Abstract
Purpose of Review
HIV/AIDS and COVID-19 have been the major pandemics overwhelming our times. Given the enduring immune disfunction featuring people living with HIV (PLWH) despite combination antiretroviral therapy (cART), concerns for higher incidence and severity of SARS-CoV-2 infection as well as for suboptimal responses to the newly developed vaccines in this population arose early during the pandemics. Herein, we discuss the complex interplay between HIV and SARS-CoV-2, with a special focus on the immune responses to SARS-CoV-2 natural infection and vaccination in PLWH.
Recent Findings
Overall, current literature shows that COVID-19 severity and outcomes may be worse and immune responses to infection or vaccination lower in PLWH with poor CD4 + T-cell counts and/or uncontrolled HIV viremia. Data regarding the risk of post-acute sequelae of SARS-CoV-2 infection (PASC) among PLWH are extremely scarce, yet they seem to suggest a higher incidence of such condition.
Summary
Scarce immunovirological control appears to be the major driver of weak immune responses to SARS-CoV-2 infection/vaccination and worse COVID-19 outcomes in PLWH. Therefore, such individuals should be prioritized for vaccination and should receive additional vaccine doses. Furthermore, given the potentially higher risk of developing long-term sequelae, PLWH who experienced COVID-19 should be ensured a more careful and prolonged follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: HIV/AIDS and COVID-19, a Tale of Two Intersecting Pandemics
HIV/AIDS and COVID-19 have been the major pandemics overwhelming the contemporary era. HIV/AIDS was firstly reported in 1981 in previously healthy young men who developed a life-threatening Pneumocystis carinii (now known as Pneumocystis jirovecii) pneumonia, whose underlying cause was revealed 2 years later to be a retrovirus, which was named human immunodeficiency virus (HIV). Its incidence has been declining since 1996, when protease inhibitors were rolled out for HIV treatment, so that the pandemic may be now considered to have reached an endemic state worldwide [1]. COVID-19 emerged in late 2019 as a severe respiratory disease caused by the quickly identified severe acute respiratory coronavirus 2 (SARS-CoV-2), intersecting the HIV/AIDS pandemics in various ways.
Physicians and medical infrastructures previously dedicated to the care of people living with HIV (PLWH) were reallocated on the frontline in tackling COVID-19 [2]. In-person clinical visits were discouraged in favor of telemedicine, which is most likely destined to become the standard of care for PLWH with well-controlled infection in the future [3]. Limitations also involved HIV infection laboratory monitoring, as laboratory facilities and personnel were employed in diagnostic testing for SARS-CoV-2. Shortage of medical resources, fear of exposure to SARS-CoV-2, and lockdown restrictions hindered the access to antiretroviral therapy [4]. Overall, notwithstanding different approaches to cope with COVID-19 in PLWH have been put forward in different settings, all the aforementioned elements resulted in a suboptimal care of HIV infection and other comorbidities in PLWH and exacerbated inequalities for key populations affected by HIV [5].
In the meanwhile, given the HIV-driven immune dysfunction also in the course of effective combination antiretroviral therapy (cART), concerns for higher susceptibility of PLWH to SARS-CoV-2 infection and poor COVID-19 outcomes arose, thus leading to prioritize this population for vaccine administration when they became available, albeit the readiness of their immune system to respond to these novel vaccines was unknown at the time. After nearly 3 years into the COVID-19 pandemics, numerous studies aiming to unveil whether PLWH are actually at higher clinical risk have been published, but yielded apparently contradictory findings. Additionally, data assessing how efficiently the immune system of PLWH faces SARS-CoV-2 infection and responds to COVID-19 vaccines remain limited.
In this review, we summarize the knowns and the unknowns of the complex interplay between HIV and SARS-CoV-2 infection, with a special focus on the immune responses to SARS-CoV-2 natural infection and vaccination in PLWH.
Incidence and Clinical Outcome of SARS-CoV-2 Infection in PLWH
An early literature review reported that the prevalence of SARS-CoV-2 infection in PLWH was similar to that observed in the general population [6]. The same study also reported that PLWH accounted for approximately 1.0% of total hospitalized COVID-19 cases [6]. A recent cross-sectional study on 4400 consecutive PLWH attending an HIV Clinic in Spain between November 2020 and May 2021 demonstrated that the prevalence of SARS-CoV-2 infection, determined through antibody presence, was 28% [7]. In contrast, recent findings from the EuroSIDA cohort reported positive SARS-CoV-2 PCR results in 122/1026 participants (1.8%) [8]. The different testing procedures and reasons for testing may explain, at least in part, the opposing results.
From a pathogenic standpoint, single-cell transcriptomic analysis across different tissues reported higher co-expression of ACE2 and TMPRSS2 in the lung of HIV-infected humans and in the gut of SHIV-infected non-human primates as compared with uninfected controls [9], suggesting a possible higher risk of SARS-CoV-2 acquisition in PLWH. However, current literature [6, 10,11,12,13] indicates that HIV infection per se is not a risk factor for SARS-CoV-2 infection.
Conflicting data have also emerged in terms of clinical outcome of COVID-19 in the setting of HIV infection. One of the first studies published during the first pandemic wave demonstrated that PLWH were at increased risk of mortality among subjects hospitalized for COVID-19 in the UK [14]. An even higher risk of mortality in PLWH was reported when analyzing data from a large primary care database in the same country [15]. A study from Chile, which was also conducted in the first wave, showed that PLWH were more likely to be admitted to the ICU [16]. In keeping with these results, current findings from the WHO Global Clinical COVID-19 platform, which however mirror data contribution from Africa, showed that HIV infection was an independent risk factor for severe COVID-19 and in-hospital mortality [17]. In this respect, some studies [18], but not others [16], reported poor viro-immunological control as a reason underlying disease severity/mortality in PLWH.
In contrast to the above, research has also demonstrated a similar outcome in PLWH and the general population [19,20,21], highlighting the role of comorbidities in the development of critical COVID-19 [22]. In particular, one study demonstrated a lower rate of ICU admissions, invasive mechanical ventilation, or death in a large cohort of PLWH who were younger than uninfected controls [23]. A recent meta-analysis reported no difference in the risk of death in PLWH compared with the HIV-seronegative population [24].
Taken together, literature published thus far has shown heterogeneity in COVID-19 severity in the context of HIV infection. Age and comorbidities, as well as the lack of viro-immunological control, represent possible risk factors for a worse clinical outcome, and their respective contribution should be assessed in future studies [25•].
Interestingly, some observational studies reported a protective effect of certain antiretroviral drugs, namely tenofovir disoproxil fumarate/emtricitabine (TDF/FTC), against SARS-CoV-2 infection and COVID-19–related outcomes in both PLWH [13, 26, 27] and HIV pre-exposure prophylaxis (PrEP) users [28, 29]. This potential protective effect is biologically plausible due to the ability of nucleotide analog reverse transcriptase inhibitors (NRTIs) to inhibit the SARS-CoV-2 RNA-dependent RNA polymerase [30, 31]. However, others did not find such an association [7, 32]. These contradictory findings may be the consequence of the baseline characteristics of TDF/FTC-users, which are intrinsically associated with a more favorable outcome of SARS-CoV-2 infection.
Data regarding post-acute sequelae of SARS-CoV-2 infection (PASC) in PLWH are limited. The major risk factors for PASC have been described to be severity of disease, being unvaccinated against SARS-CoV-2, and medical comorbidities [33]. Furthermore, PASC has been associated with a residual inflammation following SARS-CoV-2 infection [34]. Therefore, given the potential for greater risk of COVID-19 severity and reduced responses to SARS-CoV-2 vaccines, and considered the higher burden of comorbidities [35] and the greater baseline levels of immune activation and systemic inflammation [36, 37], PLWH may be at higher risk of developing PASC. Actually, the few published studies showed a significantly greater risk of PASC in PLWH when adjusting for other factors, indicating that HIV infection may be an independent risk factor for such condition [38, 39•].
Immune Responses to SARS-CoV-2 Infection in PLWH
Innate Immune Responses
Type-I interferons (IFNs-I) constitute the first innate immune barrier to SARS-CoV-2 infection at mucosal sites [40]. However, SARS-CoV-2 has evolved several mechanisms to evade such host defense via both its structural and non-structural proteins [41, 42]. Moreover, inborn mutations in genes involved in the regulation of IFNs-I immunity, as well as production of auto-antibodies against IFNs-I during COVID-19, have been associated with poor clinical outcome [43, 44].
HIV infection triggers interferon responses in the earliest phases, contributing to limit viral replication; nonetheless, persistent exposure to IFNs-I in the chronic phase of HIV infection is associated with desensitization and immune hyperactivation, thus paradoxically contributing to disease progression [45, 46].
These observations suggest that complex interactions between the two viruses might influence IFNs-I responses in HIV/SARS-CoV-2 coinfection. An interesting study evaluated the impact of HIV infection on gut epithelial cells susceptible to SARS-CoV-2 infection, showing that chronic-treated HIV infection drives a strong interferon signaling response within absorptive enterocytes, which, however, does not prevent SARS-CoV-2 infection in this compartment [47•] (Fig. 1A). These findings may indicate that the persistent IFNs-I signaling which features chronic HIV infection despite effective cART is not able to confer a protection against SARS-CoV-2 infection. However, the interplay between HIV and SARS-CoV-2 in modulating IFNs-I responses in other anatomical sites, especially the upper respiratory tract which is the site of initial infection, and its role in influencing the susceptibility to SARS-CoV-2 infection in PLWH, have not been characterized and require future research efforts.
