Abstract
Purpose of Review
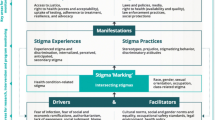
Persistent stigma remains a crucial barrier to HIV prevention and treatment services among people who use drugs (PWUD), particularly for those living with or at-risk for HIV. This scoping review examines the current state of science with regard to approaches for measuring and addressing stigma within HIV interventions among PWUD.
Recent Findings
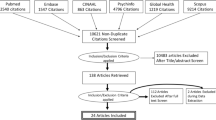
Sixteen studies fit the inclusion criteria for this review. Half the studies originated within the USA, and the remaining represented four different regions. Within these studies, stigma was measured using various quantitative, qualitative, and mixed methods. The studies primarily focused on HIV stigma, including value-based judgments, anticipated stigma, and perceived stigma domains. Information-based and skills building approaches at the individual level were the most common for the stigma reduction interventions.
Summary
Adoption of systematic evaluations is needed for measuring stigma, including intersectional stigma, within HIV interventions among PWUD. Future studies should focus on developing multilevel intersectional stigma reduction interventions for PWUD with and at-risk for HIV globally.

Similar content being viewed by others
References
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207.
Csete J, Kamarulzaman A, Kazatchkine M, Altice F, Balicki M, Buxton J, et al. Public health and international drug policy. Lancet (London, England). 2016;387(10026):1427–80.
Des Jarlais DC, Kerr T, Carrieri P, Feelemyer J, Arasteh K. HIV infection among persons who inject drugs: ending old epidemics and addressing new outbreaks. AIDS (London, England). 2016;30(6):815–26.
Centers for Disease Control and Prevention (CDC) Health Alert Network. Recent HIV clusters and outbreaks across the United States among people who inject drugs and considerations during the COVID-19 pandemic. Health Alert Network (HAN), 2020. Retrieved from https://emergency.cdc.gov/han/2020/han00436.asp. Accessed Jan 2022.
Tavitian-Exley I, Vickerman P, Bastos FI, Boily MC. Influence of different drugs on HIV risk in people who inject: systematic review and meta-analysis. Addiction (Abingdon, England). 2015;110(4):572–84.
Des Jarlais DC, Arasteh K, McKnight C, Feelemyer J, Campbell AN, Tross S, et al. What happened to the HIV epidemic among non-injecting drug users in New York City? Addiction (Abingdon, England). 2017;112(2):290–8.
O’Keefe D, Horyniak D, Dietze P. From initiating injecting drug use to regular injecting: retrospective survival analysis of injecting progression within a sample of people who inject drugs regularly. Drug Alcohol Depend. 2016;158:177–80.
Neaigus A, Miller M, Gyarmathy VA, Friedman SR. HIV heterosexual sexual risk from injecting drug users among HIV-seronegative noninjecting heroin users. Subst Use Misuse. 2011;46(2–3):208–17.
Larney S, Mathers BM, Poteat T, Kamarulzaman A, Degenhardt L. Global epidemiology of HIV among women and girls who use or inject drugs: current knowledge and limitations of existing data. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S100-9.
Goffman E. Stigma: Notes on the management of spoiled identity. New York, New York: Simon & Schuster Inc., 1986;2009.
Link BG, Phelan JC. Stigma and its public health implications. Lancet (London, England). 2006;367(9509):528–9.
Nyblade L, Mingkwan P, Stockton MA. Stigma reduction: an essential ingredient to ending AIDS by 2030. The lancet HIV. 2021;8(2):e106–13.
Mbonu NC, van den Borne B, De Vries NK. Stigma of people with HIV/AIDS in sub-Saharan Africa: a literature review. J Trop Med. 2009;2009:145891.
Rankin WW, Brennan S, Schell E, Laviwa J, Rankin SH. The stigma of being HIV-positive in Africa. PLoS Med. 2005;2(8):e247.
Boyd JE, Otilingam PG, DeForge BR. Brief version of the Internalized Stigma of Mental Illness (ISMI) scale: psychometric properties and relationship to depression, self esteem, recovery orientation, empowerment, and perceived devaluation and discrimination. Psychiatr Rehabil J. 2014;37(1):17.
Batchelder AW, Hagan MJ. The clinical relevance of a socioecological conceptualization of self-worth. Rev Gen Psychol 2022. https://doi.org/10.1177/10892680221109201
Musheke M, Ntalasha H, Gari S, McKenzie O, Bond V, Martin-Hilber A, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in sub-Saharan Africa. BMC Public Health. 2013;13:220.
Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, Mwanri L. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: a systematic review and meta-analysis. PLoS ONE. 2017;12(3):e0173928.
