Abstract
Purpose of Review
This review presents an in-depth overview of the sleep–wake phenotype of patients with cirrhosis, together with available pharmacological and non-pharmacological treatment strategies. A set of simple, practical recommendations is also provided.
Recent Findings
The understanding of the pathophysiology of sleep disorders in this patient population has improved over the past decade, especially in relation to the interplay between homeostatic and circadian sleep regulation. In addition, new tools have been utilised for both screening and in-depth investigation of the sleep–wake profile of these patients. Finally, a number of studies have evaluated the efficacy of novel treatment strategies, often with encouraging results.
Summary
Since sleep disturbances are common in patients with cirrhosis, more so than in patients with other chronic diseases of similar severity, their assessment should become routine hepatological practice, along with the initiation of adequate treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disturbances are common in patients suffering from liver cirrhosis [1,2,3] and they impinge on their health-related quality of life (H-RQoL) [4], thus representing a challenging topic of clinical relevance.
Difficulties sleeping can be due to several factors: pain and discomfort associated with the disease, poor sleep hygiene, medications that interfere with sleep, pruritus and fatigue (especially in primary biliary cirrhosis) [5], but at the same time they are pathophysiologically related to liver disease, and they represent, at least to a certain extent, a direct consequence of liver dysfunction. Notably, insomnia is also reported in well-compensated cirrhotics, with no evident reasons for disturbed sleep such as itching, tense ascites, or treatment with diuretics [1, 4].
The recognition of sleep disturbance in cirrhosis and the understanding of its underlying pathophysiological mechanisms are of crucial importance in the management of the disease, since they may translate into potential improvement of these patients’ quality of life.
Phenotype
Sleep disturbances in cirrhosis were first characterized in 1954, when Sherlock et al. described sleep–wake inversion (i.e. the combination of restless nights and excessive daytime sleepiness) in patients with severe overt hepatic encephalopathy (HE) [3]. These features represent an extreme of the wide range of sleep disturbances exhibited by cirrhotic patients, even by those without signs of overt HE.
Few studies are available regarding the prevalence of sleep disturbance in cirrhotic patients without overt HE [1, 2, 6•, 7]. These document a prevalence of difficulties falling asleep, multiple night awakenings and daytime sleepiness varying from 27 to 70% [1, 2, 4, 6•, 7, 8].
A list of the most common sleep disorders described in patients with liver cirrhosis, divided into three groups from an aetiological point of view, follows [1,2,3,4, 6•, 9••, 10,11,12,13,14,15,16]:
-
A.
Sleep–wake signs/symptoms associated with cirrhosis:
-
prolonged sleep latency/difficulty with sleep initiation/sleep onset insomnia;
-
frequent nocturnal awakening/fragmented sleep/difficulty with sleep continuity/sleep maintenance insomnia;
-
difficulty falling asleep after nocturnal awakenings;
-
shortened sleep duration;
-
poor sleep quality/reduced ability to produce restorative sleep/unrefreshing sleep.
-
-
B.
Sleep–wake signs/symptoms secondary to the aetiology of liver disease:
-
C.
Sleep–wake signs/symptoms related to HE:
-
hypersomnia/somnolence/excessive and inappropriately timed sleepiness/numerous and long daytime naps (up to sleep–wake inversion in severe overt HE).
-
A summary of the available studies, where phenotypic characteristics of sleep disturbances in cirrhotic patients are described, is provided in Table 1.
Pathophysiology and Relation to Hepatic Encephalopathy
The origin of sleep–wake disturbances in cirrhosis is likely to be multifactorial.
It has been observed that patients with cirrhosis present delayed sleep habits/evening preference [1]. These features are, in turn, associated with impaired sleep quality. Evening type cirrhotic patients present an increased sleep latency and worse sleep quality than their counterparts with earlier sleep times [4].
Based on the assumption that sleep is regulated by two primary components, a homeostatic process, that builds up during wakefulness and declines during sleep [20], and a circadian process, with near 24-h periodicity, Montagnese et al. [9•] have proposed a model to explain the abnormal interaction between homeostatic and circadian components of sleep in cirrhotic patients.
With regard to the homeostatic sleep–wake regulation in patients with cirrhosis, it has subsequently been shown that hyperammonaemia/HE correlates with daytime sleepiness and disruption of sleep architecture. In 2012, Bersagliere et al. [21] demonstrated that the administration of a so-called amino acid challenge (AAC), a mixture of 54 g of amino acids which is used to simulate hyperammonaemia/mild HE, leads to a significant increase in daytime subjective sleepiness and changes in the sleep EEG architecture in cirrhotic patients, with a consequent impairment in their ability to generate restful sleep. These findings support the interpretation of HE as a vigilance defect [4]. Indeed, the absence of daytime sleepiness has been shown to have a high negative predictive value in relation to the occurrence of HE-related hospitalizations, thus suggesting that patients who do not report daytime sleepiness may not need formal neuropsychiatric assessment or particularly close monitoring in relation to their risk of HE [22].
Based on the hypothesis that the sleepiness-inducing effect of ammonium is mediated by adenosine, a known regulator of sleep/wake homeostasis, a recent study performed on hyperammonaemic rats (i.e. fed with an ammonium-enriched diet for 4 weeks) showed, after sleep deprivation, a larger increase in adenosine levels in hyperammonaemic animals in comparison to controls, highlighting the role of adenosine in mediating the sleepiness/sleep-inducing effects of hyperammonaemia [23••]. Interestingly, the increase in putrescine, a molecule that is presumably correlated with neuroinflammation [24] and/or blood brain barrier alterations [25], was higher in the hyperammonaemic group, pointing to a more than additive effect underlying the association between hyperammonaemia/neurocognitive impairment and insomnia.
However, there are multiple, mostly unexplored mechanisms through which cirrhosis and its complications might affect sleep–wake patterns. Further pathophysiological factors may contribute to sleep impairment, as sleep abnormalities have also been reported in patients with little or no evidence of neuropsychiatric disturbance related to HE [2] and in a number of studies no significant relationships have been observed between night sleep disturbances and the presence/degree of HE [4, 22].
Abnormalities in the circadian rhythm of melatonin of both central (reduced cerebral sensitivity to dark/light cues as a consequence of a dysfunction of the central suprachiasmatic nucleus circadian clock) and peripheral origin (reduced melatonin clearance, high daytime melatonin levels and low urinary 6-sulfatoxymelatonin concentration) may play a role, although without offering a comprehensive explanation for the observed sleep–wake disorders [11, 26].