Immune responses to SARS-CoV-2 infection in PLWH. A Chronic HIV infection on cART drives a strong constitutive IFN-I signaling within absorptive enterocytes in the small intestine, which, however, is not able to prevent SARS-CoV-2 infection in this compartment. The interplay between HIV and SARS-CoV-2 in modulating IFNs-I responses in other anatomical sites, especially the respiratory tract, which is the site of initial infection, is currently unknown. B PLWH with well-controlled HIV infection mount adaptive immune responses comparable to those of people without HIV. Yet, PLWH with low CD4 + T-cell counts and/or detectable HIV viremia develop suboptimal immune responses to SARS-CoV-2 infection (fewer and exhausted SARS-CoV-2–specific T-cells, impaired T-cell cross recognition of VOCs, lower SARS-CoV-2–specific B-cells and neutralizing antibodies). C HIV infection is associated with enduring systemic inflammation and immune activation despite effective cART; on the other side, in absence of cART, HIV infection leads to immune suppression, mainly—albeit not only—driven by the depletion of CD4 + T-cells. Whether such features of HIV infection may exacerbate or hinder the COVID-19–related cytokine storm is currently unknown, as the few available data are conflicting. D PLWH with low CD4 + T-cell counts may have a delayed SARS-CoV-2 clearance due to the immune defects. The subsequent prolonged viral replication (sustained by the RNA-dependent RNA-polymerase) can lead to the emergence of multiple mutations and thus to the development of new viral variants escaping from antibody neutralization. PLWH, people living with HIV; cART, combination antiretroviral therapy; IFN-I, type-I interferon; VOCs, variants of concern. Created with BioRender.com
Adaptive Immune Responses
Early and robust development of SARS-CoV-2–specific cell-mediated immunity and neutralizing antibodies has been associated to a favorable clinical course of COVID-19 [48,49,50]. HIV infection is characterized by a profound disruption of the adaptive immune system, in both its cellular and humoral components, with destruction of CD4 + T-cells, increased CD8 + T-cells, T-cell activation/exhaustion, defective T follicular helper (Tfh) cells activity, and dysfunction and polyclonal activation of B-cells [51, 52]. Furthermore, it has recently been demonstrated that SARS-CoV-2 is able to productively infect CD4 + T-cells binding to cell entry receptors other than ACE2 (like LFA-1 and CD147) and to induce their apoptosis which is probably dependent on mitochondria ROS-hypoxia pathways [53••, 54••], suggesting that HIV and SARS-CoV-2 may collide on the immune system. These observations raise the concern that PLWH, especially those with incomplete immune restoration despite virologically effective cART [55], may not appropriately respond to SARS-CoV-2 infection. Thus far, data on adaptive immune responses to natural SARS-CoV-2 infection in this population is limited and, at times, conflicting.
One of the earliest studies in this regard evaluated the T-cell profile in the course of HIV/SARS-CoV-2 coinfection during the first wave of the COVID-19 pandemics, when some PLWH suspended cART due to medication shortages. Compared to SARS-CoV-2 mono-infected individuals, HIV/SARS-CoV-2–co-infected individuals showed reduced Th1 cells and cytotoxic CD8 + T-cell responses, as well as a higher rate of T-cell exhaustion, which was even more pronounced in those not taking cART [56]. These data suggest a synergic effect of HIV and SARS-CoV-2 on T-cell dysfunction, especially in PLWH with uncontrolled HIV viremia, which may not mount proper immune responses against SARS-CoV-2. A more recent study showed that individuals with unsuppressed HIV infection mount weak antigen-specific CD4 + and CD8 + T-cell responses to SARS-CoV-2 and poorly recognize SARS-CoV-2 beta variant, due to HIV-induced immune defects such as low CD4 + T-cell counts, high HIV plasma viral loads, and elevated immune activation. Yet, virologically suppressed PLWH exhibit SARS-CoV-2–specific T-cell responses similar to those of HIV-negative peers, highlighting the role of uncontrolled HIV infection in hampering immune responses to SARS-CoV-2 and T-cell cross-recognition between viral variants, thus partly explaining the high propensity for severe COVID-19 among PLWH and their vulnerability to emerging SARS-CoV-2 VOCs [57••].
Also, inadequate immune reconstitution on virologically effective cART has been shown to potentially hinder the development of T-cell responses to SARS-CoV-2 infection. Indeed, while T-cell responses against structural and non-structural SARS-CoV-2 proteins in the convalescent phase of mild COVID-19 are similar in PLWH with cART-suppressed HIV viral load and HIV-negative subjects overall, the magnitude of SARS-CoV-2–specific T-cell responses is positively related with the CD4/CD8 ratio and the size of naïve CD4 T-cell pool in PLWH [58••]. Accordingly, another study found that HIV infection does not significantly alter the functional and phenotypical profile of SARS-CoV-2–specific CD4 + T-cells, yet the magnitude of SARS-CoV-2–specific T-cell and humoral responses is lower in PLWH with poor CD4 T-cell recovery despite cART [59].
Donadeu et al. reported that COVID-19–recovered PLWH with well-controlled HIV infection are capable of developing a robust adaptive SARS-CoV-2–specific immune response which persists up to 6 months, similar to people without HIV; furthermore, immune responses are more pronounced among severe COVID-19 patients, irrespective of HIV status [60••]. These data suggest that magnitude and persistence of the immune response after SARS-CoV-2 infection may be mainly driven by the degree of COVID-19 clinical severity, rather than the HIV status.
Some studies showed that T-cell and humoral responses to SARS-CoV-2 infection do not necessarily move in the same direction. Peluso et al. found that, in the backdrop of similar humoral responses compared to HIV-uninfected individuals, cART-treated PLWH recovering from SARS-CoV-2 infection display high expression of the co-inhibitory receptor PD-1 on SARS-CoV-2–specific memory CD4 + T-cells and low frequencies of specific CD8 + T-cells, suggesting that they may have impaired T-cell functionality upon reencountering infection [39•]. It has also been reported that although PLWH on effective cART may present lower memory T-cell responses against SARS-CoV-2 as well as dysregulated T follicular helper (Tfh) populations, that is enough to generate a cooperation between T-cells and B-cells that allows to elicit an effective antibody response against the pathogen [61].
Studies evaluating humoral immune responses to SARS-CoV-2 in PLWH also yielded inconsistent observations, probably due to the different demographic and viro-immunological characteristics of study participants, various degree of COVID-19 severity, and sampling during diverse phases post-infection.
Alrubayyi et al. found comparable antibody titers against S1 and N proteins of SARS-CoV-2 in HIV-positive and -negative subjects after mild COVID-19 [58••]. Similarly, Alcaide et al. showed that antibody responses during the 6-month period post-mild COVID-19 do not differ by HIV status [62]. Snyman et al. reported that magnitude, kinetics, and durability of anti-SARS-CoV-2 IgM, IgG, and IgA, as well as neutralization potency, are similar in PLWH and people without HIV [63]. It should be specified that all the studies mentioned above included individuals with well-controlled HIV infection.
In sharp contrast, Spinelli et al. found lower RBD-specific IgG concentrations and pseudovirus neutralizing antibodies titers in PLWH with past SARS-CoV-2 infection as compared to HIV-negative individuals [64]. Liu et al. described that in the acute phase of COVID-19, PLWH exhibit a lower IgG seroconversion rate and shorter duration of humoral responses compared to HIV-negative individuals [65]. It must be noted, however, that both studies included also virally unsuppressed people. Accordingly, Khan et al. showed lower neutralization of the Delta variant and a higher frequency of non-responders in PLWH, with the highest frequency of non-responders in those with uncontrolled HIV viremia; furthermore, neutralization activity was correlated with CD4 + T-cell counts, underscoring the importance of both immune recovery and HIV viremia suppression on cART, in influencing humoral immune responses to SARS-CoV-2 [66].
Humoral responses in the convalescent phase of SARS-CoV-2 infection in PLWH may also be influenced by the severity of COVID-19, since antibodies’ magnitude and functionality in PLWH have been reported similar to those of people without HIV in the mild (asymptomatic) and severe (symptomatic requiring hospitalization) disease, but diminished in the moderate (symptomatic not requiring hospitalization) disease [67].
Lastly, given that PLWH have been shown to be at higher risk of developing PASC, Peluso et al. explored immunologic features potentially related to such condition in this population, yet no relationships between PASC and SARS-CoV-2–specific humoral and T-cell responses or immune exhaustion were found [39•], suggesting that other factors may be involved in PASC pathogenesis in PLWH.
Taken together, these data indicate that adaptive immune responses to SARS-CoV-2 infection in PLWH are similar to those of the general population overall, but may be less efficient in the setting of scarce immune recovery and uncontrolled HIV viremia (Fig. 1B).
Inflammation
HIV infection elicits a chronic hyperinflammatory state that persists despite effective cART [36, 37], sharing inflammatory markers that have been also described as elevated in severe COVID-19, such as IL-6 and TNF-α [49]. Given these premises, it can be speculated that HIV may exacerbate COVID-19–related cytokine storm and thus severity, leading to unfavorable outcomes. On the other hand, it may be assumed that PLWH can be protected from hyper-activation/inflammation–mediated immunopathology due to the HIV-driven immune defects. As described in HIV-negative individuals [50], PLWH hospitalized for COVID-19 have been shown capable of mounting a profound inflammatory reaction in response to SARS-CoV-2 coinfection that is higher in fatal cases [68]. While some studies reported lower levels of inflammatory markers such as IL-6, TNF-α, and IL-8 in PLWH as compared to the HIV-negative counterpart [61, 69], another study found higher IL-6, TNF-α, and IP-10 in HIV/SARS-CoV-2–coinfected individuals [39•]. Hence, whether immune imbalances which feature chronic HIV infection may enhance or hinder the COVID-19–related cytokine storm is yet to be determined (Fig. 1C).
