Abstract
Purpose of Review
The treatment of Waldenström macroglobulinemia (WM) has evolved over the past decade. With the seminal discoveries of MYD88 and CXCR warts, hypogammaglobulinemia, infections, and myelokathexis (WHIM) mutations in WM cells, our understanding of the disease biology and treatment has improved. The development of a new class of agents, Bruton tyrosine kinase inhibitors (BTKi), has substantially impacted the treatment paradigm of WM. Herein, we review the current and emerging BTKi and the evidence for their use in WM.
Recent Findings
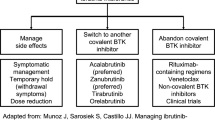
Clinical trials have established the role of covalent BTKi in the treatment of WM. Their efficacy is compromised among patients who harbor CXCR4WHIM mutation or MYD88WT genotype. The development of BTKC481 mutation-mediated resistance to covalent BTKi may lead to disease refractoriness. Novel, non-covalent, next-generation BTKi are emerging, and preliminary results of the early phase clinical trials show promising activity in WM, even among patients refractory to a covalent BTKi.
Summary
Covalent BTK inhibitors have demonstrated meaningful outcomes in treatment-naïve (TN) and relapsed refractory (R/R) WM, particularly among those harboring the MYD88L265P mutation. The next-generation BTKi demonstrate improved selectivity, resulting in a more favorable toxicity profile. In WM, BTKi are administered until progression or the development of intolerable toxicity. Consequently, the potential for acquired resistance, the emergence of cumulative toxicities, and treatment-related financial burden are critical challenges associated with the continuous therapy approach. By circumventing BTK C481 mutations that alter the binding site to covalent BTKi, the non-covalent BTKi serve as alternative agents in the event of acquired resistance. Head-to-head comparative trials with the conventional chemoimmunotherapies are lacking. The findings of the RAINBOW trial (NCT046152), comparing the dexamethasone, rituximab, and cyclophosphamide (DRC) regimen to the first-generation, ibrutinib are awaited, but more studies are needed to draw definitive conclusions on the comparative efficacy of chemoimmunotherapy and BTKi. Complete response is elusive with BTKi, and combination regimens to improve upon the efficacy and limit the treatment duration are also under evaluation in WM.
Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study. P.K is the principal investigator of trials for which Mayo Clinic has received research funding from Amgen, Regeneron, Bristol Myers Squibb, Loxo Pharmaceuticals, Ichnos, Karyopharm, Sanofi, AbbVie and GlaxoSmithKline. Prashant Kapoor has served on the Advisory Boards of BeiGene, Mustang Bio, Pharmacyclics, X4 Pharmaceuticals, AstraZeneca, Kite, Oncopeptides, Angitia Bio, GlaxoSmithKline, AbbVie and Sanofi.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ghobrial IM, Gertz MA, Fonseca R. Waldenström macroglobulinaemia. Lancet Oncol. 2003;4(11):679–85.
Fonseca R, Hayman S. Waldenström macroglobulinaemia. Br J Haematol. 2007;138(6):700–20.
Kyle RA, et al. Fifty-year incidence of Waldenström Macroglobulinemia in Olmsted County, Minnesota, from 1961 through 2010: a population-based study with complete case capture and hematopathologic review. Mayo Clin Proc. 2018;93(6):739–46.
Yin X, et al. Trends in incidence and mortality of Waldenström Macroglobulinemia: a population-based study. Front Oncol. 2020;10:1712.
Castillo JJ, Ghobrial IM, Treon SP. Biology, prognosis, and therapy of waldenström macroglobulinemia. Cancer Treat Res 2015;165:177–195.
Treon SP, et al. MYD88 L265P somatic mutation in Waldenström’s macroglobulinemia. N Engl J Med. 2012;367(9):826–33.
Lin SC, Lo YC, Wu H. Helical assembly in the MyD88-IRAK4-IRAK2 complex in TLR/IL-1R signalling. Nature. 2010;465(7300):885–90.
Varettoni M, et al. Prevalence and clinical significance of the MYD88 (L265P) somatic mutation in Waldenstrom’s macroglobulinemia and related lymphoid neoplasms. Blood. 2013;121(13):2522–8.