Disturbances in the 24-h rhythm of skin temperature have been recently reported in patients with cirrhosis [27]. In physiological conditions, skin temperature starts to decrease in the evening and a redistribution of heat from core to peripheral regions, driven by vasodilatation of distal skin sites, occurs [28,29,30]. The peripheral heat loss is measured by the distal-proximal gradient (DPG), which is an excellent predictor of sleep latency [28, 29]. In patients with cirrhosis, an impaired thermoregulation, in terms of absolute values and time-course of DPG, has been reported [27]. These alterations may be explained by the hyperdynamic circulatory syndrome [31], caused by the generalized state of vasodilatation, which may hamper heat dissipation in these patients. Moreover, such abnormalities were shown to parallel the severity of the disease and the associated sleep–wake abnormalities [27].
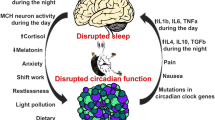
A model for the interaction and the effects of circadian and homeostatic dysfunction in cirrhosis, based on the current available evidence, is presented in Fig. 1 [20].
Cirrhosis-associated abnormalities within the context the two-process model of sleep regulation (adapted and updated from Fig. 1 of Reference 9). (a) Normal interaction between the circadian oscillation in sleep propensity and the increase in homeostatic sleep pressure during the waking hours: the greater the distance between the two curves (23:00), the higher the sleep propensity (adapted from [20]). (b) Abnormal interaction between the homeostatic regulation (black line) and the delayed circadian rhythm (red dotted line) in a patient with cirrhosis; gray line: reference circadian oscillation in the healthy population. The lack of synchrony between the two processes leads to a jet-lag East-type sleep disorder, which could contribute to the observed difficulties in commencing (increased latency) and maintaining sleep (fragmentation) (adapted from [9•]). (c) Abnormal interaction between homeostatic fluctuations (red broken line) and shifted/delayed circadian rhythm (red dotted line) in a patient with cirrhosis and HE; gray lines: reference circadian oscillation and homeostatic build-up in the healthy population. Hyperammonaemia/HE results in magnified and short-lived adenosine responses to the build-up of sleep pressure during the waking hours. This translates into an inability to generate slow-wave, restorative sleep and in a less efficient recovery from sleep deprivation.
Comorbidities
The presence of comorbid conditions should be considered in the assessment of sleep impairment in cirrhotic patients and it represents a non-negligible issue in the evaluation and proper treatment.
Obstructive Sleep Apnoea
An exemplifying condition is represented by obstructive sleep apnoea (OSA) in metabolic cirrhosis. The prevalence of this well-recognized cause of sleep fragmentation and excessive daytime somnolence [32] is increased in obese patients [33]. Emerging data support the hypothesis that OSA-related oxidative stress and hepatic ischemia-reperfusion injury may contribute to the progression from steatosis to nonalcoholic steatohepatitis (NASH) and, ultimately, metabolic cirrhosis [34,35,36,37,38].
Bajaj et al. [39] analysed the complex relationship between OSA and metabolic cirrhosis in terms of sleep quality, daytime sleepiness, cognition and driving simulation, highlighting the fact that OSA is a cause of daytime sleepiness in cirrhosis and concluding that OSA should be considered as a modulator of cognitive function and sleep quality in chronic liver disease. Moreover, Continuous Positive Airway Pressure (CPAP) has been shown to be effective in the treatment of OSA both in patients with and without cirrhosis, significantly improving executive function and sleep quality in both groups [39].
Alcohol Misuse
The negative influence of alcohol consumption on the sleep–wake cycle represents another example of the complex relationship between liver disease and its pathogenetic factors.
In recent years, a better understanding of the relationship between sleep homeostasis and genetic substrates of circadian physiology on one hand, and psychiatric disorders, including alcohol misuse, on the other, has lent support to the idea that alcohol consumption and chronobiological disruption reciprocally interact, thus resulting in a vicious cycle [40, 41]. Indeed, reciprocal interactions occur between the circadian system and ethanol consumption at both physiological and genetic levels [42]. Studies on animal models suggest that mutations of circadian clock genes (e.g. Per2 and CLOCK), are associated with increased alcohol intake, which in turn is promoted by perturbed circadian behaviour [43].
In addition, the adverse effects of alcohol consumption on sleep are well characterised both in healthy individuals and alcohol misusers. In social drinkers, acute alcohol intake determines a reduced sleep onset latency and an increased quality (delta power) and quantity of NREM sleep [44, 45], whereas severe insomnia, excessive daytime sleepiness, and altered sleep architecture are the consequences of prolonged alcohol misuse [46, 47]. Abstinence from alcohol in alcohol misusers results in severe and protracted sleep disruption, with insomnia, sleep fragmentation, and alterations in sleep architecture, that may persist for several years after withdrawal. Furthermore, sleep impairment is a predictive factor of relapse [45].
Therefore, it is reasonable to hypothesize that circadian deregulation (i.e. delayed sleep habits, irregular life-style, lack of sleep-wake, food intake and physical activity routines) may promote alcohol misuse, which in turn disrupts sleep and alters circadian rhythms.
Primary Biliary Cirrhosis
Sleep disorders complained by patients with primary biliary cirrhosis (PBC), a chronic autoimmune cholestatic disorder, may be partially explained by symptoms of liver disease, notably fatigue and pruritus [48, 49].
A significant correlation has been observed between the severity of pruritus and sleep impairment. PBC patients who show the greatest perception of pruritus and significantly complain about itching present longer sleep latency and earlier wake-up times, when compared to patients who are not considerably troubled by this symptom [5].
Similarly, fatigue negatively influences sleep–wake habits in PBC patients as it is significantly correlated with sleepiness in the morning and early afternoon hours [5, 48].
Hepatitis C Virus Infection
It has been observed that over half of patients with chronic hepatitis C complain of chronic fatigue, depression, reduced quality of life and sleep disturbance, in particular daytime sleepiness and poor sleep quality [50, 51]. The combination of such signs and symptoms has been termed “hepatitis C virus (HCV) syndrome” [52, 53] and it includes both hepatic and extra-hepatic manifestations of the infection, which are largely independent of the stage of liver fibrosis and the genotype [54].
In a study conducted on HCV-infected patients, with the aim of characterizing sleep disturbances in this population by means of actigraphy, questionnaires and sleep diaries, patients achieved lower quality of life scores and higher scores for depression, fatigue and sleep disturbances, in particular higher nocturnal activity and worse sleep efficiency, than healthy controls. Fatigue and quality of life scores correlated with bad sleep quality and daytime sleepiness [55].