Delayed Clearance of SARS-CoV-2 and Immune Escape
Low CD4 + T-cell counts in PLWH can potentially hamper SARS-CoV-2 clearance, as suggested by a murine model of acute SARS-CoV-2 infection, in which depletion of CD4 + T-cells led to reduced antibody response and delayed viral clearance [70]. Prolonged infections may allow SARS-CoV-2 to evolve diverse resistance mutations, since it mutates at a relatively slow rate compared to other RNA viruses due to its proof-reading mechanism [71]. Actually—as previously described in patients with immune suppression due to other causes [72,73,74]—several cases of prolonged SARS-CoV-2 infection have been reported in PLWH with severe T-cell depletion and/or AIDS, with subsequent emergence of a multitude of mutations conferring extensive escape from antibody neutralization elicited by both ancestral SARS-CoV-2 infection and vaccines [18, 75••, 76, 77] (Fig. 1D).
SARS-CoV-2 Vaccine Efficacy and Safety in PLWH
When SARS-CoV-2 vaccines were rolled out, PLWH—especially those with current CD4 + T-cell count < 200/μL, evidence of an opportunistic infection, and/or with a detectable viral load—were prioritized for vaccination, due to the potential higher risk for worse COVID-19 outcomes [78].
Given that suboptimal and less durable immune responses to several vaccines have been reported in PLWH, particularly in those with scarce immune recovery despite cART [79,80,81,82], concerns were raised about immunogenicity and clinical efficacy of these vaccines in this potentially more vulnerable population.
Unfortunately, the larger phase 2/3 SARS-CoV-2 vaccine clinical trials included few PLWH (176 for mRNA-1273, 196 for BNT162b2, and 107 for ChAdOx1-S), therefore lacking to report efficacy, safety, and immunogenicity for this sub-population [83,84,85]. Additionally, there are no head-to-head comparisons between different COVID-19 vaccines in PLWH thus far; hence, whether a certain vaccine platform is more effective and should therefore be preferred in this population is currently unknown. Furthermore, data on vaccine-induced protection against emerging variants of concern (VOCs) in this population are also lacking and should be addressed by future research.
Nonetheless, two large longitudinal studies carried out in the USA found a higher rate of breakthrough infections in fully vaccinated PLWH [86, 87]; however, among them, high CD4 + T-cell counts (> 500/μL) and having received an additional dose were associated with a reduced risk [86]. These data clearly suggest that the clinical efficacy of the primary vaccine cycle may be inferior in PLWH, especially in those with low CD4 + T-cell counts, who should therefore receive additional doses.
Risk of severe side effects to SARS-CoV-2 vaccines has not been reported to be higher in PLWH than in general population. However, HIV viral blips after SARS-CoV-2 vaccination were described in some PLWH with low CD4 + T-cell nadir and/or high HIV-RNA zenith [88, 89]. Previous studies have found transient increases in HIV viral load with other vaccines, including HBV, influenza, and Streptococcus pneumoniae [90,91,92], which typically occurs within 7–14 days post-vaccination [93]. Such phenomenon may be attributed to a reactivation of the latent HIV reservoir, probably due to a vaccine-elicited generalized inflammatory response with cytokine production able to activate bystander cells harboring latent HIV, rather than the solely activation of HIV-infected vaccine-specific T-cells [93]. In this context, the increased HIV transcription is accompanied by enhanced HIV-specific CD8 + T-cell responses, pointing to standard vaccines as a potential tool to reverse HIV latency to enable eradication by cytotoxic T-cells [93]. Accordingly, a recent study showed that BNT162b2 vaccine activates the RIG-I/TLR–TNF–NFkB axis, resulting in transcription of HIV proviruses; in parallel, Nef-specific CD8 + T-cells increase and acquire cytotoxic effector functions, which correlate with reduction of cell-associated HIV-mRNA, suggesting killing or suppression of cells transcribing HIV; however, significant depletion of intact proviruses was not observed, highlighting challenges to achieving HIV reservoir reductions [94•]. Nevertheless, the interplay between vaccines, immune system, and latent HIV infection is yet to be thoroughly understood and deserves further research in order to inform future HIV eradication strategies.
Immune Responses to SARS-CoV-2 Vaccines in PLWH
Whilst published data on clinical efficacy in PLWH are scarce, immunogenicity to SARS-CoV-2 vaccines have been studied more extensively albeit not comprehensively. In particular, cellular responses to these vaccines have been evaluated only by few studies thus far, likely due to technical difficulties; however, given the T-cell dysfunction which features HIV infection, it would be of paramount importance to assess the ability of COVID-19 vaccines to induce polyfunctional SARS-CoV-2–specific T-cells, which have been shown to lend protection against the severe forms of disease [48, 49].
In general, immune responses to mRNA vaccines (mRNA-1273 and BNT162b2) have been reported similar to those of the general population in people with well-controlled HIV infection [95•, 96••]. Additionally, no differences in BNT162b2-elicited antibody neutralization of different VOCs (alpha, beta, and gamma) have been shown between PLWH and HIV-negative vaccinees [97].
On the contrary, PLWH with low CD4 + T-cell counts, detectable viremia, and/or previous AIDS were found to have weaker and less durable humoral and T-cell responses to mRNA vaccines [95•, 96••, 98•, 99, 100, 101•], suggesting that they may benefit from additional vaccine doses. In this respect, a third dose of a mRNA vaccine following the primary cycle has been shown to strongly boost humoral albeit not T-cell responses in PLWH with advanced disease at the time of HIV diagnosis (CD4 + T-cells < 200/μL and/or AIDS), irrespective of the current CD4 + T-cell count [102••]. Furthermore, PLWH with a current CD4 + T-cell count < 250/μL retain a similar neutralization activity against Delta variant, yet reduced against Beta [103].
In accordance with these findings, we have recently shown that in PLWH with pre-cART advanced immunodeficiency and full virologic control on cART, a 2-dose mRNA-1273 vaccine cycle is able to induce spike-specific memory polyfunctional T helper 1 (Th1) and T follicular helper (Tfh) cells as well as anti-RBD antibodies capable of inhibiting the spike-ACE2 binding. Such vaccine-elicited immune responses, which are still detectable after 6 months from vaccination, are not inferior to those of HIV-negative peers, albeit a positive correlation between humoral responses and CD4 + T-cell recovery on cART were found [104].
As regard adenoviral vector vaccines (ChAdOx1-S and Ad26.COV2.S), no significant differences were found in magnitude and durability of vaccine-induced humoral and T-cell responses based on HIV status [66, 105••, 106]. PLWH also show ChAdO1x-S–elicited cross-reactive binding antibodies to the Beta variant; furthermore, those who develop high-titre responses also retain neutralization activity against Beta [107]. PLWH with well-controlled HIV vaccinated with Ad26.COV2.S display similar neutralization response of the Delta variant as compared to people without HIV [66]. However, immunogenicity of such vaccines in PLWH with lower CD4 + T-cell counts has not been evaluated.
Alternative vaccine platforms—protein (NVX-CoV2373) and inactivated vaccines (CoronaVac, BBIBP-CorV)—have been administered in PLWH in some countries. Humoral responses to NVX-CoV2373 have been shown lower in PLWH as compared to people without HIV, especially in those without prior SARS-CoV-2 infection [108•]. Immunogenicity of inactivated vaccines in PLWH have been reported similar [109, 110•] or lower [111,112,113] than in general population according to different studies, but invariably reduced in those with low CD4 + T-cell counts and/or CD4/CD8 ratio [109, 110•, 111].
A comparison between the immunogenicity of different vaccine platforms in PLWH has been reported in some studies. mRNA vaccines appear to elicit the highest immune responses in this population [113,114,115, 116•, 117]. Among mRNA vaccines, BNT162b2 has been show less immunogenic than mRNA-1273 [100, 102••, 118]. However, given the lack of immune thresholds that correlate to protection after vaccination, the clinical significance of such lower immunogenicity is currently unknown. Nonetheless, in light of these data and awaiting future clarifications on their clinical relevance, mRNA vaccines should be preferred in PLWH [119].
Some studies reported higher immune responses to both mRNA and adenoviral vector COVID-19 vaccines in PLWH with previous SARS-CoV-2 infection [107, 118, 120] or preexisting cross-reactive T-cell responses correlated with prior exposure to seasonal coronaviruses [106], suggesting that, similar to what observed in the general population, a preexisting immune memory may boost immune responses to COVID-19 vaccines.
Lastly, similarly to HIV-negative individuals [121, 122], PLWH show waning antibody immunity (especially against VOCs), yet persistent T-cell responses 6 months post-vaccination [123•], pointing to a potential role of vaccine-elicited cellular immune memory in ensuring a long-term protection.
The main findings of the major studies evaluating immune responses to different SARS-CoV-2 vaccine platforms in PLWH are summarized in Table 1.
