Abstract
The incidence of acute myeloid leukemia (AML) is expected to increase in conjunction with our ageing population. Although it is proving to be a heterogeneous disease process, the only treatment with proven survival benefit for poor risk AML remains allogeneic hematopoietic cell transplant. Although this is presumed to be a curative strategy, many patients relapse after transplant, prompting us to examine various ways that we can improve outcomes. These efforts involve every step of AML diagnostics and therapy, including the intricate processes of conditioning, graft manipulation and immunomodulation. The hope is that improvement in these steps will ultimately improve survival and decrease relapse rates for AML patients after transplant.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic cell transplantation (allo-HCT) is an important and widely used treatment for patients with hematological malignancies, including acute myeloid leukemia (AML) and high-risk myelodysplastic syndrome (MDS). An estimated 20,000 patients receive allo-HCT each year, and while the procedure can be a patient’s sole potentially curative option, post-transplant relapse is common. According to the Center for International Bone Marrow Transplant Registry (CIBMTR), relapse rates following HLA-matched myeloablative transplantation range from approximately 25 % for good-risk patients [i.e., AML in first complete remission (CR1) or chronic myeloid leukemia (CML) in chronic phase] to over 60 % for poorest risk patients (those transplanted in relapse). Factors influencing relapse (for better or worse) can be classified as intrinsic to the disease, the allo-HCT preparative regimen, or the interaction between the disease and the transplanted immune system. For all of the sophisticated work performed on this problem, it is certain that we have only an initial understanding of the elements driving post-HCT AML relapse [1, 2••]. In this review, we outline current strategies to study and treat AML relapse after allo-HCT with an emphasis on new innovative investigational approaches (Table 1). While treatment elements designed to reduce relapse can be categorized as pre-HCT, intra-HCT or post-HCT strategies, many of these approaches are relevant to more than one category.
Prognostic (Biological) AML Markers
Cytogenetics and Relapse after Allo-HCT
When considering non-transplant therapy (induction and consolidation) for AML, age, cytogenetics and response to therapy remain major predictors of outcome. Similarly, patients with poor-risk cytogenetics are known to fare worse after allo-HCT than patients with a more favorable karytotype [3–5]. However, Tallman et al. compared matched unrelated allo-HCT in CR1 (261 patients) to those transplanted in second CR (CR2 = 299 patients), and showed that favorable cytogenetics were associated with improved outcome only in CR2 transplants [6]. Importantly, normal cytogenetics confer only intermediate (as opposed to favorable) prognosis in adult AML, while the worst risk is associated with a monosomal karyotype (MK) or complex cytogenetics (≥3 anomalies). It is this poorest risk group that derives the most benefit in terms of relapse rates and survival after allo-HCT [6].
Sub-Cytogenetic Molecular Changes and Allo-HCT Replase
A growing number of sub-cytogenetic molecular anomalies have prognostic implications before and after allo-HCT in AML. For example, mutations occurring in the core binding factor [t(8:21) and inv 16] or the B23/nucleophosmin (NPM1) locus are associated with potential cure following high dose cytarabine regimens, allowing for the avoidance of allo-HCT. Even so, up to 20–30 % of apparent favorable-risk cases carry a prevailing c-kit proto-oncogene mutation responsible for decreased overall survival [7].
A major target for AML molecular therapy is the FLT3-ITD (internal tandem duplication) mutation, which is very common in adult leukemia and causes constitutive tyrosine kinase activation. Drafting off the success of imatinib in CML, new tyrosine kinase inhibitors (TKIs) such as sorafenib, sunitinib, midostaurin, and more recently AC220 and PLX3397, are being used singly or with chemotherapy in AML clinical trials. Metzelder et al. treated three relapsed/refractory AML patients prior to allo-HCT with sorafenib monotherapy. Two of the patients had remissions followed by allo-HCT [8]. AC220 is the subject of an ongoing Phase II trial for the treatment of resistant/relapsed AML. Two cohorts are being studied; Cohort 1 includes patients over 60 years who are refractory to one therapy, and Cohort 2 has patients over 18 years who are refractory to two regimens. AC220 achieved a composite partial remission (PR) rate of 19 % and a CR rate of 62 %. Median overall survival (OS) is 24.7 weeks for efficacy evaluable patients, 24.1 weeks for Cohort 1, and the data is not complete yet for Cohort 2 [9]. PLX3397 [10] is also a highly selective inhibitor of FLT3-ITD, c-fms and c-kit that is currently being studied at the Fred Hutchinson Cancer Research Center in FLT3 mutation positive AML refractory to conventional therapy in a phase I clinical trial. Compared to the dramatic success in CML, expectations for TKIs in AML are more limited, due to the extremely complex molecular etiology and evolution, and rapid progression of the acute disease. Disease stabilization and CRs may be short-lived, suggesting that resistance to the drugs develops quickly. Theoretically, resistance may be circumvented by applying concurrent therapies with diverse molecular targets and modes of action against the aberrant signal transduction in leukemic blasts.