Yang G, et al. A mutation in MYD88 (L265P) supports the survival of lymphoplasmacytic cells by activation of Bruton tyrosine kinase in Waldenström macroglobulinemia. Blood. 2013;122(7):1222–32.
Hunter ZR, et al. The genomic landscape of Waldenstrom macroglobulinemia is characterized by highly recurring MYD88 and WHIM-like CXCR4 mutations, and small somatic deletions associated with B-cell lymphomagenesis. Blood. 2014;123(11):1637–46.
Kaiser LM, et al. CXCR4 in Waldenström’s Macroglobulinema: chances and challenges. Leukemia. 2021;35(2):333–45.
Gustine JN, et al. CXCR4 (S338X) clonality is an important determinant of ibrutinib outcomes in patients with Waldenstrom macroglobulinemia. Blood Adv. 2019;3(19):2800–3.
Treon SP, et al. Somatic mutations in MYD88 and CXCR4 are determinants of clinical presentation and overall survival in Waldenstrom macroglobulinemia. Blood. 2014;123(18):2791–6.
Varettoni M, et al. Pattern of somatic mutations in patients with Waldenström macroglobulinemia or IgM monoclonal gammopathy of undetermined significance. Haematologica. 2017;102(12):2077–85.
Castillo JJ, et al. Recommendations for the diagnosis and initial evaluation of patients with Waldenström Macroglobulinaemia: a Task Force from the 8th International Workshop on Waldenström Macroglobulinaemia. Br J Haematol. 2016;175(1):77–86.
Kastritis E, et al. Waldenström's macroglobulinaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018; 29(Suppl 4): iv41-iv50.
Kyle RA, et al. Prognostic markers and criteria to initiate therapy in Waldenstrom’s macroglobulinemia: consensus panel recommendations from the Second International Workshop on Waldenstrom’s Macroglobulinemia. Semin Oncol. 2003;30(2):116–20.
Kapoor P, et al. Diagnosis and Management of Waldenström Macroglobulinemia: Mayo Stratification of Macroglobulinemia and Risk-Adapted Therapy (mSMART) Guidelines 2016. JAMA Oncol. 2017;3(9):1257–65.
Owen RG, et al. Clinicopathological definition of Waldenstrom’s macroglobulinemia: consensus panel recommendations from the Second International Workshop on Waldenstrom’s Macroglobulinemia. Semin Oncol. 2003;30(2):110–5.
Pophali PA, et al. Prevalence and survival of smouldering Waldenström macroglobulinaemia in the United States. Br J Haematol. 2019;184(6):1014–7.
Kyle RA, et al. Progression in smoldering Waldenstrom macroglobulinemia: long-term results. Blood. 2012;119(19):4462–6.
Bustoros M, et al. Progression risk stratification of asymptomatic Waldenström macroglobulinemia. J Clin Oncol. 2019;37(16):1403–11.
Alexanian R, et al. Asymptomatic Waldenstrom’s macroglobulinemia. Semin Oncol. 2003;30(2):206–10.
Baldini L, et al. Immunoglobulin M monoclonal gammopathies of undetermined significance and indolent Waldenstrom’s macroglobulinemia recognize the same determinants of evolution into symptomatic lymphoid disorders: proposal for a common prognostic scoring system. J Clin Oncol. 2005;23(21):4662–8.
• Zanwar S, et al. Disease outcomes and biomarkers of progression in smouldering Waldenström macroglobulinaemia. Br J Haematol. 2021;195(2): 210–216. A retrospective study that identified biomarkers (hemoglobin ≤123 g/L and β2-microglobulin ≥2.7 µg/mL) in patients with smouldering Waldenström macroglobulinaemia (SWM) that predict a shorter time to progression to active WM. The study also revealed comparable survival of SWM and a matched USA population.
Morel P, et al. International prognostic scoring system for Waldenstrom macroglobulinemia. Blood. 2009;113(18):4163–70.
Zanwar S, et al. Modified staging system for Waldenström Macroglobulinemia (MSS-WM): a multi-institutional externally validated prognostic model for active/symptomatic Waldenström Macroglobulinemia. Blood. 2023;142(Supplement 1):3030–3030.
Kastritis E, et al. A revised international prognostic score system for Waldenström’s macroglobulinemia. Leukemia. 2019;33(11):2654–61.