Concluding Remarks
COVID-19 pandemics posed a serious threat to public health and collided with HIV/AIDS, leading to a suboptimal care of PLWH worldwide. Nevertheless, concerns for higher susceptibility of PLWH to SARS-CoV-2 infection and poor COVID-19 outcomes arose, thus leading to prioritize this population for vaccination. Additionally, given the enduring immune dysfunction which features chronic HIV infection despite effective cART, PLWH have been considered at risk of lower and less functional immune responses to SARS-CoV-2 natural infection and vaccination, with potentially negative implications for disease outcomes and vaccines efficacy.
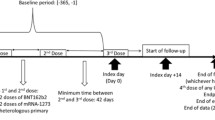
Despite such concerns, current knowledge, albeit not granular and at times apparently conflicting, is somehow reassuring for PLWH with well-controlled HIV infection. Immune responses to both SARS-CoV-2 natural infection and vaccination in PLWH have been shown similar to those of people without HIV, with the only exception of those with low CD4 + T-cell counts and/or uncontrolled HIV viremia, who may indeed develop suboptimal T-cell and humoral immune memory following infection and vaccination (Fig. 2). Accordingly, COVID-19 severity and outcomes in this population seem to be worse especially in the presence of concurrent age-related comorbidities and in case of severe CD4 + T-cells depletion, a condition which also potentially increase the risk of breakthrough infections after the primary vaccine cycle, suggesting a suboptimal immune response to vaccination. Data regarding the risk of PASC among PLWH are extremely scarce, yet seemingly indicative of a higher incidence, albeit whether immune factors are involved in its pathogenesis and whether it can negatively impact the immunologic landscape of chronic HIV infection in the long run is yet to be determined.
Interplay between HIV infection and immune responses to SARS-CoV-2 infection and vaccination. PLWH with well-controlled HIV infection on cART (suppressed HIV viremia and full recovery of CD4 + T-cell counts) mount adequate adaptive immune responses to both SARS-CoV-2 infection and vaccination, which lend protection against the severe forms of the disease and from future infections/reinfections. On the contrary, ongoing HIV replication and immunodeficiency with low CD4 + T-cell counts hamper the development of both T-cell and humoral memory in response to SARS-CoV-2 infection and vaccination, thus explaining the increased risk of severe COVID-19 and breakthrough infections in PLWH with scarce immunovirological control. Created with BioRender.com
Altogether, these data clearly support the need for additional vaccine doses in PLWH with ongoing HIV replication and/or scarce immune reconstitution despite virally effective cART. Furthermore, given the potentially higher risk of developing long-term sequelae, PLWH who experienced COVID-19 should be ensured a more careful and prolonged follow-up, in order to avoid adding the PASC fuel to the HIV crackling flames.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
UNAIDS. Fact sheet 2022. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf. Accessed 1 Oct 2022
Kowalska JD, Skrzat-Klapaczyńska A, Bursa D, Balayan T, Begovac J, Chkhartishvili N, et al. HIV care in times of the COVID-19 crisis - where are we now in Central and Eastern Europe? Int J Infect Dis. 2020;96:311–4. https://doi.org/10.1016/j.ijid.2020.05.013.
Budak JZ, Scott JD, Dhanireddy S, Wood BR. The impact of COVID-19 on HIV care provided via telemedicine-past, present, and future. Curr HIV/AIDS Rep. 2021;18(2):98–104. https://doi.org/10.1007/s11904-021-00543-4.
Luis H, Fridayantara WD, Mahariski P, Wignall FS, Irwanto I, Gedela K. Evolving ART crisis for people living with HIV in Indonesia. Lancet HIV. 2020;7(6):e384–5. https://doi.org/10.1016/S2352-3018(20)30138-7.
GLAAD. Invisible people. A retrospective report on the impacts of COVID & HIV in the United States. https://www.glaad.org/sites/default/files/Invisible%20People%20Report%20-%20COVID%20%26%20HIV%20-%20United%20States%20-%20GLAAD%20-2022-1.pdf. Accessed 1 Oct 2022
Ambrosioni J, Blanco JL, Reyes-Urueña JM, Davies MA, Sued O, Marcos MA, et al. Overview of SARS-CoV-2 infection in adults living with HIV. Lancet HIV. 2021;8(5):e294–305. https://doi.org/10.1016/S2352-3018(21)00070-9.
de Lazzari E, Blanco J, Rico N, Filella X, Egri N, Ruiz R, et al. Prevalence, risk factors and the impact of antiretroviral treatment in SARS-CoV-2 infection in people with HIV: a cross-sectional study. HIV Glasgow, 23–26 October 2022, Glasgow, UK / Virtual. J Int AIDS Soc. 25:e26009.https://doi.org/10.1002/jia2.26009
Fursa O, Bannister W, Neesgaard B, Podlekareva D, Kowalska J, Benfield T, et al. Prevalence, outcomes, and factors associated with testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection among people living with. HIV across Europe in the multinational EuroSIDA cohort HIV Glasgow, Glasgow, UK / Virtual. J Int AIDS Soc. 2022;25:e26009. https://doi.org/10.1002/jia2.26009.
Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM, Miao VN, Tzouanas CN, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016-35.e19. https://doi.org/10.1016/j.cell.2020.04.035.
Huang J, Xie N, Hu X, Yan H, Ding J, Liu P, et al. Epidemiological, virological and serological features of coronavirus disease 2019 (COVID-19) cases in people living with human immunodeficiency virus in Wuhan: a population-based cohort study. Clin Infect Dis. 2021;73(7):e2086–94. https://doi.org/10.1093/cid/ciaa1186.
Tesoriero JM, Swain CE, Pierce JL, Zamboni L, Wu M, Holtgrave DR, et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw Open. 2021;4(2):e2037069. https://doi.org/10.1001/jamanetworkopen.2020.37069.
Inciarte A, Gonzalez-Cordon A, Rojas J, Torres B, de Lazzari E, de la Mora L, et al. Clinical characteristics, risk factors, and incidence of symptomatic coronavirus disease 2019 in a large cohort of adults living with HIV: a single-center, prospective observational study. AIDS. 2020;34(12):1775–80. https://doi.org/10.1097/QAD.0000000000002643.
Del Amo J, Polo R, Moreno S, Díaz A, Martínez E, Arribas JR, et al. Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy: a cohort study. Ann Intern Med. 2020;173(7):536–41. https://doi.org/10.7326/M20-3689.
Geretti AM, Stockdale AJ, Kelly SH, Cevik M, Collins S, Waters L, et al. Outcomes of coronavirus disease 2019 (COVID-19) related hospitalization among people with human immunodeficiency virus (HIV) in the ISARIC World Health Organization (WHO) Clinical Characterization Protocol (UK): a prospective observational study. Clin Infect Dis. 2021;73(7):e2095–106. https://doi.org/10.1093/cid/ciaa1605.
Bhaskaran K, Rentsch CT, MacKenna B, Schultze A, Mehrkar A, Bates CJ, et al. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV. 2021;8(1):e24–32. https://doi.org/10.1016/S2352-3018(20)30305-2.
Ceballos ME, Ross P, Lasso M, Dominguez I, Puente M, Valenzuela P, et al. Clinical characteristics and outcomes of people living with HIV hospitalized with COVID-19: a nationwide experience. Int J STD AIDS. 2021;32(5):435–43. https://doi.org/10.1177/0956462420973106.
Bertagnolio S, Thwin SS, Silva R, Nagarajan S, Jassat W, Fowler R, et al. Clinical features of, and risk factors for, severe or fatal COVID-19 among people living with HIV admitted to hospital: analysis of data from the WHO Global Clinical Platform of COVID-19. Lancet HIV. 2022;9(7):e486–95. https://doi.org/10.1016/S2352-3018(22)00097-2.
Hoffman SA, Costales C, Sahoo MK, Palanisamy S, Yamamoto F, Huang C, et al. SARS-CoV-2 neutralization resistance mutations in patient with HIV/AIDS, California, USA. Emerg Infect Dis. 2021;27(10):2720–3. https://doi.org/10.3201/eid2710.211461.
Vizcarra P, Pérez-Elías MJ, Quereda C, Moreno A, Vivancos MJ, Dronda F, et al. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. Lancet HIV. 2020;7(8):e554–64. https://doi.org/10.1016/S2352-3018(20)30164-8.
Shalev N, Scherer M, LaSota ED, Antoniou P, Yin MT, Zucker J, et al. Clinical characteristics and outcomes in people living with human immunodeficiency virus hospitalized for coronavirus disease 2019. Clin Infect Dis. 2020;71(16):2294–7. https://doi.org/10.1093/cid/ciaa635.
Lee MJ, Snell LB, Douthwaite ST, Fidler S, Fitzgerald N, Goodwin L, et al. Clinical outcomes of patients with and without HIV hospitalized with COVID-19 in England during the early stages of the pandemic: a matched retrospective multi-centre analysis (RECEDE-C19 study). HIV Med. 2022;23(2):121–33. https://doi.org/10.1111/hiv.13174.
Bachelard A, Sautereau A, Digumber M, Isernia V, Phung B, Lehur AC, et al. Risk factors associated with severe/critical COVID-19 in people living with HIV-1. Int J Infect Dis. 2022;122:152–4. https://doi.org/10.1016/j.ijid.2022.05.055.
Olalla-Sierra J, Martín-Escalante MD, García-Alegría J, Rubio-Rivas M, de Miguel-Campo B, Zurita-Etayo M, et al. Coronavirus disease 2019 hospitalization outcomes in persons with and without HIV in Spain. AIDS. 2022;36(5):683–90. https://doi.org/10.1097/QAD.0000000000003056.