Calabrese SK. Understanding, contextualizing, and addressing PrEP stigma to enhance PrEP implementation. Curr HIV/AIDS Rep. 2020;17(6):579–88.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640.
Bain LE, Tarkang EE, Ebuenyi ID, Kamadjeu R. The HIV/AIDS pandemic will not end by the year 2030 in low and middle income countries. Pan Afr Med J. 2019;32:67.
Collins PH, Bilge S. Intersectionality: John Wiley & Sons; 2020.
Earnshaw VA, Smith LR, Cunningham CO, Copenhaver MM. Intersectionality of internalized HIV stigma and internalized substance use stigma: Implications for depressive symptoms. J Health Psychol. 2015;20(8):1083–9.
Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–36.
Batchelder AW, Foley JD, Kim J, Thiim A, Kelly J, Mayer K, et al. Intersecting internalized stigmas and HIV self-care among men who have sex with men and who use substances. Soc Sci Med. 1982;2021(275):113824.
Batchelder AW, Foley JD, Wirtz MR, Mayer K, O’Cleirigh C. Substance use stigma, avoidance coping, and missed hiv appointments among msm who use substances. AIDS Behav. 2021;25(5):1454–63.
Stringer KL, Marotta P, Baker E, Turan B, Kempf MC, Drentea P, et al. Substance use stigma and antiretroviral therapy adherence among a drug-using population Living with HIV. AIDS Patient Care STDS. 2019;33(6):282–93.
Richard EL, Schalkoff CA, Piscalko HM, Brook DL, Sibley AL, Lancaster KE, et al. “You are not clean until you’re not on anything“: Perceptions of medication-assisted treatment in rural Appalachia. The International journal on drug policy. 2020:102704.
Schalkoff CA, Richard EL, Piscalko HM, Sibley AL, Brook DL, Lancaster KE, et al. ”Now we are seeing the tides wash in“: Trauma and the Opioid Epidemic in Rural Appalachian Ohio. Subst Use Misuse. 2021;56(5):650–9.
Levi-Minzi MA, Surratt HL. HIV stigma among substance abusing people living with HIV/AIDS: implications for HIV treatment. AIDS Patient Care STDS. 2014;28(8):442–51.
Heads AM, Hill MJ, Suchting R, Yammine L, Gilmore-Thomas A. Predictors of anticipated PrEP stigma among women with self-reported problematic substance use: implications for engaging women in the PrEP care continuum. Arch Sex Behav. 2021;50(7):2955–64.
Basta T. HIV-related stigma and knowledge among individuals living in rural Appalachian Ohio. AIDS 2010-XVIII International AIDS Conference. Vienna, Austria, 2020.
White RH, O’Rourke A, Kilkenny ME, Schneider KE, Weir BW, Grieb SM, et al. Prevalence and correlates of receptive syringe‐sharing among people who inject drugs in rural Appalachia. Addiction (Abingdon, England) 2021;116(2):328–36.
Thomas N, van de Ven K, Mulrooney KJ. The impact of rurality on opioid-related harms: A systematic review of qualitative research. International Journal of Drug Policy. 2019:102607.
Allen ST, O’Rourke A, White RH, Smith KC, Weir B, Lucas GM, et al. Barriers and facilitators to PrEP use among people who inject drugs in rural Appalachia: a qualitative study. AIDS Behav. 2020;24(6):1942–50.
Biello KB, Bazzi AR, Mimiaga MJ, Biancarelli DL, Edeza A, Salhaney P, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm reduction journal. 2018;15(1):55.
Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18(1):919.
Sereda Y, Kiriazova T, Makarenko O, Carroll JJ, Rybak N, Chybisov A, et al. Stigma and quality of co-located care for HIV-positive people in addiction treatment in Ukraine: a cross-sectional study. Journal of the International AIDS Society. 2020;23(5):e25492-e.
English D, Rendina HJ, Parsons JT. The effects of intersecting stigma: a longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychol Violence. 2018;8(6):669–79.
Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–73.
Bowleg L, Bauer G. Invited reflection:quantifying intersectionality. Psychol Women Q. 2016;40(3):337–41.
Kulesza M, Matsuda M, Ramirez JJ, Werntz AJ, Teachman BA, Lindgren KP. Towards greater understanding of addiction stigma: intersectionality with race/ethnicity and gender. Drug Alcohol Depend. 2016;169:85–91.
Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87.
Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS education and prevention: official publication of the International Society for AIDS Education. 2003;15(1):49–69.
Mak WWS, Mo PKH, Ma GYK, Lam MYY. Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Soc Sci Med. 1982;2017(188):30–40.
Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society. 2013;16(3 Suppl 2):18734.
