagliflozin attenuates pressure overload-induced myocardial remodeling in mice via activating SIRT1 and inhibiting endoplasmic reticulum stress. Acta Pharmacol Sin. 2022;43(7):1721–32.
Chang WT, Lin YW, Ho CH, Chen ZC, Liu PY, Shih JY. Dapagliflozin suppresses ER stress and protects doxorubicin-induced cardiotoxicity in breast cancer patients. Arch Toxicol. 2021;95(2):659–71.
Malik A, Bagchi AK, Jassal DS, Singal PK. Doxorubicin–induced cardiomyopathy is mitigated by empagliflozin via the modulation of endoplasmic reticulum stress pathways. Mol Med Rep. 2024;29(5).
Macha S, Mattheus M, Halabi A, Pinnetti S, Woerle HJ, Broedl UC. Pharmacokinetics, pharmacodynamics and safety of empagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, in subjects with renal impairment. Diabetes Obes Metab. 2014;16(3):215–22.
Barreto J, Borges C, Rodrigues TB, Jesus DC, Campos-Staffico AM, Nadruz W, et al. Pharmacokinetic properties of Dapagliflozin in Hemodialysis and Peritoneal Dialysis patients. Clin J Am Soc Nephrol. 2023;18(8):1051–8.
Barnett AH, Mithal A, Manassie J, Jones R, Rattunde H, Woerle HJ, et al. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2014;2(5):369–84.
Author information
Authors and Affiliations
Contributions
R.S. and Y.O. wrote the main manuscript text and prepared Fig. 1. Y.O. prepared Fig. 2. NRD and TS reviewed the manuscript and provided critical feedback. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
RS and NRD declare that they have no conflict of interest. TS has received grants from NIDDK, NHLBI, NINR, and Numares Health and participated on a data safety monitoring board or advisory board for CHINOOK trial and Wake Forest university. YO has received consultant fees from CLS Vifor pharma.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Siddiqui, R., Obi, Y., Dossabhoy, N.R. et al. Is There a Role for SGLT2 Inhibitors in Patients with End-Stage Kidney Disease?. Curr Hypertens Rep (2024). https://doi.org/10.1007/s11906-024-01314-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s11906-024-01314-3