Favara G, Barchitta M, Maugeri A, Faro G, Agodi A. HIV infection does not affect the risk of death of COVID-19 patients: a systematic review and meta-analysis of epidemiological studies. J Glob Health. 2022;12:05036. https://doi.org/10.7189/jogh.12.05036.
• Del Amo J, Polo R, Moreno S, Jarrín I, Hernán MA. SARS-CoV-2 infection and coronavirus disease 2019 severity in persons with HIV on antiretroviral treatment. AIDS. 2022;36(2):161–8. https://doi.org/10.1097/QAD.0000000000003132. (Recent literature review which critically examined incidence and clinical outcome of COVID-19 in PLWH, showing that the risk of SARS-CoV-2 infection in such population is not hightnened and that clinical severity is not homogeneous among PLWH, increasing with age and baseline comorbidities.)
Li G, Park LS, Lodi S, Logan RW, Cartwright EJ, Aoun-Barakat L, et al. Tenofovir disoproxil fumarate and coronavirus disease 2019 outcomes in men with HIV. AIDS. 2022;36(12):1689–96. https://doi.org/10.1097/QAD.0000000000003314.
Del Amo J, Polo R, Moreno S, Martínez E, Cabello A, Iribarren JA, et al. Tenofovir disoproxil fumarate/emtricitabine and severity of coronavirus disease 2019 in people with HIV infection. AIDS. 2022;36(15):2171–9. https://doi.org/10.1097/QAD.0000000000003372.
Ayerdi O, Puerta T, Clavo P, Vera M, Ballesteros J, Fuentes ME, et al. Preventive efficacy of tenofovir/emtricitabine against severe acute respiratory syndrome coronavirus 2 among pre-exposure prophylaxis users. Open Forum Infect Dis. 2020;7(11):ofaa455. https://doi.org/10.1093/ofid/ofaa455.
Fernandes DE, Ferreira PRA, Mastroianni KG. Pre-exposure prophylaxis during the SARS-CoV-2 pandemic: can PrEP prevent COVID-19-related symptoms? Epidemiol Infect. 2020;148:e231. https://doi.org/10.1017/S0950268820002253.
Elfiky AA. Ribavirin, Remdesivir, Sofosbuvir, Galidesivir, and Tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): a molecular docking study. Life Sci. 2020;253:117592. https://doi.org/10.1016/j.lfs.2020.117592.
Zanella I, Zizioli D, Castelli F, Quiros-Roldan E. Tenofovir, another inexpensive, well-known and widely available old drug repurposed for SARS-COV-2 infection. Pharmaceuticals (Basel). 2021;14(5). https://doi.org/10.3390/ph14050454.
Nomah DK, Reyes-Urueña J, Díaz Y, Moreno S, Aceiton J, Bruguera A, et al. Impact of tenofovir on SARS-CoV-2 infection and severe outcomes among people living with HIV: a propensity score-matched study. J Antimicrob Chemother. 2022;77(8):2265–73. https://doi.org/10.1093/jac/dkac177.
Akbarialiabad H, Taghrir MH, Abdollahi A, Ghahramani N, Kumar M, Paydar S, et al. Long COVID, a comprehensive systematic scoping review. Infection. 2021;49(6):1163–86. https://doi.org/10.1007/s15010-021-01666-x.
Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier CML, Patel SK, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol. 2022;23(2):210–6. https://doi.org/10.1038/s41590-021-01113-x.
Spinelli MA, Peluso MJ, Lynch KL, Yun C, Glidden DV, Henrich TJ, et al. Differences in post-mRNA vaccination SARS-CoV-2 IgG concentrations and surrogate virus neutralization test response by HIV status and type of vaccine: a matched case-control observational study. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab1009.
Lv T, Cao W, Li T. HIV-related immune activation and inflammation: current understanding and strategies. J Immunol Res. 2021;2021:7316456. https://doi.org/10.1155/2021/7316456.
Deeks SG, Tracy R, Douek DC. Systemic effects of inflammation on health during chronic HIV infection. Immunity. 2013;39(4):633–45. https://doi.org/10.1016/j.immuni.2013.10.001.
Kingery JR, Safford MM, Martin P, Lau JD, Rajan M, Wehmeyer GT, et al. Health status, persistent symptoms, and effort intolerance one year after acute COVID-19 infection. J Gen Intern Med. 2022;37(5):1218–25. https://doi.org/10.1007/s11606-021-07379-z.
• Peluso MJ, Spinelli MA, Deveau TM, Forman CA, Munter SE, Mathur S, et al. Postacute sequelae and adaptive immune responses in people with HIV recovering from SARS-COV-2 infection. AIDS. 2022;36(12):F7–16. https://doi.org/10.1097/QAD.0000000000003338. (This study showed that in the backdrop of similar humoral responses compared to HIV-uninfected individuals, PLWH recovering from COVID-19 display fewer SARS-CoV-2–specific CD8+ T-cells and greater exhaustion of CD4+ T-cells; furthermore, PLWH show a higher risk of developing PASC when adjusting for other factors.)
Park A, Iwasaki A. Type I and type III interferons - induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020;27(6):870–8. https://doi.org/10.1016/j.chom.2020.05.008.
Sa Ribero M, Jouvenet N, Dreux M, Nisole S. Interplay between SARS-CoV-2 and the type I interferon response. PLoS Pathog. 2020;16(7):e1008737. https://doi.org/10.1371/journal.ppat.1008737.
Lei X, Dong X, Ma R, Wang W, Xiao X, Tian Z, et al. Activation and evasion of type I interferon responses by SARS-CoV-2. Nat Commun. 2020;11(1):3810. https://doi.org/10.1038/s41467-020-17665-9.
Zhang Q, Bastard P, Liu Z, Le Pen J, Moncada-Velez M, Chen J, et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370(6515). https://doi.org/10.1126/science.abd4570.
Bastard P, Rosen LB, Zhang Q, Michailidis E, Hoffmann HH, Zhang Y, et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020;370(6515). https://doi.org/10.1126/science.abd4585.
Scagnolari C, Antonelli G. Type I interferon and HIV: subtle balance between antiviral activity, immunopathogenesis and the microbiome. Cytokine Growth Factor Rev. 2018;40:19–31. https://doi.org/10.1016/j.cytogfr.2018.03.003.
Bosinger SE, Utay NS. Type I interferon: understanding its role in HIV pathogenesis and therapy. Curr HIV/AIDS Rep. 2015;12(1):41–53. https://doi.org/10.1007/s11904-014-0244-6.
• Fardoos R, Asowata OE, Herbert N, Nyquist SK, Zungu Y, Singh A, et al. HIV infection drives interferon signaling within intestinal SARS-CoV-2 target cells. JCI Insight. 2021;6(16). https://doi.org/10.1172/jci.insight.148920. (This study showed that chronic HIV infection drives a constitutive activation of the type-I interferon pathways within absorptive enterocytes, which, however, does not prevent SARS-CoV-2 infection in this compartment.)
Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861–80. https://doi.org/10.1016/j.cell.2021.01.007.
Rovito R, Augello M, Ben-Haim A, Bono V, d’Arminio Monforte A, Marchetti G. Hallmarks of severe COVID-19 pathogenesis:. Front Immunol. 2022;13:912336. https://doi.org/10.3389/fimmu.2022.912336.
Tincati C, Cannizzo ES, Giacomelli M, Badolato R, d’Arminio Monforte A, Marchetti G. Heightened circulating interferon-inducible chemokines, and activated pro-cytolytic Th1-cell phenotype features Covid-19 aggravation in the second week of illness. Front Immunol. 2020;11:580987. https://doi.org/10.3389/fimmu.2020.580987.
Fenwick C, Joo V, Jacquier P, Noto A, Banga R, Perreau M, et al. T-cell exhaustion in HIV infection. Immunol Rev. 2019;292(1):149–63. https://doi.org/10.1111/imr.12823.
Bussmann BM, Reiche S, Bieniek B, Krznaric I, Ackermann F, Jassoy C. Loss of HIV-specific memory B-cells as a potential mechanism for the dysfunction of the humoral immune response against HIV. Virology. 2010;397(1):7–13. https://doi.org/10.1016/j.virol.2009.11.003.
•• Pontelli MC, Castro Í, Martins RB, La Serra L, Veras FP, Nascimento DC, et al. SARS-CoV-2 productively infects primary human immune system cells in vitro and in COVID-19 patients. J Mol Cell Biol. 2022;14(4). https://doi.org/10.1093/jmcb/mjac021. (This study showed that monocytes, as well as both B and T lymphocytes, are susceptible to SARS-CoV-2 infection in vitro, accumulating double-stranded RNA consistent with viral RNA replication and ultimately leading to expressive T cell apoptosis.)
•• Shen XR, Geng R, Li Q, Chen Y, Li SF, Wang Q, et al. ACE2-independent infection of T lymphocytes by SARS-CoV-2. Signal Transduct Target Ther. 2022;7(1):83. https://doi.org/10.1038/s41392-022-00919-x. (This study reports that SARS-CoV-2 is able to productively infect CD4+ T-cells binding to cell entry receptors other than ACE2 (most likely LFA-1) and to induce their apoptosis which is probably dependent on mitochondria ROS-hypoxia pathways.)