Quality of CR Prior to Allo-HCT and the Effect on Relapse after Allo-HCT
Complete remission in AML (defined as the presence on bone marrow morphologic analysis of less than 5 % blasts and normal peripheral counts) remains the goal of induction and consolidation chemotherapy, and is an eligibility requirement for transplant at most centers performing allo-HCT. For patients with low-risk disease, as noted above, chemotherapy induced CR may be all that is required for cure. However, for intermediate-risk and poor-risk disease, patients should be referred for allo-HCT, which is the sole potentially curative approach.
Estimates of the probability of overall survival and disease-free survival for acute myeloid leukemia (AML) first complete remission (CR1) patients with negative versus positive minimal residual disease (MRD) via multi-parametric flow cytometry results pre-allo-HCT [12•]
Growing evidence supports the conclusion that the prognostic function of the morphologic CR can be improved by further qualification. CR with minimal residual disease (MRD) refers to a morphologic blast count <5 % with any detectable persistence of the leukemic clone. Evaluation of MRD includes histology techniques with a 1–5 % limit of detection (LOD) (similar to cytogenetic culture techniques). Molecular approaches to determining MRD include fluorescent in situ hybridization (FISH: up to 0.5 % LOD), flow cytometry analysis (0.1 % to 0.01 % LOD) [11], or polymerase chain reaction (PCR: LOD is the most sensitive, but will vary depending on the specific characteristics of the primer set and reaction conditions). A recent study evaluated the presence of MRD (detected by ten color flow cytometry) and the clinical outcomes of 99 patients who received standard chemotherapy followed by allo-HCT (Fig. 1). MRD-positivity was associated with a hazard ratio of 4.05 for overall mortality and an 8.49 hazard ratio for relapse when compared to the MRD-negative cohort [12•]. Similarly, data from 254 patients treated at MD Anderson Cancer Center revealed persistance of cytogenetic abnormalities at the time of morphologic CR in 28 % of cases. Patients with MRD had median relapse free survival (RFS) and OS of 6 months and 11 months, compared to median RFS and OS of 21 months and 26 months in patients with normal karyotype at CR. Patients with persistent cytogenetic abnormalities who underwent stem cell transplant had an improved survival compared to those who did not undergo transplant (3 year RFS 33 % and 9 %, OS 33 % and 8 %, respectively) [13•]. These data underscore the importance of obtaining a CR by the most sensitive analysis. Therefore, although the optimal timing and method of analysis is unclear, MRD is a prognostic factor of growing importance.
Conditioning regimens for allo-HCT (figure courtesy of H.J. Deeg) [2••]
AML Induction Agents
Based on the critical importance of a high-quality CR, induction and consolidation are pivotal components of a patients’ success after allo-HCT. However, no induction regimen has yet demonstrated a significantly improved outcome compared to the standard three days of anthracycline and seven days of cytarabine (so-called “7 + 3”). Dose intensity appears critical, since 90 mg/m2 of daunorubicin was shown to improve outcomes with minimal additional toxicity compared to 45 mg/m2, even in the elderly [14, 15]. Importantly, it not yet clear that the improved CR rate translates into more patients proceeding to allo-HCT or a superior post-allo-HCT relapse rate.
To improve induction responses, some approaches try to sensitize leukemic blasts to standard chemotherapy. For example, a Phase I study added the hypomethylating agent decitabine to standard 7 + 3 induction as a form of “epigenetic priming”. Of 30 patients evaluated, 83 % achieved a CR [16]. Further studies are in process to validate these findings. In vitro studies also show a synergistic anti-tumor effect of clofarabine (a nucleoside analogue) with cytarabine by increasing intracellular levels of ara-CTP. Phase II trials using clofarabine and cytarabine in older AML patients in the relapsed and de novo setting demonstrate tolerable side effect profiles, and potentially improved outcomes [17, 18].
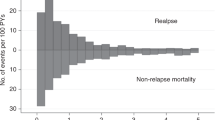
Transplant Strategies to Reduce Relapse
Allo-HCT may be the best chance for a curative modality for patients with intermediate-risk or high-risk AML (including patients with relapsed disease). Fear of relapse after allo-HCT has prompted studies to improve conditioning regimens through intensification, and manipulation of the graft-versus-leukemia (GVL) effect (the rationale behind the feasibility of reduced-intensity HCT; Fig. 2). The challenge is balancing the risk of graft-vs-host disease (GVHD) and other causes of transplant-related mortality (TRM) with relapse.