While the above serve as examples of how the aetiology of liver disease and related comorbidities may impinge on the ultimate sleep–wake profile of a patient with cirrhosis, the consideration of aetiology/comorbidities and the formal diagnosis/exclusion of concomitant sleep–wake disorders are recommended (vide infra).
Tools
Sleep health can be assessed by measuring the following parameters:
-
night sleep quality,
-
sleep–wake timing,
-
daytime sleepiness.
The evaluation of sleep–wake behaviour in patients with cirrhosis comprises a heterogeneous mix of methodologies which can be distinguished into subjective and objective/semi-quantitative.
Subjective Sleep Assessment
This is based on daily sleep diaries and questionnaires. Sleep diaries have been widely utilized for collecting patient’s habitual daily routines over time in sleep–wake research. These diaries have been commonly adapted to the population/features of the study but a comparison between studies is difficult because of the absence of standardization. Recently, a ‘Consensus Sleep Diary’ with standard indices to evaluate sleep–wake disturbances and particularly insomnia has been approved [56]. There is agreement that such tool should provide information on a set of parameters including night sleep onset latency (SOL), wakefulness after initial sleep onset (WASO), total sleep time (TST), total time spent in bed (TIB), sleep efficiency, and sleep quality or satisfaction, which reflects a subjective global appraisal of each night’s sleep [56]. Based on this approach, some authors have utilized this standardized diary for evaluating self-perception of sleep quality in patients with cirrhosis, confirming delayed sleep-wake timing and frequent night awakenings [27].
The Pittsburgh Sleep Quality Index (PSQI) is the gold standard test among self-administered tools utilized for evaluating the subjective sleep quality and sleep disturbances over the preceding month, as well as for distinguishing between ‘good’ and ‘poor’ sleepers [57]. It consists of 19 individual items grouped in seven components: sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, sleep medication, and daytime dysfunction, each component being weighted equally on a 0–3 scale. The sum of all components provides a total PSQI score (ranged between 0 and 21), where scores ≥ 5 identifies poor sleepers. The PSQI takes around 10 min to be filled in and 5 min to be scored. Depending on the severity of cirrhosis, time required to complete the test and answering properly all the items can become complicated. In these settings, using simplified and quick the questionnaires, such as the validated Sleep Timing and Sleep Quality Screening Questionnaire (STSQS) [58], becomes a more suitable option for the diagnosis of subjective sleep disturbances in this population. This questionnaire takes approximately 2 min to be completed, without extra time for scoring. STSQS collects information of sleep quality rated on a 1–9 analogue scale (1: ‘best sleep ever’, 9: ‘worst sleep ever’) providing also information about habitual sleep timing: bedtime, sleep latency, night awakenings, and wake-up/get-up time. Recently, Gencdal et al. [15] have confirmed a significant correlation between STSQS and PSQI for the diagnosis of sleep disturbances in patients with cirrhosis.
Excessive daytime somnolence is one of the manifestations of the abnormal sleep–wake rhythm in patients with cirrhosis [9•] and it is commonly evaluated by means of The Epworth Sleepiness Scale (ESS) [59]. Subjects rate their likelihood of ‘dozing off’ in eight different daytime situations: sitting and reading, watching TV, sitting inactive in a public place like a theatre or meeting, as a passenger in a car for an hour without a break, lying down to rest in the afternoon when circumstances permit, sitting and talking to someone, sitting quietly after lunch without alcohol, in a car, while stopped for a few minutes in traffic. The likelihood of ‘dozing off’ is rated from 0 (unlikely) to 3 (very likely). The higher the ESS score (range 0–24), the sleepier the subject. A score ≥ 11 is considered abnormal. The detection of a strong correlation between poor cognition and excessive daytime sleepiness [6•] highlights the importance of sleepiness evaluation in the analysis of sleep disturbances in this population.
Objective Sleep Assessment
Although the assessment of subjective sleep quality provides valuable information and it is recommended for screening purposes, these tools do not offer quantitative information about sleep architecture or sleep stages.
For in-depth studies, polysomnography (PSG) represents the gold standard diagnostic tool. This technique monitors brain electrogenesis, eye movements, skeletal muscle activity, blood oxygen levels, and heart/breathing rhythms during sleep.
A small number of PSG studies of patients with cirrhosis are available [60,61,62].
A correlation between the severity of HE on one hand and PSG patterns, the duration of sleep and its organization on the other was first identified in 1972 by Kurtz et al. [63] who analysed 18 polygraphic recordings from 15 cirrhotics in different stages of encephalopathy [63].
In more recent years, polysomnographic features and sleep aspects in cirrhotic patients have been extensively characterized, as well as the role of liver dysfunction severity [60,61,62]. Teodoro et al. [60] have showed that cirrhosis is associated with shorter sleep time, reduced sleep efficiency, increased sleep latency, increased rapid eye movement (REM) latency and reduced REM sleep [60], confirming the existence of a disturbed sleep structure in this population.
Nevertheless, PSG is an expensive and labour-intensive tool. In addition, since it initially disrupts sleep, its application normally requires an adaptation night (i.e. first night polysomnography on for the subject to get used to it, second night actual recording) to avoid the well-known ‘first-night effect’ [64]. Due to the aforementioned limitations, this technique is generally employed in the research field and currently not included in the routine assessment of sleep quality.
Actigraphy is a semi-quantitative technique that records temporal rest-activity patterns and allows the analysis of micro/macrostructure of nocturnal sleep [65]. Moreover, it is cost-effective compared to PSG, unobtrusive and can be utilized in free-living conditions. The actigraph is a wrist-watch like device that includes an accelerometer to monitor the subject’s movements. The simple assumption underlying the technique is wake = movement; sleep = lack of movement. Recorded data are analyzed with a software package to estimate sleep parameters such as total time in bed, sleep latency, real sleep time, assumed sleep, wake time after sleep onset, or number of awakenings per night. In liver units, actigraphy has been used in combination with complementary structured interviews or validated questionnaires with the idea of obtaining more detailed information about sleep–wake cycle beyond data provided by body movements, confirming poor sleep quality, prolonged sleep latency and reduced sleep efficiency in cirrhotic patients [66•, 67].