Gertz MA. Waldenström macroglobulinemia: 2021 update on diagnosis, risk stratification, and management. Am J Hematol. 2021;96(2):258–69.
Rummel MJ, et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet. 2013;381(9873):1203–10.
Dimopoulos MA, et al. Primary treatment of Waldenström macroglobulinemia with dexamethasone, rituximab, and cyclophosphamide. J Clin Oncol. 2007;25(22):3344–9.
Paludo J, et al. Dexamethasone, rituximab and cyclophosphamide for relapsed and/or refractory and treatment-naïve patients with Waldenstrom macroglobulinemia. Br J Haematol. 2017;179(1):98–105.
Paludo J, et al. Bendamustine and rituximab (BR) versus dexamethasone, rituximab, and cyclophosphamide (DRC) in patients with Waldenström macroglobulinemia. Ann Hematol. 2018;97(8):1417–25.
Treon SP, et al. Primary therapy of Waldenström macroglobulinemia with bortezomib, dexamethasone, and rituximab: WMCTG clinical trial 05–180. J Clin Oncol. 2009;27(23):3830–5.
Ghobrial IM, et al. Phase II trial of weekly bortezomib in combination with rituximab in relapsed or relapsed and refractory Waldenstrom macroglobulinemia. J Clin Oncol. 2010;28(8):1422–8.
Dimopoulos MA, et al. Primary therapy of Waldenström macroglobulinemia (WM) with weekly bortezomib, low-dose dexamethasone, and rituximab (BDR): long-term results of a phase 2 study of the European Myeloma Network (EMN). Blood. 2013;122(19):3276–82.
Treon SP, et al. Carfilzomib, rituximab, and dexamethasone (CaRD) treatment offers a neuropathy-sparing approach for treating Waldenström’s macroglobulinemia. Blood. 2014;124(4):503–10.
Castillo JJ, et al. Prospective clinical trial of ixazomib, dexamethasone, and rituximab as primary therapy in Waldenström macroglobulinemia. Clin Cancer Res. 2018;24(14):3247–52.
Castillo JJ, et al. Ixazomib, dexamethasone, and rituximab in treatment-naive patients with Waldenström macroglobulinemia: long-term follow-up. Blood Adv. 2020;4(16):3952–9.
Burger JA. Bruton tyrosine kinase inhibitors: present and future. Cancer J. 2019;25(6):386–93.
Stevenson FK, et al. B-cell receptor signaling in chronic lymphocytic leukemia. Blood. 2011;118(16):4313–20.
Satterthwaite AB, Witte ON. The role of Bruton’s tyrosine kinase in B-cell development and function: a genetic perspective. Immunol Rev. 2000;175:120–7.
Pals ST, Kersten MJ, Spaargaren M. Targeting cell adhesion and homing as strategy to cure Waldenstrom’s macroglobulinemia. Best Pract Res Clin Haematol. 2016;29(2):161–8.
Castillo JJ, et al. Consensus treatment recommendations from the tenth International Workshop for Waldenström Macroglobulinaemia. Lancet Haematol. 2020;7(11):e827–37.
Davids MS, Brown JR. Ibrutinib: a first in class covalent inhibitor of Bruton’s tyrosine kinase. Future Oncol (Lond, Engl). 2014;10(6):957–67.
Pharmacyclics, I. ImbruvicaTM (ibrutinib) capsules for oral use; US prescribing information. 2013.
Abeykoon JP, Yanamandra U, Kapoor P. New developments in the management of Waldenström macroglobulinemia. Cancer Manag Res. 2017;9:73–83.
Mason C, et al. Ibrutinib penetrates the blood brain barrier and shows efficacy in the therapy of Bing Neel syndrome. Br J Haematol. 2017;179(2):339–41.
•• Castillo JJ, et al. Ibrutinib for the treatment of Bing-Neel syndrome: a multicenter study. Blood. 2019;133(4):299-305. A retrospective, multicenter study that demonstrated a favorable response with ibrutinib therapy in patients with Bing-Neal syndrome.
Treon SP, et al. Ibrutinib in previously treated Waldenstrom’s macroglobulinemia. N Engl J Med. 2015;372(15):1430–40.
Treon SP, et al. Ibrutinib monotherapy in symptomatic, treatment-naïve patients with Waldenström macroglobulinemia. J Clin Oncol. 2018;36(27):2755–61.