Bayat AH, Mohammadi R, Moradi-Joo M, Bayani A, Ahounbar E, Higgs P, et al. HIV and drug related stigma and risk-taking behaviors among people who inject drugs: a systematic review and meta-analysis. J Addict Dis. 2020;38(1):71–83.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Sallis JF, Owen N, Fisher E 2015 Ecological models of health behavior. Health behavior: Theory, research, and practice. 2015;5(43–64).
Mateu-Gelabert P, Gwadz MV, Guarino H, Sandoval M, Cleland CM, Jordan A, et al. The staying safe intervention: training people who inject drugs in strategies to avoid injection-related HCV and HIV infection. AIDS education and prevention: official publication of the International Society for AIDS Education. 2014;26(2):144–57.
Basta TB, Stambaugh T, Fisher CB. Efficacy of an educational intervention to increase consent for HIV testing in rural Appalachia. Ethics Behav. 2015;25(2):125–49.
Maskay MH, Cabral HJ, Davila JA, Whitlock Davich JA, Marcus R, Quinn EK, et al. Longitudinal stigma reduction in people living with HIV experiencing homelessness or unstable housing diagnosed with mental health or substance use disorders: an intervention study. Am J Public Health. 2018;108(S7):S546–51.
Lewis CF, Lekas HM, Rivera A, Williams SZ, Crawford ND, Pérez-Figueroa RE, et al. Pharmacy PEP access intervention among persons who use drugs in New York City: iPEPcare study-rethinking biomedical HIV prevention strategies. AIDS Behav. 2020;24(7):2101–11.
Batchelder AW, Moskowitz JT, Jain J, Cohn M, Earle MA, Carrico AW. A novel technology-enhanced internalized stigma and shame intervention for HIV-positive persons with substance use disorders. Cogn Behav Pract. 2020;27(1):55–69.
Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am J Public Health. 2002;92(3):371–7.
Broady TR, Brener L, Vuong T, Cama E, Treloar C. Online interventions to reduce stigma towards population groups affected by blood borne viruses in Australia. Int J Drug Policy. 2021;96:103292.
Go VF, Frangakis C, Le Minh N, Ha TV, Latkin CA, Sripaipan T, et al. Increased survival among HIV-infected PWID receiving a multi-level HIV risk and stigma reduction intervention: results from a randomized controlled trial. J Acquir Immune Defic Syndr. 2017;74(2):166–74.
Sugarman J, Trumble I, Hamilton E, Sarasvita R, Dumchev K, Viet H, et al. Reported participation benefits in international HIV prevention research with people who inject drugs. Ethics & human research. 2019;41(5):28–34.
Tofighi B, Isaacs N, Byrnes-Enoch H, Lakew R, Lee JD, Berry C, et al. Expanding treatment for opioid use disorder in publicly funded primary care clinics: exploratory evaluation of the NYC health + hospitals buprenorphine ECHO program. J Subst Abuse Treat. 2019;106:1–3.
Fix RL, Letourneau EJ, Mauro PM, McCart MR, Sheidow AJ. Factors promoting and impeding HIV testing among adolescents in juvenile drug court. AIDS Care. 2019;31(2):177–80.
Duby Z, Fong-Jaen F, Nkosi B, Brown B, Scheibe A. ‘We must treat them like all the other people’: evaluating the integrated key populations sensitivity training programme for healthcare workers in South Africa. South Afr J HIV Med. 2019;20(1):909.
Gichane MW, Wechsberg WM, Ndirangu J, Browne FA, Bonner CP, Grimwood A, et al. Implementation science outcomes of a gender-focused HIV and alcohol risk-reduction intervention in usual-care settings in South Africa. Drug Alcohol Depend. 2020;215:108206.
Silvia RJ. A music assignment to develop pharmacy students’ empathy toward people with opioid use disorder. Am J Pharm Educ. 2020;84(4):7631.
Burgess K, Parkhill G, Wiggins J, Ruth S, Stoovè M. Re-Wired: treatment and peer support for men who have sex with men who use methamphetamine. Sexual health. 2018;15(2):157–9.
Lunze K, Kiriazova T, Blokhina E, Bushara N, Bridden C, Gnatienko N, et al. Linking HIV-positive people in addiction care to HIV services in St Petersburg, Russia - Mixed-methods implementation study of strengths-based case management. Global public health. 2021;16(11):1711–23.
66. Lemons-Lyn A, Reidy W, Myint WW, Chan KN, Abrams E, Aung ZZ, et al. Optimizing HIV Services for Key Populations in Public-Sector Clinics in Myanmar. Journal of the International Association of Providers of AIDS Care (JIAPAC). 2021;20:23259582211055933.
Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction (Abingdon, England). 2012;107(1):39–50.