A list of the most important steps that should not be neglected in the routine assessment and management of sleep disorders in cirrhotic patients, including practical recommendations and diagnostic advice provided by the literature of the last few years, is reported below and summarized in the algorithm shown in Fig. 2.
-
Formal diagnosis/exclusion of concomitant sleep–wake disorders that may be responsible for/contribute to sleep impairment.
-
The presence of comorbidities/concomitant factors, that may contribute to sleep impairment (i.e. OSA, alcohol, pruritus in PBC, ascites), should be sought for and a proper treatment should be initiated [68].
-
Specific enquiry for sleep–wake disturbances and detailed characterization of symptoms (excessive daytime sleepiness, difficulty falling asleep, frequent nocturnal awakenings/fragmented sleep, poor sleep quality/unrestful sleep, delayed sleep habits) should be performed.
-
Sleep–wake cycle-related habits and daily routine (fixed/regular or disordered/irregular) should be assessed, recommending the adherence to a regular life-style and constant habits.
-
Meal times, amount and timing of physical activity, if any.
-
The detection of excessive daytime sleepiness should elicit the hypothesis of HE and suggest the assessment of cognitive performance and ammonaemia [22].
-
Detailed and complete pharmacological history should be collected, in order to identify medications that could be responsible for/contribute to sleep disturbance [68].
-
Specific enquiry about sleep behaviour, with detailed assessment of sleep quality, sleep timing, and daytime sleepiness should be performed with appropriate tools, i.e. daily sleep diaries and sleep quality questionnaires [58]. These include the PSQI, to assess sleep quality and sleep disturbances over the preceding month, and to differentiate ‘good’ from ‘poor sleepers’; the simplified STSQS, which provides information on both sleep quality and sleep timing, and the ESS, to evaluate excessive daytime somnolence.
Treatment
Since sleep–wake assessment is not part of routine hepatological practice and the pathophysiology of sleep disorders is not completely elucidated [9•], limited data are available on how sleep–wake disturbances should be treated in patients with cirrhosis. Here follows a summary of both non-pharmacological and pharmacological approaches that have been administered and evaluated over the last few years.
Non-pharmacological Approaches
Since cirrhotic patients often suffer from ‘pill burden’, non-pharmacological treatments have often been preferred to medication [69].
For example, exposure to bright light in the early hours of the morning and avoidance of bright light exposure in the evening are sleep and light hygiene practices that should be encouraged. Drawing parallels between delayed sleep phase syndrome (DSPS), a circadian rhythm sleep disorder characterized by considerable delays in sleep onset/wake times, effectively treated with exposure to bright light in the morning [70], and the circadian deregulation and delayed melatonin response observed in cirrhosis, appropriately timed bright light therapy has been considered as a potentially beneficial non-pharmacological approach to sleep disturbances in cirrhosis [16]. One encouraging case report described in 2011 suggests that treatment with morning light might be effective [71]: an 82-year-old cirrhotic woman with a tendency to sleep–wake inversion underwent controlled lighting administration with a wall-mounted lamp, with variable light intensity/spectrum, in order to advance her sleep–wake cycle. Light was more intense and blue enriched in the morning, whereas it became less intense and red enriched during the afternoon/evening hours. As a result, a progressive improvement of sleep–wake rhythms was recorded, with reduced daytime sleepiness and fewer night awakenings. Nevertheless, a subsequent small randomized control trial of 12 cirrhotic patients did not confirm these preliminary findings, showing no obvious beneficial effect after administration of bright light therapy in terms of sleep onset, quality, and daytime sleepiness. These results are most likely in relation to the severity of disturbance at baseline, since sleep and circadian rhythms in hospitalized, decompensated patients with cirrhosis are extremely compromised [66•].
Mindfulness-based stress reduction (MBSR) is an attractive approach, the beneficial effects of which on sleep disturbances in cirrhotic patients have recently been evaluated [72]: a 4-week dedicated mindfulness and supportive group therapy approach significantly improved depression, sleep quality and H-RQoL in a group of 20 cirrhotic patients. In particular, besides a significant reduction in Beck Depression Inventory (BDI), also PSQI and, consequently, overall H-RQoL scores were significantly improved after treatment. Moreover, this approach significantly reduced the perceived burden, improved depression, and enhanced sleep quality of the caregivers of patients with cirrhosis.
Progressive neuromuscular relaxation training, lavender warm sponge bath and footbath were shown to improve sleep-related symptoms in patients with chronic liver disease, producing a significant reduction in self-rating scales of sleep [73].
Pharmacological Treatments
Sleep disorders are often inadequately treated in cirrhosis because of the role of the liver in metabolising psychoactive medication and the fact that the therapeutic-toxic threshold of these medications is very narrow in cirrhosis [72, 74]. These patients are fairly sensitive to psychoactive medication, and the risk of precipitating severe HE when administering psychoactive drugs for sleep impairment is not negligible [9•]. For example, when an “aetiological” treatment was attempted by Spahr et al. [75] who administered the histamine H1 blocker hydroxyzine to patients with minimal HE and sleep impairment, despite an increase in sleep efficiency in treatment-group vs placebo-group, one patient developed an acute episode of HE reversible upon cessation of treatment, highlighting the need of caution when prescribing this type of drugs [75].
The impairment of melatonin metabolism observed in cirrhosis, as a result of the dysfunction of the central SCN circadian clock [26, 76], may represent an interesting field of research for future therapeutic strategies. Nevertheless, several variables need to be considered, such as overnight melatonin clearance, delays in the nocturnal rise of melatonin and in its time to peak [11, 26, 77]. Therefore, the benefits and risks of melatonin administration are worthy of specific, formal studies.
Lactulose is an effective treatment for HE. Singh et al. [78•] have recently demonstrated that improvement in HE with lactulose also leads to improvement in sleep disturbances and H-RQoL. Both sleep disorders, measured with PSQI, ESS and PSG, and H-RQoL, measured with SF-36(v2) questionnaire, have shown a significant improvement after lactulose therapy for 3 months [78•], confirming preliminary results obtained in a previous randomized controlled trial by Prasad et al. [79].
Recently, rifaximin has been shown to improve objective sleep architecture parameters on 24-h PSG, with increased REM sleep after a 28-day course of treatment, although no changes were detected in the subjective quality of sleep and sleepiness [80].