Dimopoulos MA, et al. Ibrutinib for patients with rituximab-refractory Waldenström’s macroglobulinaemia (iNNOVATE): an open-label substudy of an international, multicentre, phase 3 trial. Lancet Oncol. 2017;18(2):241–50.
Buske C, et al. Ibrutinib plus rituximab versus placebo plus rituximab for waldenström’s macroglobulinemia: final analysis from the randomized phase III iNNOVATE study. J Clin Oncol. 2022;40(1):52–62.
Tam CS, et al. A randomized phase 3 trial of zanubrutinib vs ibrutinib in symptomatic Waldenstrom macroglobulinemia: the ASPEN study. Blood. 2020;136(18):2038–50.
•• Dimopoulos MA, et al. Zanubrutinib versus ibrutinib in symptomatic Waldenström macroglobulinemia: final analysis from the randomized phase III ASPEN study. J Clin Oncol. 2023; 41(33):5099–5106. The phase III ASPEN study demonstrated the comparable efficacy and improved safety of zanubrutinib versus ibrutinib in patients with WM. The final analysis published reported the long term outcomes from ASPEN.
Advani RH, et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. J Clin Oncol. 2013;31(1):88–94.
Treon SP, et al. Long-term follow-up of ibrutinib monotherapy in symptomatic, previously treated patients with Waldenström macroglobulinemia. J Clin Oncol. 2021;39(6):565–75.
•• Dimopoulos MA, et al. A phase 3 clinical trial that evaluated the effect of adding ibrutinib to rituximab in patients with relapse/refractory and treatment naive WM. N Engl J Med. 2018;378(25):2399–2410. A phase 3 clinical trial that evaluated the effect of adding ibrutinib to rituximab in patients with relapse/refractory and treatment naive WM.
Buske C, et al. Ibrutinib treatment in Waldenström’s macroglobulinemia: follow-up efficacy and safety from the iNNOVATETM study. Blood. 2018;132:149.
Trotman J, et al. Zanubrutinib for the treatment of patients with Waldenstrom macroglobulinemia: 3 years of follow-up. Blood. 2020;136(18):2027–37.
An G, et al. A Phase II Trial of the Bruton Tyrosine-Kinase Inhibitor Zanubrutinib (BGB-3111) in Patients with Relapsed/Refractory Waldenström Macroglobulinemia. Clin Cancer Res. 2021;27(20):5492–5501.
•• Dimopoulos M, et al. Long-term follow-up results of a phase 3 randomized trial of zanubrutinib (Zanu) vs ibrutinib (Ibr) in patients (Pts) with Waldenstrom macroglobulinemia [abstract], in European Hematology Association Annual Meeting. 2022. ASPEN is the largest phase 3, head-to-head trial of zanubrutinib versus ibrutinib comparison in WM.
•• Owen RG, et al. Acalabrutinib monotherapy in patients with Waldenström macroglobulinemia: a single-arm, multicentre, phase 2 study. Lancet Haematol. 2020;7(2):e112–e121. A single-arm, multicentre, phase 2 trial with the aim to evaluate the activity and safety of acalabrutinib in patients with WM.
Sekiguchi N, et al. A multicenter, open-label, phase II study of tirabrutinib (ONO/GS-4059) in patients with Waldenstrom’s macroglobulinemia. Cancer Sci. 2020;111(9):3327–37.
Sekiguchi N, et al. Two-year outcomes of tirabrutinib monotherapy in Waldenström’s macroglobulinemia. Cancer Science, 2022;113(6):2085–2096.
• Cao X-x, et al. Evaluation of orelabrutinib monotherapy in patients with relapsed or refractory Waldenstrom's macroglobulinemia in a single-arm, multicenter, open-label, phase 2 study. eClinicalMedicine. 2022;52:101682. A prospective, multicenter study of orelabrutinib in patients with WM who had at least one prior line of treatment. The purpose of this study was to evaluate the efficacy and safety of orelabrutinib in patients with relapsed or refractory WM.
Cao X, et al. Orelabrutinib monotherapy in patients with relapsed or refractory Waldenström’s macroglobulinemia in a single-arm, multicenter, open-label, phase 2 study: long term follow-up results. Blood. 2023;142(Supplement 1):3039–3039.