Bono V, Augello M, Tincati C, Marchetti G. Failure of CD4+ T-cell recovery upon virally-effective cART: an enduring gap in the understanding of HIV+ immunological non-responders. New Microbiol. 2022;45(3):155–72.
Sharov KS. HIV/SARS-CoV-2 co-infection: T cell profile, cytokine dynamics and role of exhausted lymphocytes. Int J Infect Dis. 2021;102:163–9. https://doi.org/10.1016/j.ijid.2020.10.049.
•• Nkosi T, Chasara C, Papadopoulos AO, Nguni TL, Karim F, Moosa MS, et al. Unsuppressed HIV infection impairs T cell responses to SARS-CoV-2 infection and abrogates T cell cross-recognition. Elife. 2022;11. https://doi.org/10.7554/eLife.78374. (This study showed that individuals with unsuppressed HIV infection mount weak antigen-specific CD4+ and CD8+ T-cell responses to SARS-CoV-2 and poorly recognize SARS-CoV-2 Beta variant.)
•• Alrubayyi A, Gea-Mallorquí E, Touizer E, Hameiri-Bowen D, Kopycinski J, Charlton B, et al. Characterization of humoral and SARS-CoV-2 specific T cell responses in people living with HIV. Nat Commun. 2021;12(1):5839. https://doi.org/10.1038/s41467-021-26137-7. (This study reported that while T-cell responses against structural and non-structural SARS-CoV-2 proteins in the convalescent phase of mild COVID-19 are similar in PLWH with cART-suppressed HIV viral load and HIV-negative subjects overall, the magnitude of SARS-CoV-2–specific T-cell responses is positively related with the CD4/CD8 ratio and the size of naïve CD4 T-cell pool in PLWH.)
Riou C, du Bruyn E, Stek C, Daroowala R, Goliath RT, Abrahams F, et al. Relationship of SARS-CoV-2-specific CD4 response to COVID-19 severity and impact of HIV-1 and tuberculosis coinfection. J Clin Invest. 2021;131(12). https://doi.org/10.1172/JCI149125.
•• Donadeu L, Tiraboschi JM, Scévola S, Torija A, Meneghini M, Jouve T, et al. Long-lasting adaptive immune memory specific to SARS-CoV-2 in convalescent COVID-19 stable people living with HIV. AIDS. 2022. https://doi.org/10.1097/QAD.0000000000003276. (This study showed that COVID-19-recovered PLWH with well-controlled HIV infection are capable of developing and maintaining up to six months a robust adaptive SARS-CoV-2–specific T- and B-cellular response similarly to people without HIV, suggesting that magnitude and persistence of the immune response after SARS-CoV-2 infection are mainly driven by the degree of COVID-19 clinical severity, with severe patients exhibiting higher immune responses.)
Giannone D, Vecchione MB, Czernikier A, Polo ML, Gonzalez Polo V, Cruces L, et al. SARS-CoV-2 humoral and cellular immune responses in COVID-19 convalescent individuals with HIV. J Infect. 2022;85(3):334–63. https://doi.org/10.1016/j.jinf.2022.05.026.
Alcaide ML, Nogueira NF, Salazar AS, Montgomerie EK, Rodriguez VJ, Raccamarich PD, et al. A Longitudinal analysis of SARS-CoV-2 antibody responses among people with HIV. Front Med (Lausanne). 2022;9:768138. https://doi.org/10.3389/fmed.2022.768138.
Snyman J, Hwa SH, Krause R, Muema D, Reddy T, Ganga Y, et al. Similar antibody responses against severe acute respiratory syndrome coronavirus 2 in individuals living without and with human immunodeficiency virus on antiretroviral therapy during the first South African infection wave. Clin Infect Dis. 2022;75(1):e249–56. https://doi.org/10.1093/cid/ciab758.
Spinelli MA, Lynch KL, Yun C, Glidden DV, Peluso MJ, Henrich TJ, et al. SARS-CoV-2 seroprevalence, and IgG concentration and pseudovirus neutralising antibody titres after infection, compared by HIV status: a matched case-control observational study. Lancet HIV. 2021;8(6):e334–41. https://doi.org/10.1016/S2352-3018(21)00072-2.
Liu Y, Xiao Y, Wu S, Marley G, Ming F, Wang X, et al. People living with HIV easily lose their immune response to SARS-CoV-2: result from a cohort of COVID-19 cases in Wuhan, China. BMC Infect Dis. 2021;21(1):1029. https://doi.org/10.1186/s12879-021-06723-2.
Khan K, Lustig G, Bernstein M, Archary D, Cele S, Karim F, et al. Immunogenicity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and Ad26.CoV2.S vaccination in people living with human immunodeficiency virus (HIV). Clin Infect Dis. 2022;75(1):e857–64. https://doi.org/10.1093/cid/ciab1008.
Schuster DJ, Karuna S, Brackett C, Wesley MS, Li SS, Eisel N, et al. Lower SARS-CoV-2 specific humoral immunity in people living with HIV-1 recovered from non-hospitalized COVID-19. JCI Insight. 2022. https://doi.org/10.1172/jci.insight.158402.
Ho HE, Peluso MJ, Margus C, Matias Lopes JP, He C, Gaisa MM, et al. Clinical Outcomes and immunologic characteristics of coronavirus disease 2019 in people with human immunodeficiency virus. J Infect Dis. 2021;223(3):403–8. https://doi.org/10.1093/infdis/jiaa380.
Vergori A, Boschini A, Notari S, Lorenzini P, Castilletti C, Colavita F, et al. SARS-CoV-2 specific immune response and inflammatory profile in advanced HIV-infected persons during a COVID-19 outbreak. Viruses. 2022;14(7). https://doi.org/10.3390/v14071575.
Israelow B, Mao T, Klein J, Song E, Menasche B, Omer SB, et al. Adaptive immune determinants of viral clearance and protection in mouse models of SARS-CoV-2. Sci Immunol. 2021;6(64):eabl4509. https://doi.org/10.1126/sciimmunol.abl4509.
Robson F, Khan KS, Le TK, Paris C, Demirbag S, Barfuss P, et al. Coronavirus RNA proofreading: molecular basis and therapeutic targeting. Mol Cell. 2020;79(5):710–27. https://doi.org/10.1016/j.molcel.2020.07.027.
Chen L, Zody MC, Di Germanio C, Martinelli R, Mediavilla JR, Cunningham MH, et al. Emergence of multiple SARS-CoV-2 antibody escape variants in an immunocompromised host undergoing convalescent plasma treatment. mSphere. 2021;6(4):e0048021. https://doi.org/10.1128/mSphere.00480-21.
Choi B, Choudhary MC, Regan J, Sparks JA, Padera RF, Qiu X, et al. Persistence and evolution of SARS-CoV-2 in an immunocompromised host. N Engl J Med. 2020;383(23):2291–3. https://doi.org/10.1056/NEJMc2031364.
Clark SA, Clark LE, Pan J, Coscia A, McKay LGA, Shankar S, et al. SARS-CoV-2 evolution in an immunocompromised host reveals shared neutralization escape mechanisms. Cell. 2021;184(10):2605-17.e18. https://doi.org/10.1016/j.cell.2021.03.027.
•• Cele S, Karim F, Lustig G, San JE, Hermanus T, Tegally H, et al. SARS-CoV-2 prolonged infection during advanced HIV disease evolves extensive immune escape. Cell Host Microbe. 2022;30(2):154-62.e5. https://doi.org/10.1016/j.chom.2022.01.005. (This study showed that advanced HIV disease may determine prolonged SARS-CoV-2 infection, with subsequent evolution of a multitude of mutations conferring extensive escape from antibody neutralization.)
Riddell AC, Kele B, Harris K, Bible J, Murphy M, Dakshina S, et al. Generation of novel SARS-CoV-2 variants on B.1.1.7 lineage in three patients with advanced HIV disease. Clin Infect Dis. 2022. https://doi.org/10.1093/cid/ciac409.
Spinicci M, Mazzoni A, Borchi B, Graziani L, Mazzetti M, Bartalesi F, et al. AIDS patient with severe T cell depletion achieved control but not clearance of SARS-CoV-2 infection. Eur J Immunol. 2022;52(2):352–5. https://doi.org/10.1002/eji.202149574.
World Health Organization. WHO SAGE Roadmap for prioritizing uses of COVID-19 vaccines. https://www.who.int/publications/i/item/who-sage-roadmap-for-prioritizing-uses-of-covid-19-vaccines. Accessed 1 Oct 2022
van den Berg R, van Hoogstraten I, van Agtmael M. Non-responsiveness to hepatitis B vaccination in HIV seropositive patients; possible causes and solutions. AIDS Rev. 2009;11(3):157–64.
Avelino-Silva VI, Miyaji KT, Hunt PW, Huang Y, Simoes M, Lima SB, et al. CD4/CD8 ratio and KT ratio predict yellow fever vaccine immunogenicity in HIV-infected patients. PLoS Negl Trop Dis. 2016;10(12):e0005219. https://doi.org/10.1371/journal.pntd.0005219.
Kroon FP, van Dissel JT, Labadie J, van Loon AM, van Furth R. Antibody response to diphtheria, tetanus, and poliomyelitis vaccines in relation to the number of CD4+ T lymphocytes in adults infected with human immunodeficiency virus. Clin Infect Dis. 1995;21(5):1197–203. https://doi.org/10.1093/clinids/21.5.1197.