Another interesting subject of study is represented by the association of ammonia-lowering [L-ornithine-L-aspartate (LOLA)] and vigilance-enhancing medication (caffeine). A pilot study [81] conducted on six healthy volunteers and six cirrhotic patients sought to assess the effects of the administration of an amino acid challenge (AAC—see above), alone and in combination with either LOLA and caffeine. Results showed that both the administration of LOLA and caffeine could contain the post-AAC increase in capillary ammonia levels in healthy volunteers. In this group, the administration of caffeine also resulted in a reduction in subjective sleepiness, in line with previous studies [82], and in the amplitude of the EEG on several frontal/temporal-occipital sites. This was taken as evidence that the association of ammonia-lowering and vigilance-enhancing medication is worthy of further study. The timing of caffeine administration is also worthy of study in patients with cirrhosis.
Hypnotics should be used with caution, especially in decompensated patients, and chosen amongst those with negligible hepatic metabolism, short half-life, no active metabolites, and limited lipophilia, to avoid prolonged intracerebral action [9•].
A list of the available studies, evaluating specific non-pharmacological approaches or pharmacological treatments, and collective reviews, is provided in Table 2.
Future Perspectives
In conclusion, over the last few years, progress has been made in terms of both the description of the sleep–wake abnormalities associated with cirrhosis, and the understanding of their pathophysiology. However, this has not yet translated into well-defined therapeutic strategies or well-designed treatment trials.
In parallel, a phenomenal amount of progress has been made by basic chronobiologists in the understanding of the functions of the liver clock and its role, dependence and ability to dissociate from the main, cerebral circadian clock [83, 84]. Meanwhile, the circadian and sleep–wake consequences of the timing of meals [85] and physical activity [86] are being better defined.
The 2017 Nobel prize in Physiology/Medicine went to the discovery of the molecular mechanisms controlling circadian rhythms. Evidence of the health consequences of both circadian deregulation and sleep loss [87, 88] is emerging at an impressive rate. Such exciting discoveries have remarkable translational, clinical and therapeutic potential, and hepatology may represent a favourable environment in this respect. We should attempt to rise to the challenge.
Change history
23 May 2018
The article Assessment and Management of Sleep Disturbance in Cirrhosis, written by Chiara Formentin, Maria Garrido, and Sara Montagnese, was originally published electronically on the publisher’s internet portal (currently SpringerLink) on 13 February 2018 without open access.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Córdoba J, Cabrera J, Lataif L, Penev P, Zee P, Blei AT. High prevalence of sleep disturbance in cirrhosis. Hepatology. 1998;27(2):339–45. https://doi.org/10.1002/hep.510270204.
Mostacci B, Ferlisi M, Baldi Antognini A, Sama C, Morelli C, Mondini S, et al. Sleep disturbance and daytime sleepiness in patients with cirrhosis: a case control study. Neurol Sci. 2008;29(4):237–40. https://doi.org/10.1007/s10072-008-0973-7.
Sherlock S, Summerskill WH, White LP, Phear EA. Portal-systemic encephalopathy; neurological complications of liver disease. Lancet. 1954;267(6836):454–7.
Montagnese S, Middleton B, Skene DJ, Morgan MY. Night-time sleep disturbance does not correlate with neuropsychiatric impairment in patients with cirrhosis. Liver Int. 2009;29(9):1372–82. https://doi.org/10.1111/j.1478-3231.2009.02089.x.
Montagnese S, Nsemi LM, Cazzagon N, Facchini S, Costa L, Bergasa NV, et al. Sleep-wake profiles in patients with primary biliary cirrhosis. Liver Int. 2013;33(2):203–9. https://doi.org/10.1111/liv.12026.
• Samanta J, Dhiman RK, Khatri A, Thumburu KK, Grover S, Duseja A, et al. Correlation between degree and quality of sleep disturbance and the level of neuropsychiatric impairment in patients with liver cirrhosis. Metab Brain Dis. 2013;28(2):249–59. https://doi.org/10.1007/s11011-013-9393-3. This study analyses the relationship between night sleep disturbance/excessive daytime sleepiness and neuropsychiatric impairment in patients with cirrhosis.
De Cruz S, Espiritu J, Zeidler M, Wang T. Sleep disorders in chronic liver disease. Seminars in Respiratory and Critical Care Medicine. 2012;33(1):26–35. https://doi.org/10.1055/s-0032-1301732.
Bianchi G, Marchesini G, Nicolino F, Graziani R, Sgarbi D, Loguercio C, et al. Psychological status and depression in patients with liver cirrhosis. Dig Liver Dis. 2005;37(8):593–600. https://doi.org/10.1016/j.dld.2005.01.020.
• Montagnese S, De Pittà C, De Rui M, Corrias M, Turco M, Merkel C, et al. Sleep-wake abnormalities in patients with cirrhosis. Hepatology. 2014;59(2):705–12. https://doi.org/10.1002/hep.26555. This review describes the features of sleep-wake disturbances in patients with cirrhosis, their mutual relationships, and those with hepatic failure/hepatic encephalopathy, along with providing the available information on their pathophysiology.
Llansola M, Cantero JL, Hita-Yañez E, Mirones-Maldonado MJ, Piedrafita B, Ahabrach H, et al. Progressive reduction of sleep time and quality in rats with hepatic encephalopathy caused by portacaval shunts. Neuroscience. 2012;201:199–208. https://doi.org/10.1016/j.neuroscience.2011.11.009.
Steindl PE, Finn B, Bendok B, Rothke S, Zee PC, Blei AT. Disruption of the diurnal rhythm of plasma melatonin in cirrhosis. Ann Intern Med. 1995;123(4):274–7. https://doi.org/10.7326/0003-4819-123-4-199508150-00005.
Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. https://doi.org/10.1053/smrv.2002.0186.
AL-Jahdali H, Al Enezi A, Anwar AE, AL-Harbi A, Baharoon S, Aljumah A, et al. Prevalence of insomnia and sleep patterns among liver cirrhosis patients. J Circadian Rhythms. 2014;12(1):2. https://doi.org/10.5334/jcr.aa.
Moore C. Evaluation and management of insomnia, muscle cramps, fatigue, and itching in cirrhotic patients. Clin Liver Dis. 2016;7(1):5–7. https://doi.org/10.1002/cld.516.
Gencdal G, Gunsar F, Meral CE, Salman E, Gürsel B, Oruç N, et al. Sleep disorders in cirrhotics; how can we detect ? Liver Int. 2014;34(8):1192–7. https://doi.org/10.1111/liv.12485.