Dimopoulos M, et al. Zanubrutinib for the treatment of MYD88 wild-type Waldenström macroglobulinemia: a substudy of the phase 3 ASPEN trial. Blood Adv. 2020;4(23):6009–18.
•• Mato AR, et al. Pirtobrutinib in relapsed or refractory B-cell malignancies (BRUIN): a phase 1/2 study. Lancet. 2021; 397(10277): 892-901. A prospective, multicenter study of orelabrutinib in patients with WM who had at least one prior line of treatment. The purpose of this study was to evaluate the efficacy and safety of orelabrutinib in patients with relapsed or refractory WM. A first-in-human, multicentre, open-label, phase 1/2 trial of pirtobrutinib with the goal to evaluate the safety and efficacy pirtobrutinib, a highly selective, reversible BTK inhibitor, in relapsed/refractory B-cell malignancies.
Palomba ML, et al. Efficacy of pirtobrutinib, a highly selective, non-covalent (Reversible) BTK inhibitor in relapsed / refractory Waldenström macroglobulinemia: results from the Phase 1/2 BRUIN study. Blood. 2022;140(Supplement 1):557–60.
Treon SP, Xu L, Hunter Z. MYD88 mutations and response to ibrutinib in Waldenström’s macroglobulinemia. N Engl J Med. 2015;373(6):584–6.
Zanwar S, Abeykoon JP, Kapoor P. Novel treatment strategies in the management of Waldenstrom Macroglobulinemia. Curr Hematol Malig Rep. 2020;15(1):31–43.
Paydas S. Management of adverse effects/toxicity of ibrutinib. Crit Rev Oncol Hematol. 2019;136:56–63.
Paulus A, et al. Waldenstrom macroglobulinemia cells devoid of BTK(C481S) or CXCR4(WHIM-like) mutations acquire resistance to ibrutinib through upregulation of Bcl-2 and AKT resulting in vulnerability towards venetoclax or MK2206 treatment. Blood Cancer J. 2017;7(5):e565.
Munir T, et al. Final analysis from RESONATE: up to six years of follow-up on ibrutinib in patients with previously treated chronic lymphocytic leukemia or small lymphocytic lymphoma. Am J Hematol. 2019;94(12):1353–63.
Leong DP, et al. The risk of atrial fibrillation with ibrutinib use: a systematic review and meta-analysis. Blood. 2016;128(1):138–40.
McMullen JR, et al. Ibrutinib increases the risk of atrial fibrillation, potentially through inhibition of cardiac PI3K-Akt signaling. Blood. 2014;124(25):3829–30.
Xiao L, et al. Ibrutinib-mediated atrial fibrillation attributable to inhibition of C-Terminal Src kinase. Circulation. 2020;142(25):2443–55.
Gustine JN, et al. Atrial fibrillation associated with ibrutinib in Waldenström macroglobulinemia. Am J Hematol. 2016;91(6):E312–3.
Vrontikis A, et al. Proposed algorithm for managing ibrutinib-related atrial fibrillation. Oncology (Williston Park). 2016;30(11):970–4 (980-1, c3).
Shanafelt TD, et al. Atrial fibrillation in patients with chronic lymphocytic leukemia (CLL). Leuk Lymphoma. 2017;58(7):1630–9.
Mock J, et al. Risk of major bleeding with ibrutinib. Clin Lymphoma Myeloma Leuk. 2018;18(11):755–61.
Yun S, et al. Risk of atrial fibrillation and bleeding diathesis associated with ibrutinib treatment: a systematic review and pooled analysis of four randomized controlled trials. Clin Lymphoma Myeloma Leuk. 2017;17(1):31-37.e13.
Shatzel JJ, et al. Ibrutinib-associated bleeding: pathogenesis, management and risk reduction strategies. J Thromb Haemost. 2017;15(5):835–47.
•• Tam CS, et al. A randomized phase 3 trial of zanubrutinib vs ibrutinib in symptomatic Waldenström macroglobulinemia: the ASPEN study. Blood. 2020;136(18):2038–2050. A novel phase 3 trial comparing the efficacy and safety of ibrutinib with zanubrutinib in patients with WM. The results demonstrate that zanubrutinib treatment was associated with a trend toward better response quality and less toxicity.