Chambers LA, Rueda S, Baker DN, Wilson MG, Deutsch R, Raeifar E, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health. 2015;15:848.
Smith LR, Earnshaw VA, Copenhaver MM, Cunningham CO. Substance use stigma: reliability and validity of a theory-based scale for substance-using populations. Drug Alcohol Depend. 2016;162:34–43.
Brown SA. Standardized measures for substance use stigma. Drug Alcohol Depend. 2011;116(1–3):137–41.
Relf MVWLH, Holt L, Nyblade L, Ellis Caiola C. A review of the state of the science of HIV and stigma: context, conceptualization, measurement, interventions, gaps, and future priorities. J Assoc Nurse in AIDS Care : JANAC. 2021;32(3):392–407.
Stevelink S, Wu IC, Voorend CG, van Brakel WH. The psychometric assessment of internalised stigma instruments: a systematic review. Stigma, Res Action. 2012;2(2):100–18.
Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet (London, England). 2010;375(9719):1014–28.
Lancaster KE, Hoffman IF, Hanscom B, Ha TV, Dumchev K, Susami H, et al. Regional differences between people who inject drugs in an HIV prevention trial integrating treatment and prevention (HPTN 074): a baseline analysis. J Int AIDS Soc. 2018;21(10):e25195.
Thanh DC, Moland KM, Fylkesnes K. Persisting stigma reduces the utilisation of HIV-related care and support services in Viet Nam. BMC Health Serv Res. 2012;12:428.
Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–73.
Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Review. 1991;43(6):1241–99.
Wakefield WD, Hudley C. African American male adolescents’ preferences in responding to racil discrimination: effects of ethnic identity and situational influences. Adolescence. 2005;40(158):237.
Karver TS, Atkins K, Fonner VA, Rodriguez-Diaz CE, Sweat MD, Taggart T, et al. HIV-related intersectional stigma and discrimination measurement: state of the science. Am J Public Health. 2022;112(S4):S420–32.
Earnshaw VA, Jonathon Rendina H, Bauer GR, Bonett S, Bowleg L, Carter J, et al. Methods in HIV-related intersectional stigma research: core elements and opportunities. Am J Public Health. 2022;112(S4):S413–9.
Hankivsky O, Reid C, Cormier R, Varcoe C, Clark N, Benoit C, et al. Exploring the promises of intersectionality for advancing women’s health research. International journal for equity in health. 2010;9:5.
Azim T, Bontell I, Strathdee SA. Women, drugs and HIV. The International journal on drug policy. 2015;26(01):S16-21.
Reback CJ, Fletcher JB. HIV prevalence, substance use, and sexual risk behaviors among transgender women recruited through outreach. AIDS Behav. 2014;18(7):1359–67.
Carter A, Min JE, Chau W, Lima VD, Kestler M, Pick N, et al. Gender inequities in quality of care among HIV-positive individuals initiating antiretroviral treatment in British Columbia, Canada (2000–2010). PLoS ONE. 2014;9(3):e92334.
Malinowska-Sempruch K. What interventions are needed for women and girls who use drugs? A global perspective. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S96–7.
Hoskin RA. Femmephobia: The role of anti-femininity and gender policing in LGBTQ+ people’s experiences of discrimination. Sex Roles. 2019;81(11):686–703.
Lancaster KE, Cooper HLF, Browning CR, Malvestutto CD, Bridges JFP, Young AM. Syringe service program utilization, barriers, and preferences for design in rural Appalachia: differences between men and women who inject drugs. Substance use & misuse. 2020:1–10.
El-Bassel N. Strathdee SA 2015 Women who use or inject drugs: an action agenda for women-specific, multilevel, and combination HIV prevention and research. J Acquired Immune Deficiency Syndromes. 1999;69(Suppl 2):S182–90.
Iversen J, Page K, Madden A, Maher L. HIV, HCV, and health-related harms among women who inject drugs: implications for prevention and treatment. J Acquir Immune Defic Syndr. 2015;69(01):S176-81.
Funding
KEL was supported by the National Institute of Drug Abuse through K01DA048174 (Lancaster, PI) and R21DA053708 (Lancaster, PI). AWB was supported by the National Institute of Drug Abuse through K23DA043418 (Batchelder, PI) and R34DA053686 (Batchelder, PI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Behavioral-Bio-Medical Interface
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lancaster, K.E., Endres-Dighe, S., Sucaldito, A.D. et al. Measuring and Addressing Stigma Within HIV Interventions for People Who Use Drugs: a Scoping Review of Recent Research. Curr HIV/AIDS Rep 19, 301–311 (2022). https://doi.org/10.1007/s11904-022-00619-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-022-00619-9