Montagnese S, Middleton B, Mani AR, Skene DJ, Morgan MY. Sleep and circadian abnormalities in patients with cirrhosis: features of delayed sleep phase syndrome? Metab Brain Dis. 2009;24(3):427–39. https://doi.org/10.1007/s11011-009-9146-5.
Prat G, Adan A. Influence of circadian typology on drug consumption, hazardous alcohol use, and hangover symptoms. Chronobiol Int. 2011;28(3):248–57. https://doi.org/10.3109/07420528.2011.553018.
Wittmann M, Paulus M, Roenneberg T. Decreased psychological well-being in late ‘chronotypes’ is mediated by smoking and alcohol consumption. Substance Use & Misuse. 2010;45(1–2):15–30. https://doi.org/10.3109/10826080903498952.
Smolensky MH, Hermida RC, Reinberg A, Sackett-Lundeen L, Portaluppi F. Circadian disruption: new clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol Int. 2016;33(8):1101–19. https://doi.org/10.1080/07420528.2016.1184678.
Borbély AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1(3):195–204.
Bersagliere A, Raduazzo ID, Nardi M, Schiff S, Gatta A, Amodio P, et al. Induced hyperammonemia may compromise the ability to generate restful sleep in patients with cirrhosis. Hepatology. 2012;55(3):869–78. https://doi.org/10.1002/hep.24741.
De Rui M, Schiff S, Aprile D, Angeli P, Bombonato G, Bolognesi M, et al. Excessive daytime sleepiness and hepatic encephalopathy: it is worth asking. Metab Brain Dis. 2013;28(2):245–8. https://doi.org/10.1007/s11011-012-9360-4.
•• Marini S, Santangeli O, Saarelainen P, Middleton B, Chowdhury N, Skene DJ, et al. Abnormalities in the polysomnographic, adenosine and metabolic response to sleep deprivation in an animal model of hyperammonemia. Front Physiol. 2017;8:636. https://doi.org/10.3389/fphys.2017.00636. The role of hyperammonemia in modulating adenosine/metabolite/EEG response to sleep deprivation and its influence on homeostatic sleep regulation is elucidated.
Rodrigo R, Cauli O, Gomez–Pinedo U, Agusti A, Hernandez-Rabaza V, Garcia-Verdugo J, et al. Hyperammonemia induces neuroinflammation that contributes to cognitive impairment in rats with hepatic encephalopathy. Gastroenterology. 2010;139(2):675–84. https://doi.org/10.1053/j.gastro.2010.03.040.
Skowrońska M, Albrecht J. Alterations of blood brain barrier function in hyperammonemia: an overview. Neurotox Res. 2012;21(2):236–44. https://doi.org/10.1007/s12640-011-9269-4.
Montagnese S, Middleton B, Mani AR, Skene DJ, Morgan MY. On the origin and the consequences of circadian abnormalities in patients with cirrhosis. Am J Gastroenterol. 2010;105(8):1773–81. https://doi.org/10.1038/ajg.2010.86.
Garrido M, Saccardo D, De Rui M, Vettore E, Verardo A, Carraro P, et al. Abnormalities in the 24-hour rhythm of skin temperature in cirrhosis: sleep-wake and general clinical implications. Liver Int. 2017;37(12):1833–42. https://doi.org/10.1111/liv.13525.
Kräuchi K, Cajochen C, Werth E, Wirz-Justice A. Functional link between distal vasodilation and sleep-onset latency? Am J Physiol. Regul, Integr Comp Physiol. 2000;278(3):R741–8. https://doi.org/10.1152/ajpregu.2000.278.3.R741.
Kräuchi K, Cajochen C, Werth E, Wirz-Justice A. Warm feet promote the rapid onset of sleep. Nature. 1999;401(6748):36–7. https://doi.org/10.1038/43366.
Raymann RJEM, Swaab DF, Van Someren EJW. Cutaneous warming promotes sleep onset. Am J Physiol Regul, Integr Comp Physiol. 2005;288(6):R1589–97. https://doi.org/10.1152/ajpregu.00492.2004.
Bolognesi M, Di Pascoli M, Verardo A, Gatta A. Splanchnic vasodilation and hyperdynamic circulatory syndrome in cirrhosis. World J Gastroenterol. 2014;20(10):2555–63. https://doi.org/10.3748/wjg.v20.i10.2555.
Simon S, Collop N. Latest advances in sleep medicine. Chest. 2012;142(6):1645–51. https://doi.org/10.1378/chest.12-2391.
Musso G, Cassader M, Olivetti C, Rosina F, Carbone G, Gambino R. Association of obstructive sleep apnoea with the presence and severity of non-alcoholic fatty liver disease. A systematic review and meta-analysis. Obes Rev. 2013;14(5):417–31. https://doi.org/10.1111/obr.12020.
Day CP. From fat to inflammation. Gastroenterology. 2006;130(1):207–10. https://doi.org/10.1053/j.gastro.2005.11.017.
Mishra P, Nugent C, Afendy A, Bai C, Bhatia P, Afendy M, et al. Apnoeic-hypopnoeic episodes during obstructive sleep apnoea are associated with histological nonalcoholic steatohepatitis. Liver Int. 2008;28(8):1080–6. https://doi.org/10.1111/j.1478-3231.2008.01822.x.
Savransky V, Nanayakkara A, Vivero A, Li J, Bevans S, Smith PL, et al. Chronic intermittent hypoxia predisposes to liver injury. Hepatology. 2007;45(4):1007–13. https://doi.org/10.1002/hep.21593.
Li J, Grigoryev DN, Ye SQ, Thorne L, Schwartz AR, Smith PL, et al. Chronic intermittent hypoxia upregulates genes of lipid biosynthesis in obese mice. J Appl Physiol. 2005;99(5):1643–8. https://doi.org/10.1152/japplphysiol.00522.2005.
Drager LF, Li J, Reinke C, Bevans-Fonti S, Jun JC, Polotsky VY. Intermittent hypoxia exacerbates metabolic effects of diet-induced obesity. Obesity. 2011;19(11):2167–74. https://doi.org/10.1038/oby.2011.240.
Bajaj JS, Thacker LR, Leszczyszyn D, Taylor SA, Heuman DM, Raman S, et al. Effects of obstructive sleep apnea on sleep quality, cognition, and driving performance in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13(2):390–397.e1. https://doi.org/10.1016/j.cgh.2014.08.028.
Landgraf D, McCarthy MJ, Welsh DK. Circadian clock and stress interactions in the molecular biology of psychiatric disorders. Curr Psychiatr Rep. 2014;16(10):483. https://doi.org/10.1007/s11920-014-0483-7.