Rogers KA, et al. Incidence and description of autoimmune cytopenias during treatment with ibrutinib for chronic lymphocytic leukemia. Leukemia. 2016;30(2):346–50.
de Weerdt I, et al. Incidence and management of toxicity associated with ibrutinib and idelalisib: a practical approach. Haematologica. 2017;102(10):1629–39.
Brown JR, et al. Incidence of and risk factors for major haemorrhage in patients treated with ibrutinib: an integrated analysis. Br J Haematol. 2019;184(4):558–69.
Bye AP, et al. Ibrutinib inhibits platelet integrin alphaIIbbeta3 Outside-in signaling and thrombus stability but not adhesion to collagen. Arterioscler Thromb Vasc Biol. 2015;35(11):2326–35.
Levade M, et al. Ibrutinib treatment affects collagen and von Willebrand factor-dependent platelet functions. Blood. 2014;124(26):3991–5.
Bye AP, et al. Severe platelet dysfunction in NHL patients receiving ibrutinib is absent in patients receiving acalabrutinib. Blood Adv. 2017;1(26):2610–23.
Greil R, et al. Pretreatment with ibrutinib reduces cytokine secretion and limits the risk of obinutuzumab-induced infusion-related reactions in patients with CLL: analysis from the iLLUMINATE study. Ann Hematol. 2021;100(7):1733–42.
Bercusson A, et al. Ibrutinib blocks Btk-dependent NF-ĸB and NFAT responses in human macrophages during Aspergillus fumigatus phagocytosis. Blood. 2018;132(18):1985–8.
Varughese T, et al. Serious infections in patients receiving ibrutinib for treatment of lymphoid cancer. Clin Infect Dis. 2018;67(5):687–92.
Abeykoon JP, et al. Ibrutinib monotherapy outside of clinical trial setting in Waldenstrom macroglobulinaemia: practice patterns, toxicities and outcomes. Br J Haematol. 2020;188(3):394–403.
Gustine JN, et al. Ibrutinib discontinuation in Waldenström macroglobulinemia: etiologies, outcomes, and IgM rebound. Am J Hematol. 2018;93(4):511–7.
Castillo JJ, et al. Impact of ibrutinib dose intensity on patient outcomes in previously treated Waldenström macroglobulinemia. Haematologica. 2018;103(10):e466–8.
Hodge LS, et al. Constitutive activation of STAT5A and STAT5B regulates IgM secretion in Waldenstrom’s macroglobulinemia. Blood. 2014;123(7):1055–8.
Mahajan S, et al. Transcription factor STAT5A is a substrate of Bruton’s tyrosine kinase in B cells. J Biol Chem. 2001;276(33):31216–28.
• Castillo JJ, et al. Ibrutinib withdrawal symptoms in patients with Waldenström macroglobulinemia. Haematologica. 2018;103(7):e307–e310. A retrospective study the describes the symptoms of withdrawal and the rate of withdrawal symptoms in WM patients who hold ibrutinib therapy.
• Castillo JJ, et al. Ibrutinib and venetoclax in symptomatic, treatment-naive patients with Waldenström macroglobulinemia. Blood. 2023; 142(Supplement 1): 1661-1661. A prospective study evaluating ibrutinib and venetoclax in treatment-naive WM. This study presents the follow-up data after stopping therapy to assess ongoing safety and response durability in WM.
Barf T, et al. Acalabrutinib (ACP-196): a covalent bruton tyrosine kinase inhibitor with a differentiated selectivity and in vivo potency profile. J Pharmacol Exp Ther. 2017;363(2):240–52.
Byrd JC, et al. Acalabrutinib (ACP-196) in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374(4):323–32.
LP, A.P., CALQUENCE (acalabrutinib) capsules, for oral use Initial U.S. Approval: 2017.
Wu J, Zhang M, Liu D. Acalabrutinib (ACP-196): a selective second-generation BTK inhibitor. J Hematol Oncol. 2016;9:21.
Wang M, et al. Acalabrutinib in relapsed or refractory mantle cell lymphoma (ACE-LY-004): a single-arm, multicentre, phase 2 trial. Lancet. 2018;391(10121):659–67.