Modifications of Allo-HCT Conditioning Regimens
Modified Total Body Irradiation (TBI) Dosing
A randomized trial of AML in CR1 demonstrated a decreased relapse rate of 12 % after 15.75 Gy of TBI, compared to 35 % after 12 Gy, with similar OS [19]. Importantly, patients receiving higher radiation doses also received less GVHD immune prophylaxis, and therefore had a higher incidence of acute GVHD. Since the GVL effect is thought to accompany GVHD, the decreased relapse rates may have been a result of the increased TBI, the increased GVL, or both. However, patients who received higher TBI dosing also had increased rates of transplant related mortality, equalizing the overall survival rates between the two groups.
Modified Chemotherapy Regimens
Various conditioning regimens continue to be tested in an effort to improve allo-HCT outcomes and decrease AML relapse rates. A Phase I/II study transplanted 46 patients with hematologic malignancies and persistent disease (31 of which had AML) using clofarabine in combination with myeloablative doses of busulfan. This regimen yielded 100 % engraftment and CR in all of the AML patients without prior allo-HCT [20•]. Overall survival in all patients was 48 % at 1 year and 35 % at 2 years. Another ongoing trial randomizes patients with advanced AML/MDS to four arms comprised of busulfan in combination of varied doses of clofarabine and fludarabine. All patients treated so far have engrafted, with an 85 % CR rate at interim analysis [21]. Together, these studies show promising results in patients with high-risk/refractory AML undergoing transplant; however, the effect of these regimens on relapse remains to be determined.
Radioimmunotherapy
Monoclonal antibodies provide a targeted therapeutic approach to hematologic malignancies, best demonstrated by the success of Rituximab in non-Hodgkin lymphoma. Antibodies specific to a variety of antigens, (such as CD45, an epitope widely expressed on most hematologic tissues), are being investigated as targeted radioisotope conditioning regimens for allo-HCT. Anti-CD45 antibodies conjugated to radioiodine deliver radiation specifically to the marrow space, with decreased global morbidity in leukemic patients. A Phase I/II trial performed at the FHCRC used this approach in combination with targeted busulfan and cyclophosphamide to condition 59 AML patients. At 3 years, the non-relapse mortality was 21 %, with disease-free survival (DFS) estimated at 61 % [22]. Compared to similar patients from the International Bone Marrow Transplant Registry, the hazard of mortality of antibody-treated patients was 0.65 (95 % CI 0.39–1.08; P = 0.09). Another study evaluated the maximum tolerated dose (MTD) of the 131I-anti-CD45 antibody that can be combined with standard reduced-intensity conditioning regimen prior to allo-HCT in older patients with advanced AML or high-risk MDS. There was a 12 % TRM by day 100, with estimated 1-year relapse rate of 40 % and 1-year survival estimate of 41 % [23•]. Together, the data regarding radiolabeled anti-CD45 antibodies suggest a strategy for specific targeted stem cell ablation with the potential to reduce relapse.
Modulation of the Graft and the GVL/GVHD Effect
Reduced-Intensity Allo-HCT
Reduced-intensity transplantation (RIT) strategies were developed based on the observation that non-twin HLA-identical sibling donors conferred a superior relapse free survival compared to identical twin donors, revealing a GVL effect. In time, this observation led to successful experimentation with reduced intensity conditioning regimens (non-myeloablative regimens) that relied upon the donor immune system to deliver the cell mediated anti-tumor effect. The reduced intensity conditioning, with lower upfront mortality, allowed extension of the upper age limits for a patient to receive allo-HCT. Recent work by Sorror et.al at demonstrated a similar TRM among selected patients receiving RIT in a 60–65-year-old, 65–70-year-old, and 70–75-year-old cohort of patients [24]. Another study evaluated 122 patients with various stages of AML conditioned with 2 Gy TBI, either with or without fludarabine, as well as cyclosporine and MMF for post-HCT immunosuppression. Overall 2-year survival was 48 % and DFS was 44 % [25]. However, relapse rates at 2 years were still 39 % for all patients treated. Similarly, another study of 79 AML patients ≥55 years of age used non-myeloablative doses of busulfan and fludarabine prior to allo-HCT. Although these patients largely had a good performance status, their 1-year TRM was around 20 %, with 2 year overall survival at 46 % [26]. Relapse after transplant of all patients was estimated around 58 %. Not surprisingly, patients with lower-risk AML prior to allo-HCT had improved survival post-transplant. An additional study used RIT conditioning with fludarabine and melphalan in 36 patients considered ineligible for myeloablative allo-HCT. These patients had a median age of 57 years and 72 % of patients had a co-morbidity score ≥3. With a median follow-up of 52 months, OS and PFS rates at 4 years were 71 % and 68 %, respectively. The 4-year cumulative incidence of non-relapse mortality was 20 % and importantly, relapse mortality was only 8 % [27]. These and other studies reveal that reduced-intensity allo-HCT may provide a survival benefit by reducing relapse in selected older AML patients with higher comorbidity scores. The feasibility of RIT relies heavily on the GVL effect, which often comes with increased risk of GVHD. The challenge of maximizing GVL without concurrent immune-mediated end-organ damage has driven efforts to manipulate the donor cells with additional immune modulation.
