Abstract
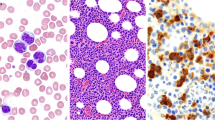
According to the recently published 2016 World Health Organization (WHO) classification of myeloid malignancies, myelodysplastic/myeloproliferative neoplasms (MDS/MPN) include atypical chronic myeloid leukemia (aCML), MDS/MPN-unclassifiable (MDS/MPN-U), chronic myelomonocytic leukemia (CMML), juvenile myelomonocytic leukemia (JMML), and MDS/MPN ring sideroblasts with thrombocytosis (MDS/MPN-RS-T). MDS/MPN-RS-T was previously a provisional category known as refractory anemia with ring sideroblasts with thrombocytosis (RARS-T) which has now attained a distinct designation in the 2016 WHO classification. In this review, we focus on biology and management of aCML, MDS/MPN-U, and MDS/MPN-RS-T. There is considerable overlap between these entities which we attempt to further elucidate in this review. We also discuss recent advances in the field of molecular landscape that further defines and characterizes this heterogeneous group of disorders. The paucity of clinical trials available secondary to unclear pathogenesis and rarity of these diseases makes the management of these entities clinically challenging. This review summarizes some of the current knowledge of the molecular pathogenesis and suggested treatment guidelines based on the available data.

Similar content being viewed by others
References
Sochacki AL, Fischer MA, Savona MR. Therapeutic approaches in myelofibrosis and myelodysplastic/myeloproliferative overlap syndromes. Onco Targets Ther. 2016;9:2273–86.
Arber DA et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Sallman DA, Padron E. Transformation of the clinical management of CMML patients through in-depth molecular characterization. Clin Lymphoma Myeloma Leuk. 2015;15(Suppl):S50–5.
Harada Y, Harada H. Chronic myelomonocytic leukemia (CMML): recent advances in molecular pathogenesis and treatment. Rinsho Ketsueki. 2016;57(2):147–55.
Adachi S, Nakahata T. Diagnosis and treatment of juvenile myelomonocytic leukemia (JMML). Nihon Rinsho. 2001;59(12):2401–6.
Koike K, Matsuda K. Molecular mechanism and progress in treatment of juvenile myelomonocytic leukemia (JMML). Rinsho Ketsueki. 2013;54(6):538–44.
Sakashita K. Juvenile myelomonocytic leukemia (JMML): recent advances in molecular pathogenesis and treatment. Rinsho Ketsueki. 2016;57(2):137–46.
Zoi K, Cross NC. Molecular pathogenesis of atypical CML, CMML and MDS/MPN-unclassifiable. Int J Hematol. 2015;101(3):229–42.
Bacher U et al. Distribution of cytogenetic abnormalities in myelodysplastic syndromes, Philadelphia negative myeloproliferative neoplasms, and the overlap MDS/MPN category. Ann Hematol. 2009;88(12):1207–13.
Meggendorfer M et al. SETBP1 mutations occur in 9% of MDS/MPN and in 4% of MPN cases and are strongly associated with atypical CML, monosomy 7, isochromosome i(17)(q10), ASXL1 and CBL mutations. Leukemia. 2013;27(9):1852–60.
Bellesso M et al. Atypical chronic myeloid leukemia with t(9;22)(p24,11.2), a BCR-JAK2 fusion gene. Rev Bras Hematol Hemoter. 2013;35(3):218–9.
Muta T, Osaki K, Yamano Y. Translocation t(9;22) (p23;q11) in atypical chronic myeloid leukemia (aCML) presenting osteolytic lesions. Int J Hematol. 2002;76(4):344–8.
Xu Y et al. A BCR-JAK2 fusion gene from ins(22;9)(q11;p13p24) in a patient with atypical chronic myeloid leukemia. Leuk Lymphoma. 2013;54(10):2322–4.
Wang SA et al. Atypical chronic myeloid leukemia is clinically distinct from unclassifiable myelodysplastic/myeloproliferative neoplasms. Blood. 2014;123(17):2645–51.
Gotlib J et al. The new genetics of chronic neutrophilic leukemia and atypical CML: implications for diagnosis and treatment. Blood. 2013;122(10):1707–11.
Piazza R et al. Recurrent SETBP1 mutations in atypical chronic myeloid leukemia. Nat Genet. 2013;45(1):18–24.
Breccia M et al. Identification of risk factors in atypical chronic myeloid leukemia. Haematologica. 2006;91(11):1566–8.
Hernandez JM et al. Clinical, hematological and cytogenetic characteristics of atypical chronic myeloid leukemia. Ann Oncol. 2000;11(4):441–4.
Martiat P, Michaux JL, Rodhain J. Philadelphia-negative (Ph-) chronic myeloid leukemia (CML): comparison with Ph + CML and chronic myelomonocytic leukemia. The Groupe Francais de Cytogenetique Hematologique. Blood. 1991;78(1):205–11.
Kurzrock R et al. BCR rearrangement-negative chronic myelogenous leukemia revisited. J Clin Oncol. 2001;19(11):2915–26.
Maxson JE et al. Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N Engl J Med. 2013;368(19):1781–90.