NCCN Clinical Practice Guidelines in Oncology Waldenstrom Macroglobulinemia/Lymphoplasmacytic Lymphoma. 2022 12/7/2021; Available from: https://www.nccn.org/professionals/physician_gls/pdf/waldenstroms.pdf.
Berinstein N, et al. Indolent lymphoma: high CR and VGPR rate with fixed duration Bendamustine, Rituximab and Acalabrutinib in Waldenstroms Macroglobulinaemia (BRAWM). Blood. 2023;142(Supplement 1):3037–3037.
Sarosiek SR, et al. Prospective study of acalabrutinib with rituximab in patients with symptomatic anti-MAG mediated IgM peripheral neuropathy. Blood. 2023;142(Supplement 1):213–213.
Tam CS, et al. Phase 1 study of the selective BTK inhibitor zanubrutinib in B-cell malignancies and safety and efficacy evaluation in CLL. Blood. 2019;134(11):851–9.
Ou YC, et al. A phase 1, open-label, single-dose study of the pharmacokinetics of zanubrutinib in subjects with varying degrees of hepatic impairment. Leuk Lymphoma. 2020;61(6):1355–63.
Opat S, et al. The MAGNOLIA trial: zanubrutinib, a next-generation bruton tyrosine kinase inhibitor, demonstrates safety and efficacy in relapsed/refractory marginal zone lymphoma. Clin Cancer Res. 2021;27(23):6323–32.
Tam CS, et al. Biomarker analysis of the ASPEN study comparing zanubrutinib to ibrutinib in patients with Waldenström Macroglobulinemia. Blood Adv 2024.
Chen J, et al. The effect of Bruton's tyrosine kinase (BTK) inhibitors on collagen-induced platelet aggregation, BTK, and tyrosine kinase expressed in hepatocellular carcinoma (TEC). Eur J Haematol 2018;101(5):604–612.
Liclican A, et al. Biochemical characterization of tirabrutinib and other irreversible inhibitors of Bruton’s tyrosine kinase reveals differences in on - and off - target inhibition. Biochim Biophys Acta Gen Subj. 2020;1864(4): 129531.
Kozaki R, et al. Responses to the selective Bruton’s Tyrosine Kinase (BTK) inhibitor tirabrutinib (ONO/GS-4059) in diffuse large b-cell lymphoma cell lines. Cancers. 2018;10(4):127.
Yahiaoui A, et al. PI3Kδ inhibitor idelalisib in combination with BTK inhibitor ONO/GS-4059 in diffuse large B cell lymphoma with acquired resistance to PI3Kδ and BTK inhibitors. PLoS ONE. 2017;12(2):e0171221.
Yasuhiro T, et al. Anti-tumor efficacy study of the Bruton’s tyrosine kinase (BTK) inhibitor, ONO/GS-4059, in combination with the glycoengineered type II anti-CD20 monoclonal antibody obinutuzumab (GA101) demonstrates superior in vivo efficacy compared to ONO/GS-4059 in combination with rituximab. Leuk Lymphoma. 2017;58(3):699–707.
Bates J, et al. The combination of a BET inhibitor (GS-5829) and a BTK inhibitor (GS-4059) potentiates DLBCL cell line cell death and reduces expression of MYC, IL-10, and IL-6 in vitro. Blood. 2016;128(22):5116–5116.
Dhillon S. Tirabrutinib: first approval. Drugs. 2020;80(8):835–40.
Walter HS, et al. A phase 1 clinical trial of the selective BTK inhibitor ONO/GS-4059 in relapsed and refractory mature B-cell malignancies. Blood. 2016;127(4):411–9.
Yamagami J, et al. A multicenter, open-label, uncontrolled, single-arm phase 2 study of tirabrutinib, an oral Bruton’s tyrosine kinase inhibitor, in pemphigus. J Dermatol Sci. 2021;103(3):135–42.
Dhillon S. Orelabrutinib: first approval. Drugs. 2021;81(4):503–7.
Xu L, et al. Acquired mutations associated with ibrutinib resistance in Waldenström macroglobulinemia. Blood. 2017;129(18):2519–25.
Chen JG, et al. BTK(Cys481Ser) drives ibrutinib resistance via ERK1/2 and protects BTK(wild-type) MYD88-mutated cells by a paracrine mechanism. Blood. 2018;131(18):2047–59.