Kernéis S, Launay O, Turbelin C, Batteux F, Hanslik T, Boëlle PY. Long-term immune responses to vaccination in HIV-infected patients: a systematic review and meta-analysis. Clin Infect Dis. 2014;58(8):1130–9. https://doi.org/10.1093/cid/cit937.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16. https://doi.org/10.1056/NEJMoa2035389.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15. https://doi.org/10.1056/NEJMoa2034577.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99–111. https://doi.org/10.1016/S0140-6736(20)32661-1.
Coburn SB, Humes E, Lang R, Stewart C, Hogan BC, Gebo KA, et al. Analysis of postvaccination breakthrough COVID-19 infections among adults with HIV in the United States. JAMA Netw Open. 2022;5(6):e2215934. https://doi.org/10.1001/jamanetworkopen.2022.15934.
Sun J, Zheng Q, Madhira V, Olex AL, Anzalone AJ, Vinson A, et al. Association between immune dysfunction and COVID-19 breakthrough infection after SARS-CoV-2 vaccination in the US. JAMA Intern Med. 2022;182(2):153–62. https://doi.org/10.1001/jamainternmed.2021.7024.
Levy I, Wieder-Finesod A, Litchevsky V, Biber A, Indenbaum V, Olmer L, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in people living with HIV-1. Clin Microbiol Infect. 2021;27(12):1851–5. https://doi.org/10.1016/j.cmi.2021.07.031.
Bozzi G, Lombardi A, Ludovisi S, Muscatello A, Manganaro L, Cattaneo D, et al. Transient increase in plasma HIV RNA after COVID-19 vaccination with mRNA-1272. Int J Infect Dis. 2021;113:125–6. https://doi.org/10.1016/j.ijid.2021.10.021.
Cheeseman SH, Davaro RE, Ellison RT. Hepatitis B vaccination and plasma HIV-1 RNA. N Engl J Med. 1996;334(19):1272. https://doi.org/10.1056/NEJM199605093341916.
Glesby MJ, Hoover DR, Farzadegan H, Margolick JB, Saah AJ. The effect of influenza vaccination on human immunodeficiency virus type 1 load: a randomized, double-blind, placebo-controlled study. J Infect Dis. 1996;174(6):1332–6. https://doi.org/10.1093/infdis/174.6.1332.
Brichacek B, Swindells S, Janoff EN, Pirruccello S, Stevenson M. Increased plasma human immunodeficiency virus type 1 burden following antigenic challenge with pneumococcal vaccine. J Infect Dis. 1996;174(6):1191–9. https://doi.org/10.1093/infdis/174.6.1191.
Yek C, Gianella S, Plana M, Castro P, Scheffler K, García F, et al. Standard vaccines increase HIV-1 transcription during antiretroviral therapy. AIDS. 2016;30(15):2289–98. https://doi.org/10.1097/QAD.0000000000001201.
• Stevenson EM, Terry S, Copertino D, Leyre L, Danesh A, Weiler J, et al. SARS CoV-2 mRNA vaccination exposes latent HIV to Nef-specific CD8. Nat Commun. 2022;13(1):4888. https://doi.org/10.1038/s41467-022-32376-z. (This interesting study showed that BNT162b2 vaccine activates the RIG-I/TLR–TNF–NFkB axis, resulting in transcription of HIV proviruses; in parallel, Nef-specific CD8+ T-cells increase and acquire cytotoxic effector functions, which correlate with reduction of cell-associated HIV-mRNA, suggesting killing or suppression of cells transcribing HIV; however, significant depletion of intact proviruses was not observed, highlighting challenges to achieving HIV reservoir reductions.)
• Nault L, Marchitto L, Goyette G, Tremblay-Sher D, Fortin C, Martel-Laferrière V, et al. Covid-19 vaccine immunogenicity in people living with HIV-1. Vaccine. 2022;40(26):3633–7. https://doi.org/10.1016/j.vaccine.2022.04.090. (This study reported that humoral immune responses to mRNA-1273 vaccine are similar to those of HIV-negative controls in PLWH with CD4+ T-cell counts >250/μL, yet lower in those with CD4+ T-cell counts <250/μL.)
•• Antinori A, Cicalini S, Meschi S, Bordoni V, Lorenzini P, Vergori A, et al. Humoral and cellular immune response elicited by mRNA vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in people living with human immunodeficiency virus receiving antiretroviral therapy based on current CD4 T-lymphocyte count. Clin Infect Dis. 2022;75(1):e552–63. https://doi.org/10.1093/cid/ciac238. (This study showed that humoral and T-cell responses to mRNA vaccination are significantly impaired in PLWH with CD4+ T-cell counts <200/μL, but comparable to those of the general population in PLWH with good CD4+ T-cell counts.)
Woldemeskel BA, Karaba AH, Garliss CC, Beck EJ, Wang KH, Laeyendecker O, et al. The BNT162b2 mRNA vaccine elicits robust humoral and cellular immune responses in people living with human immunodeficiency virus (HIV). Clin Infect Dis. 2022;74(7):1268–70. https://doi.org/10.1093/cid/ciab648.
• Sisteré-Oró M, Andrade N, Wortmann DDJ, Du J, Garcia-Giralt N, González-Cao M, et al. Anti-SARS-COV-2 specific immunity in HIV immunological non-responders after mRNA-based COVID-19 vaccination. Front Immunol. 2022;13:994173. https://doi.org/10.3389/fimmu.2022.994173. (This study reported that immune responses to BNT162b2 vaccine are insufficient in 50% of immunological non-responder PLWH (CD4+ T-cell counts <350/μL), whereas a booster vaccination is able to generate a SARS-CoV-2–specific T-cell response.)
Tau L, Turner D, Adler A, Marom R, Ahsanov S, Matus N, et al. SARS-CoV-2 humoral and cellular immune responses of patients with HIV after vaccination with BNT162b2 mRNA COVID-19 vaccine in the Tel-Aviv Medical Center. Open Forum Infect Dis. 2022;9(4):ofac089. https://doi.org/10.1093/ofid/ofac089.
Spinelli MA, Peluso MJ, Lynch KL, Yun C, Glidden DV, Henrich TJ, et al. Differences in post-mRNA vaccination severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) immunoglobulin G (IgG) concentrations and surrogate virus neutralization test response by human immunodeficiency virus (HIV) status and type of vaccine: a matched case-control observational study. Clin Infect Dis. 2022;75(1):e916–9. https://doi.org/10.1093/cid/ciab1009.
• Benet S, Blanch-Lombarte O, Ainsua-Enrich E, Pedreño-Lopez N, Muñoz-Basagoiti J, Raïch-Regué D, et al. Limited humoral and specific T-cell responses after SARS-CoV-2 vaccination in PLWH with poor immune reconstitution. J Infect Dis. 2022. https://doi.org/10.1093/infdis/jiac406. (This study showed lower immune responses to mRNA vaccines in PLWH with CD4+ T-cell counts <200/μL; furthermore, neutralizing capacity and specific T-cell responses (against wild-type SARS-CoV-2 and VOCs like Alpha, Delta, Kappa) are absent or reduced in a higher percentage of PLWH with CD4+ T-cell counts <200/μL.)
•• Vergori A, Cozzi Lepri A, Cicalini S, Matusali G, Bordoni V, Lanini S, et al. Immunogenicity to COVID-19 mRNA vaccine third dose in people living with HIV. Nat Commun. 2022;13(1):4922. https://doi.org/10.1038/s41467-022-32263-7. (This study displayed that a third dose of a mRNA vaccine following the primary cycle strongly boost humoral albeit not T-cell responses in PLWH presenting with advanced disease at the time of HIV diagnosis (CD4+ T-cells <200/μL and/or AIDS), irrespective of the current CD4+ T-cell count.)
Pourcher V, Belin L, Soulie C, Rosenzwajg M, Marot S, Lacombe K, et al. High seroconversion rate and SARS-CoV-2 Delta neutralization in people with HIV vaccinated with BNT162b2. AIDS. 2022;36(11):1545–52. https://doi.org/10.1097/QAD.0000000000003300.
Augello M, Bono V, Rovito R, Yellenki V, Tincati C, d’Arminio Monforte A, et al. T-cell and humoral responses to mRNA-1273 vaccine up to 6 months in late presenter (LP) people living with HIV (PLWH). HIV Glasgow, 23–26 October 2022, Glasgow, UK / Virtual. J Int AIDS Soc. 25: e26009. https://doi.org/10.1002/jia2.26009
•• Frater J, Ewer KJ, Ogbe A, Pace M, Adele S, Adland E, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: a single-arm substudy of a phase 2/3 clinical trial. Lancet HIV. 2021;8(8):e474–85. https://doi.org/10.1016/S2352-3018(21)00103-X. (This study showed comparable magnitude and durability of humoral and T-cell responses in PLWH and HIV-negative controls after ChAdOx1-S vaccination.)
Ogbe A, Pace M, Bittaye M, Tipoe T, Adele S, Alagaratnam J, et al. Durability of ChAdOx1 nCoV-19 vaccination in people living with HIV. JCI Insight. 2022;7(7). https://doi.org/10.1172/jci.insight.157031
Madhi SA, Koen AL, Izu A, Fairlie L, Cutland CL, Baillie V, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in people living with and without HIV in South Africa: an interim analysis of a randomised, double-blind, placebo-controlled, phase 1B/2A trial. Lancet HIV. 2021;8(9):e568–80. https://doi.org/10.1016/S2352-3018(21)00157-0.