Maxson JE et al. The colony-stimulating factor 3 receptor T640N mutation is oncogenic, sensitive to JAK inhibition, and mimics T618I. Clin Cancer Res. 2016;22(3):757–64.
Geyer JT, Orazi A. Myeloproliferative neoplasms (BCR-ABL1 negative) and myelodysplastic/myeloproliferative neoplasms: current diagnostic principles and upcoming updates. Int J Lab Hematol. 2016;38(1):12–9. doi:10.1111/ijlh.12509.
Gambacorti-Passerini CB et al. Recurrent ETNK1 mutations in atypical chronic myeloid leukemia. Blood. 2015;125(3):499–503.
Hoischen A et al. De novo mutations of SETBP1 cause Schinzel-Giedion syndrome. Nat Genet. 2010;42(6):483–5.
Khanna V et al. Durable disease control with MEK inhibition in a patient with NRAS-mutated atypical chronic myeloid leukemia. Cureus. 2015;7(12):e414.
Cortes J et al. Results of imatinib mesylate therapy in patients with refractory or recurrent acute myeloid leukemia, high-risk myelodysplastic syndrome, and myeloproliferative disorders. Cancer. 2003;97(11):2760–6.
Koldehoff M et al. Outcome of hematopoietic stem cell transplantation in patients with atypical chronic myeloid leukemia. Bone Marrow Transplant. 2004;34(12):1047–50.
DiNardo CD et al. Myelodysplastic/myeloproliferative neoplasms, unclassifiable (MDS/MPN, U): natural history and clinical outcome by treatment strategy. Leukemia. 2014;28(4):958–61.
Chaudhury A et al. Prognosis and outcomes in MDS-MPN unclassifiable: single institution experience of a rare disorder. Blood. 2015;126(23):1698.
Alchalby H, Kroger N. Allogeneic stem cell transplant vs. Janus kinase inhibition in the treatment of primary myelofibrosis or myelofibrosis after essential thrombocythemia or polycythemia vera. Clin Lymphoma Myeloma Leuk. 2014;14 Suppl:S36–41.
Eghtedar A et al. Phase 2 study of the JAK kinase inhibitor ruxolitinib in patients with refractory leukemias, including postmyeloproliferative neoplasm acute myeloid leukemia. Blood. 2012;119(20):4614–8.
Cherington C et al. Allogeneic stem cell transplantation for myeloproliferative neoplasm in blast phase. Leuk Res. 2012;36(9):1147–51.
Steensma DP, Tefferi A. JAK2 V617F and ringed sideroblasts: not necessarily RARS-T. Blood. 2008;111(3):1748.
Papaemmanuil E et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365(15):1384–95.
Effenberger KA et al. Interchangeable SF3B1 inhibitors interfere with pre-mRNA splicing at multiple stages. RNA. 2016;22(3):350–9.
Broseus J et al. Age, JAK2(V617F) and SF3B1 mutations are the main predicting factors for survival in refractory anaemia with ring sideroblasts and marked thrombocytosis. Leukemia. 2013;27(9):1826–31.
Jeromin S et al. Refractory anemia with ring sideroblasts and marked thrombocytosis cases harbor mutations in SF3B1 or other spliceosome genes accompanied by JAK2V617F and ASXL1 mutations. Haematologica. 2015;100(4):e125–7.
Broseus J et al. Low rate of calreticulin mutations in refractory anaemia with ring sideroblasts and marked thrombocytosis. Leukemia. 2014;28(6):1374–6.
Klampfl T et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013;369(25):2379–90.
Broseus J et al. Clinical features and course of refractory anemia with ring sideroblasts associated with marked thrombocytosis. Haematologica. 2012;97(7):1036–41.
Cazzola M et al. Biologic and clinical significance of somatic mutations of SF3B1 in myeloid and lymphoid neoplasms. Blood. 2013;121(2):260–9.
Cortelazzo S et al. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med. 1995;332(17):1132–6.
Huls G et al. Efficacy of single-agent lenalidomide in patients with JAK2 (V617F) mutated refractory anemia with ring sideroblasts and thrombocytosis. Blood. 2010;116(2):180–2.
Ziarkiewicz M et al. Refractory anaemia with ringed sideroblasts associated with marked thrombocytosis (RARS-T) with superimposed 5q-syndrome. Pol J Pathol. 2010;61(2):105–9.
Taylor G, Culligan D, Vickers MA. Refractory anemia with ring sideroblasts associated with marked thrombocytosis complicated by massive splenomegaly treated with lenalidomide resulting in resolution of splenomegaly but severe and prolonged pancytopenia. Case Rep Hematol. 2013;2013:718480.
Savona MR et al. An international consortium proposal of uniform response criteria for myelodysplastic/myeloproliferative neoplasms (MDS/MPN) in adults. Blood. 2015;125(12):1857–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Chetasi Talati and Eric Padron each declare no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Myelodysplastic Syndromes
Rights and permissions
About this article
Cite this article
Talati, C., Padron, E. An Exercise in Extrapolation: Clinical Management of Atypical CML, MDS/MPN-Unclassifiable, and MDS/MPN-RS-T. Curr Hematol Malig Rep 11, 425–433 (2016). https://doi.org/10.1007/s11899-016-0350-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-016-0350-1