Rosenwasser AM. Circadian clock genes: non-circadian roles in sleep, addiction, and psychiatric disorders? Neurosci Biobehav Rev. 2010;34(8):1249–55. https://doi.org/10.1016/j.neubiorev.2010.03.004.
Rosenwasser AM. Chronobiology of ethanol: animal models. Alcohol. 2015;49(4):311–9. https://doi.org/10.1016/j.alcohol.2015.04.001.
Prosser RA, Glass JD. Assessing ethanol’s actions in the suprachiasmatic circadian clock using in vivo and in vitro approaches. Alcohol. 2015;49(4):321–39. https://doi.org/10.1016/j.alcohol.2014.07.016.
Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: effects on normal sleep. Alcohol Clin Exp Res. 2013;37(4):539–49. https://doi.org/10.1111/acer.12006.
Thakkar MM, Sharma R, Sahota P. Alcohol disrupts sleep homeostasis. Alcohol. 2015;49(4):299–310. https://doi.org/10.1016/j.alcohol.2014.07.019.
Brower KJ, Perron BE. Sleep disturbance as a universal risk factor for relapse in addictions to psychoactive substances. Med Hypotheses. 2010;74(5):928–33. https://doi.org/10.1016/j.mehy.2009.10.020.
Colrain IM, Turlington S, Baker FC. Impact of alcoholism on sleep architecture and EEG power spectra in men and women. Sleep. 2009;32(10):1341–52. https://doi.org/10.1093/sleep/32.10.1341.
Cauch-Dudek K, Abbey S, Stewart DE. Heathcote EJ. Fatigue in primary biliary cirrhosis. Gut BMJ Publishing Group. 1998;43(5):705–10.
Newton JL, Gibson GJ, Tomlinson M, Wilton K, Jones D. Fatigue in primary biliary cirrhosis is associated with excessive daytime somnolence. Hepatology. 2006;44(1):91–8. https://doi.org/10.1002/hep.21230.
Sockalingam S, Abbey SE, Alosaimi F, Novak M. A review of sleep disturbance in hepatitis C. J Clin Gastroenterol. 2010;44(1):38–45. https://doi.org/10.1097/MCG.0b013e3181b314ea.
Carlson MD, Hilsabeck RC, Barakat F, Perry W. Role of sleep disturbance in chronic hepatitis C infection. Current Hepatitis Reports. 2010;9(1):25–9. https://doi.org/10.1007/s11901-010-0030-x.
Zignego AL, Ferri C, Pileri SA, Caini P, Bianchi FB, Italian Association of the Study of Liver Commission on Extrahepatic Manifestations of HCV infection. Extrahepatic manifestations of hepatitis C virus infection: a general overview and guidelines for a clinical approach. Dig Liver Dis. 2007;39(1):2–17. https://doi.org/10.1016/j.dld.2006.06.008.
Ferri C, Antonelli A, Mascia MT, Sebastiani M, Fallahi P, Ferrari D, et al. HCV-related autoimmune and neoplastic disorders: the HCV syndrome. Dig Liver Dis. 2007;39:S13–21. https://doi.org/10.1016/S1590-8658(07)80005-3.
Monaco S, Mariotto S, Ferrari S, Calabrese M, Zanusso G, Gajofatto A, et al. Hepatitis C virus-associated neurocognitive and neuropsychiatric disorders: advances in 2015. World J Gastroenterol. 2015;21(42):11974–83. https://doi.org/10.3748/wjg.v21.i42.11974.
Heeren M, Sojref F, Schuppner R, Worthmann H, Pflugrad H, Tryc AB, et al. Active at night, sleepy all day—sleep disturbances in patients with hepatitis C virus infection. J Hepatol. 2014;60(4):732–40. https://doi.org/10.1016/j.jhep.2013.11.030.
Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302. https://doi.org/10.5665/sleep.1642.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Montagnese S, Middleton B, Skene DJ, Morgan MY. Sleep-wake patterns in patients with cirrhosis: all you need to know on a single sheet. A simple sleep questionnaire for clinical use. J Hepatol. 2009;51(4):690–5. https://doi.org/10.1016/j.jhep.2009.06.006.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5. https://doi.org/10.1093/sleep/14.6.540.
Teodoro VV, Júnior MAB, Lucchesi LM, Cavignolli D, de Mello MT, Kondo M, et al. Polysomnographic sleep aspects in liver cirrhosis: a case control study. World J Gastroenterol. 2013;19(22):3433–8. https://doi.org/10.3748/wjg.v19.i22.3433.
Martino ME, Fernández-Lorente J, Romero-Vives M, Bárcena R, Gaztelu JM. Brain oscillatory activity during sleep shows unknown dysfunctions in early encephalopathy. J Physiol Biochem. 2014;70(3):821–35. https://doi.org/10.1007/s13105-014-0351-2.
Saleh K, Javaheri S. Sleep in ambulatory patients with stable cirrhosis of the liver. Sleep Medicine Elsevier. 2017;41:15–9. https://doi.org/10.1016/J.SLEEP.2017.08.022.
Kurtz D, Zenglein JP, Imler M, Girardel M, Grinspan G, Peter B, et al. Night sleep in porto-caval encephalopathy. Electroencephalogr Clin Neurophysiol. 1972;33(2):167–78.
Lee D-H, Cho C-H, Han C, Bok K-N, Moon JH, Lee E, et al. Sleep irregularity in the previous week influences the first-night effect in polysomnographic studies. Psychiatry Investigation. 2016;13(2):203–9. https://doi.org/10.4306/pi.2016.13.2.203.
Winnebeck EC, Fischer D, Leise T, Roenneberg T. Dynamics and ultradian structure of human sleep in real life. Curr Biol : CB. 2017;28(1):49–59.e5. https://doi.org/10.1016/j.cub.2017.11.063.
• De Rui M, Middleton B, Sticca A, Gatta A, Amodio P, Skene DJ, et al. Sleep and circadian rhythms in hospitalized patients with decompensated cirrhosis: effect of light therapy. Neurochem Res. 2015;40(2):284–92. https://doi.org/10.1007/s11064-014-1414-z. This study describes an attempt to treat sleep disturbances in hospitalized cirrhotic patients with bright light therapy, although with limited beneficial effects, most likely in relation to the severity of liver failure/sleep disturbance at baseline.