• Madhi SA, Moodley D, Hanley S, Archary M, Hoosain Z, Lalloo U, et al. Immunogenicity and safety of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine in people living with and without HIV-1 infection: a randomised, controlled, phase 2A/2B trial. Lancet HIV. 2022;9(5):e309–22. https://doi.org/10.1016/S2352-3018(22)00041-8. (This study reported that humoral responses to NVX-CoV2373 are lower in PLWH as compared to people without HIV, especially in those without prior SARS-CoV-2 infection.)
Liu Y, Han J, Li X, Chen D, Zhao X, Qiu Y, et al. COVID-19 vaccination in people living with HIV (PLWH) in China: a cross sectional study of vaccine hesitancy, safety, and immunogenicity. Vaccines (Basel). 2021;9(12). https://doi.org/10.3390/vaccines9121458.
• Feng Y, Zhang Y, He Z, Huang H, Tian X, Wang G, et al. Immunogenicity of an inactivated SARS-CoV-2 vaccine in people living with HIV-1: a non-randomized cohort study. EClinicalMedicine. 2022;43:101226. https://doi.org/10.1016/j.eclinm.2021.101226. (This study showed that BBIBP-CorV is able to induce similar anti-RBD Ig, neutralization activity, and T-cell responses between HIV-negative individuals and PLWH overall; however, humoral responses are weaker in PLWH with low CD4/CD8 ratio compared to PLWH with medium or high ratio.)
Han X, Yu X, Han Y, Fang Q, Shen C, Liu H, et al. Safety and immunogenicity of inactivated COVID-19 vaccines among people living with HIV in China. Infect Drug Resist. 2022;15:2091–100. https://doi.org/10.2147/IDR.S353127.
Zeng G, Xu L, Feng S, Tang J, Wang X, Li G, et al. IgG antibody responses and immune persistence of two doses of BBIBP-CorV vaccine or CoronaVac vaccine in people living with HIV (PLWH) in Shenzhen, China. Vaccines (Basel). 2022;10(6). https://doi.org/10.3390/vaccines10060880.
Wong NS, Wong BCK, Chan JMC, Wong KH, Tsang OTY, Mok CKP, et al. Surrogate neutralization responses following severe acute respiratory syndrome coronavirus 2 vaccination in people with HIV: comparison between inactivated and mRNA vaccine. AIDS. 2022;36(9):1255–64. https://doi.org/10.1097/QAD.0000000000003237.
Noe S, Ochana N, Wiese C, Schabaz F, Von Krosigk A, Heldwein S, et al. Humoral response to SARS-CoV-2 vaccines in people living with HIV. Infection. 2022;50(3):617–23. https://doi.org/10.1007/s15010-021-01721-7.
Lapointe HR, Mwimanzi F, Cheung PK, Sang Y, Yaseen F, Umviligihozo G, et al. People with HIV receiving suppressive antiretroviral therapy show typical antibody durability after dual COVID-19 vaccination, and strong third dose responses. J Infect Dis. 2022. https://doi.org/10.1093/infdis/jiac229.
• Corma-Gómez A, Fernández-Fuertes M, García E, Fuentes-López A, Gómez-Ayerbe C, Rivero-Juárez A, et al. Severe immunosuppression is related to poorer immunogenicity to SARS-CoV-2 vaccines among people living with HIV. Clin Microbiol Infect. 2022;28(11):1492–8. https://doi.org/10.1016/j.cmi.2022.05.018. (This study reported lower humoral responses to SARS-CoV-2 vaccines in PLWH with low CD4+ T-cell counts; furthermore, mRNA vaccines are associated with a higher response than adenoviral vector vaccines.)
Brumme ZL, Mwimanzi F, Lapointe HR, Cheung PK, Sang Y, Duncan MC, et al. Humoral immune responses to COVID-19 vaccination in people living with HIV receiving suppressive antiretroviral therapy. NPJ Vaccines. 2022;7(1):28. https://doi.org/10.1038/s41541-022-00452-6.
Chammartin F, Kusejko K, Pasin C, Trkola A, Briel M, Amico P, et al. Determinants of antibody response to severe acute respiratory syndrome coronavirus 2 mRNA vaccines in people with HIV. AIDS. 2022;36(10):1465–8. https://doi.org/10.1097/QAD.0000000000003246.
World Health Organization. WHO SAGE Roadmap for prioritizing uses of COVID-19 vaccines. https://www.who.int/publications/i/item/WHO-2019-nCoV-Vaccines-SAGE-Prioritization-2022.1. Accessed 1 Oct 2022
Lombardi A, Butta GM, Donnici L, Bozzi G, Oggioni M, Bono P, et al. Anti-spike antibodies and neutralising antibody activity in people living with HIV vaccinated with COVID-19 mRNA-1273 vaccine: a prospective single-centre cohort study. Lancet Reg Health Eur. 2022;13:100287. https://doi.org/10.1016/j.lanepe.2021.100287.
Goel RR, Painter MM, Apostolidis SA, Mathew D, Meng W, Rosenfeld AM, et al. mRNA vaccines induce durable immune memory to SARS-CoV-2 and variants of concern. Science. 2021;374(6572):abm0829. https://doi.org/10.1126/science.abm0829.
Agrati C, Castilletti C, Goletti D, Sacchi A, Bordoni V, Mariotti D, et al. Persistent spike-specific T cell immunity despite antibody reduction after 3 months from SARS-CoV-2 BNT162b2-mRNA vaccine. Sci Rep. 2022;12(1):6687. https://doi.org/10.1038/s41598-022-07741-z.
• Woldemeskel BA, Karaba AH, Garliss CC, Beck EJ, Aytenfisu TY, Johnston TS, et al. Decay of coronavirus disease 2019 mRNA vaccine-induced immunity in people with HIV. AIDS. 2022;36(9):1315–7. https://doi.org/10.1097/QAD.0000000000003263. (This study reported waning antibody responses (especially to VOCs) but persistent T-cell responses 6 months post vaccination in PLWH.)
Tuan JJ, Zapata H, Barakat L, Andrews L, Behnegar A, Kim YW, et al. Long-term quantitative assessment of anti-SARS-CoV-2 spike protein immunogenicity (QUASI) after COVID-19 vaccination in older people living with HIV (PWH). BMC Infect Dis. 2022;22(1):744. https://doi.org/10.1186/s12879-022-07737-0.
Jedicke N, Stankov MV, Cossmann A, Dopfer-Jablonka A, Knuth C, Ahrenstorf G, et al. Humoral immune response following prime and boost BNT162b2 vaccination in people living with HIV on antiretroviral therapy. HIV Med. 2022;23(5):558–63. https://doi.org/10.1111/hiv.13202.
Milano E, Ricciardi A, Casciaro R, Pallara E, De Vita E, Bavaro DF, et al. Immunogenicity and safety of the BNT162b2 COVID-19 mRNA vaccine in PLWH: a monocentric study in Bari. Italy J Med Virol. 2022;94(5):2230–6. https://doi.org/10.1002/jmv.27629.
Schmidt KG, Harrer EG, Tascilar K, Kübel S, El Kenz B, Hartmann F, et al. Characterization of serum and mucosal SARS-CoV-2-antibodies in HIV-1-infected subjects after BNT162b2 mRNA vaccination or SARS-CoV-2 infection. Viruses. 2022;14(3). https://doi.org/10.3390/v14030651.
de González AM, Cañizares A, Vázquez-Rodríguez P, Castro Á, Moldes L, López S, et al. Safety and immunogenicity of SARS-CoV-2 vaccines in people with HIV. AIDS. 2022;36(5):691–5. https://doi.org/10.1097/QAD.0000000000003161.
• Vergori A, Cozzi-Lepri A, Matusali G, Colavita F, Cicalini S, Gallì P, et al. SARS-CoV-2 Omicron variant neutralization after third dose vaccination in PLWH. Viruses. 2022;14(8). https://doi.org/10.3390/v14081710. (This study showed that a third dose of mRNA vaccination is able to strongly increase the neutralizing activity against Omicron variant (BA.1)—which remains poorer than that against the original W-D614G strain—regardless of HIV status.)
Ruddy JA, Boyarsky BJ, Bailey JR, Karaba AH, Garonzik-Wang JM, Segev DL, et al. Safety and antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in persons with HIV. AIDS. 2021;35(14):2399–401. https://doi.org/10.1097/QAD.0000000000003017.
Hassold N, Brichler S, Ouedraogo E, Leclerc D, Carroue S, Gater Y, et al. Impaired antibody response to COVID-19 vaccination in advanced HIV infection. AIDS. 2022;36(4):F1–5. https://doi.org/10.1097/QAD.0000000000003166.
Cai S, Liao G, Yu T, Gao Q, Zou L, Zhang H, et al. Immunogenicity and safety of an inactivated SARS-CoV-2 vaccine in people living with HIV: a cross-sectional study. J Med Virol. 2022;94(9):4224–33. https://doi.org/10.1002/jmv.27872.
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. This work was supported by grants from Fondazione Cariplo in collaboration with Regione Lombardia and Fondazione Umberto Veronesi (CAR_RIC20GMARC_01 and CAR_RIC20GMARC_02) and by Fondazione di Comunità Milano (FON_NAZ20ADARM_01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Augello, M., Bono, V., Rovito, R. et al. Immunologic Interplay Between HIV/AIDS and COVID-19: Adding Fuel to the Flames?. Curr HIV/AIDS Rep 20, 51–75 (2023). https://doi.org/10.1007/s11904-023-00647-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-023-00647-z