Jimenez C, et al. Genomic evolution of ibrutinib-resistant clones in Waldenstrom macroglobulinaemia. Br J Haematol. 2020;189(6):1165–70.
Hershkovitz-Rokah O, et al. Ibrutinib resistance in mantle cell lymphoma: clinical, molecular and treatment aspects. Br J Haematol. 2018;181(3):306–19.
Zhang SQ, et al. Mechanisms of ibrutinib resistance in chronic lymphocytic leukaemia and non-Hodgkin lymphoma. Br J Haematol. 2015;170(4):445–56.
Paulus A. et al. Waldenstrom macroglobulinemia cells devoid of BTK(C481S) or CXCR4(WHIM-like) mutations acquire resistance to ibrutinib through upregulation of Bcl-2 and AKT resulting in vulnerability towards venetoclax or MK2206 treatment. Blood Cancer J. 2017;7(5):e565.
Woyach J, et al. Resistance to acalabrutinib in CLL is mediated primarily by BTK mutations. Blood. 2019;134(Supplement_1):504–504.
Estupiñán HY, et al. BTK gatekeeper residue variation combined with cysteine 481 substitution causes super-resistance to irreversible inhibitors acalabrutinib, ibrutinib and zanubrutinib. Leukemia. 2021;35(5):1317–29.
Handunnetti SM, et al. BTK Leu528Trp - a potential secondary resistance mechanism specific for patients with chronic lymphocytic leukemia treated with the next generation BTK inhibitor zanubrutinib. Blood. 2019;134(Supplement_1):170–170.
Brandhuber B, et al. LOXO-305, a next generation reversible BTK inhibitor, for overcoming acquired resistance to irreversible BTK inhibitors. Clin Lymphoma Myeloma Leuk. 2018;18:S216.
Reiff SD, et al. The Bruton’s Tyrosine Kinase (BTK) inhibitor ARQ 531 effectively inhibits wild type and C481S mutant BTK and is superior to ibrutinib in a mouse model of chronic lymphocytic leukemia. Blood. 2016;128(22):3232–3232.
Woyach J, et al. Final results of phase 1, dose escalation study evaluating ARQ 531 in patients with relapsed or refractory B-cell lymphoid malignancies. Blood. 2019;134(Supplement_1):4298–4298.
Wang E, et al. Mechanisms of resistance to noncovalent Bruton’s tyrosine kinase inhibitors. N Engl J Med. 2022;386(8):735–43.
Dale DC, et al. Oral administration of Mavorixafor, a CXCR4 antagonist, increases peripheral white blood cell counts across different disease states [abstract], in American Society of Hematology Annual Meeting 2021: Atlanta, Georgia.
• Abeykoon JP. et al. Bendamustine rituximab (BR) versus ibrutinib (Ibr) as primary therapy for Waldenström macroglobulinemia (WM): An international collaborative study. J Clin Onco 2022;40(16):7566–47566. A multi-institutional, international, collaborative study to compare BR and single-agent ibrutinib in patients with treatment naïve WM.
Tawfiq R, et al. Outcomes in treatment patterns after first relapse in patients with Waldenstrom macroglobulinemia [abstract], in European Hematology Association Annual Meeting. 2022.
Author information
Authors and Affiliations
Contributions
RKT, JPA and PK collected the data. RKT wrote the initial draft and prepared the tables. JPA edited the manuscript. PK revised the manuscript and the tables. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
RKT and JPA declare no competing interests. P.K is the principal investigator of trials for which Mayo Clinic has received research funding from Amgen, Regeneron, Bristol Myers Squibb, Loxo Pharmaceuticals, Ichnos, Karyopharm, Sanofi, AbbVie and GlaxoSmithKline. Prashant Kapoor has served on the Advisory Boards of BeiGene, Mustang Bio, Pharmacyclics, X4 Pharmaceuticals, AstraZeneca, Kite, Oncopeptides, Angitia Bio, GlaxoSmithKline, AbbVie and Sanofi.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tawfiq, R.K., Abeykoon, J.P. & Kapoor, P. Bruton Tyrosine Kinase Inhibition: an Effective Strategy to Manage Waldenström Macroglobulinemia. Curr Hematol Malig Rep (2024). https://doi.org/10.1007/s11899-024-00731-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11899-024-00731-0