Ghabril M, Jackson M, Gotur R, Weber R, Orman E, Vuppalanchi R, et al. Most individuals with advanced cirrhosis have sleep disturbances, which are associated with poor quality of life. Clin Gastroenterol Hepatol. 2017;15(8):1271–8. https://doi.org/10.1016/j.cgh.2017.01.027.
Newton JL, Jones DEJ. Managing systemic symptoms in chronic liver disease. J Hepatol. 2012;56:S46–55. https://doi.org/10.1016/S0168-8278(12)60006-3.
Zhao X, Wong P. Managing sleep disturbances in cirrhosis. Scientifica. 2016;2016:6576812. https://doi.org/10.1155/2016/6576812.
Weyerbrock A, Timmer J, Hohagen F, Berger M, Bauer J. Effects of light and chronotherapy on human circadian rhythms in delayed sleep phase syndrome: cytokines, cortisol, growth hormone, and the sleep-wake cycle. Biol Psychiatry. 1996;40(8):794–7. https://doi.org/10.1016/0006-3223(95)00661-3.
De Rui M, Gaiani S, Middleton B, Skene DJ, Schiff S, Gatta A, et al. Bright times for patients with cirrhosis and delayed sleep habits: a case report on the beneficial effect of light therapy. Am J Gastroenterol. 2011;106(11):2048–9. https://doi.org/10.1038/ajg.2011.239.
Bajaj JS, Ellwood M, Ainger T, Burroughs T, Fagan A, Gavis EA, et al. Mindfulness-based stress reduction therapy improves patient and caregiver-reported outcomes in cirrhosis. Clin Transl Gastroenterol. 2017;8(7):e108. https://doi.org/10.1038/ctg.2017.38.
Liu C, Xie H, Zhang X, Yu Y, Zhang X, Sun Y, et al. Health related management plans improve sleep disorders of patients with chronic liver disease. Int J Clin Exp Med. 2015;8(6):9883–9.
Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis—a practical guide. Aliment Pharmacol Ther. 2013;37(12):1132–56. https://doi.org/10.1111/apt.12324.
Spahr L, Coeytaux A, Giostra E, Hadengue A, Annoni J-M. Histamine H1 blocker hydroxyzine improves sleep in patients with cirrhosis and minimal hepatic encephalopathy: a randomized controlled pilot trial. Am J Gastroenterol. 2007;102(4):744–53. https://doi.org/10.1111/j.1572-0241.2006.01028.x.
Montagnese S, Middleton B, Mani AR, Skene DJ, Morgan MY. Changes in the 24-h plasma cortisol rhythm in patients with cirrhosis. J Hepatol. 2011;54(3):588–90. https://doi.org/10.1016/j.jhep.2010.08.015.
Velissaris D, Karanikolas M, Kalogeropoulos A, Solomou E, Polychronopoulos P, Thomopoulos K, et al. Pituitary hormone circadian rhythm alterations in cirrhosis patients with subclinical hepatic encephalopathy. World J Gastroenterol. 2008;14(26):4190–5. https://doi.org/10.3748/wjg.14.4190.
• Singh J, Sharma BC, Puri V, Sachdeva S, Srivastava S. Sleep disturbances in patients of liver cirrhosis with minimal hepatic encephalopathy before and after lactulose therapy. Metab Brain Dis. 2017;32(2):595–605. https://doi.org/10.1007/s11011-016-9944-5. This studies shows the efficacy of lactulose for improve hepatic encephalopathy, sleep disturbances and H-RQoL.
Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology. 2007;45(3):549–59. https://doi.org/10.1002/hep.21533.
Bruyneel M, Sersté T, Libert W, van den Broecke S, Ameye L, Dachy B, et al. Improvement of sleep architecture parameters in cirrhotic patients with recurrent hepatic encephalopathy with the use of rifaximin. Eur J Gastroenterol Hepatol. 2017;29(3):302–8. https://doi.org/10.1097/MEG.0000000000000786.
Garrido M, Skorucak J, Raduazzo D, Turco M, Spinelli G, Angeli P, et al. Vigilance and wake EEG architecture in simulated hyperammonaemia: a pilot study on the effects of L-Ornithine-L-Aspartate (LOLA) and caffeine. Metab Brain Dis. 2016;31(4):965–74. https://doi.org/10.1007/s11011-016-9835-9.
Casula EP, Bisiacchi PS, Corrias M, Schiff S, Merkel C, Amodio P, et al. Acute hyperammonaemia induces a sustained decrease in vigilance, which is modulated by caffeine. Metab Brain Dis. 2015;30(1):143–9. https://doi.org/10.1007/s11011-014-9590-8.
Asher G, Reinke H, Altmeyer M, Gutierrez-Arcelus M, Hottiger MO, Schibler U. Poly(ADP-ribose) polymerase 1 participates in the phase entrainment of circadian clocks to feeding. Cell. 2010;142(6):943–53. https://doi.org/10.1016/j.cell.2010.08.016.
Ikeda Y, Sasaki H, Ohtsu T, Shiraishi T, Tahara Y, Shibata S. Feeding and adrenal entrainment stimuli are both necessary for normal circadian oscillation of peripheral clocks in mice housed under different photoperiods. Chronobiol Int. 2015;32(2):195–210. https://doi.org/10.3109/07420528.2014.962655.
Wehrens SMT, Christou S, Isherwood C, Middleton B, Gibbs MA, Archer SN, et al. Meal timing regulates the human circadian system. Curr Biol. 2017;27(12):1768–1775.e3. https://doi.org/10.1016/j.cub.2017.04.059.
Buxton OM, Frank SA, L’Hermite-Balériaux M, Leproult R, Turek FW, Van Cauter E. Roles of intensity and duration of nocturnal exercise in causing phase delays of human circadian rhythms. Am J Phys. 1997;273:E536–42.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–43. https://doi.org/10.1016/j.cub.2012.03.038.
Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, et al. Association between rotating night shift work and risk of coronary heart disease among women. JAMA. 2016;315(16):1726–34. https://doi.org/10.1001/jama.2016.4454.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Chiara Formentin, Maria Garrido, and Sara Montagnese each declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
The original version of this article was revised due to a retrospective Open Access order.
This article is part of the Topical Collection on Management of Cirrhotic Patient
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Formentin, C., Garrido, M. & Montagnese, S. Assessment and Management of Sleep Disturbance in Cirrhosis. Curr Hepatology Rep 17, 52–69 (2018). https://doi.org/10.1007/s11901-018-0390-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-018-0390-1