Graft Engineering
Different immunosuppression regimens and timing have been evaluated in an effort to dampen the alloreactive donor T cell response from the transplanted graft. Unfortunately, it is widely accepted that our inability to specifically target the alloreactive response diminishes the global T cell response and decreases GVL. T cell depletion and/or removal of specific T cell subsets can be accomplished in vitro pre-transplant with CD34+ cell selection or in vivo after cell infusion with the use of the anti-CD52 antibody alemtuzumab. Jakubowski et al. used T cell depleted HLA-matched related PBSC allografts in 52 patients (almost half with AML/MDS) after conditioning with fludarabine, thiotepa and hyper-fractionated TBI [28]. In the absence of immunosuppression, 3-year DFS was estimated to be 61 % in all patients and 3-year OS was estimated to be 62 %, with grade 2 acute GVHD detected in 8 % and chronic GVHD in 9 % of patients. Only six of the AML/MDS patients had hematologic or molecular evidence of relapse, suggesting that T cell depletion may help tip the scales in favor of GVL effect. Although no immune-mediated graft rejection occurred, a large proportion of the patients had absolute CD4 counts <200 cells/μL for more than 7 months. In a related study using HLA-matched unrelated stem cell donors, anti-thymocyte globulin (ATG) was added after allo-HCT as GVHD prophylaxis. In this case, 34 patients were transplanted with a 4-year estimated DFS of 56.8 % among all patients. Nine percent had grade II-III acute GVHD and 29 % had chronic GVHD, with only one late graft failure [29]. Only one AML patient relapsed (with poor-risk cytogenetics), again highlighting the possibility that GVL effect can be maintained while minimizing GVHD and the need for long term immunosuppression. Additionally, the Bone Marrow Transplant Clinical Trials Network transplanted 44 AML patients in CR1 or CR2 with chemotherapy/TBI conditioning, followed by T cell depleted grafts from HLA-matched donors (no GVHD immune prophylaxis was given). All patients engrafted in this trial, with a 22.7 % incidence of acute GVHD grade II–IV, and a 6.8 % incidence of chronic GVHD at 1 year. The 3-year relapse rate for CR1 patients was 17.4 %, with a 58 % DFS at 3 years [30].
Technically complicated methods have been devised to specifically remove alloreactive or naïve T cells from the donor graft. These strategies have been challenging to transition to the clinical setting, but provide potential for mitigating GVHD [31, 32]. Another strategy for depleting alloreactive T cells involves a large dose of cyclophosphamide early after the infusion of a T cell replete graft. This reduced the incidence of severe GVHD in haploidentical HLA matched transplant recipients [33]. Alternatively, the introduction of an inducible suicide gene could cause self-destruction of alloreactive T cells, while potentially maintaining GVL effect. These strategies may potentially maintain the integrity of the immune mediated prevention of relapse, while minimizing the morbidity and mortality associated with GVHD.
Relapse Management and Maintenance Strategies After Allo-HCT
Return of AML after transplant is of ominous portent, and relapse is fatal in the majority of patients. Commonly, the first maneuver is to reduce immunosuppression to stimulate any potential GVL effect; however, this can be a great challenge to the patient and clinician when faced with concomitant GVHD. Donor lymphocyte infusion (DLI) can be employed as a post-HCT infusion of a reserved portion of donor cells, intended to induce a GVL effect during relapse. Also discussed in this section are emerging new techniques applied after allo-HCT to further prevent relapse and improve outcomes.
Donor Lymphocyte Infusion
The role of donor lymphocyte infusion (DLI) after allo-HCT for AML is not well defined. For reasons likely attributable to the rapid natural history of AML relapse, the administration of additional donor cells result in relatively low response rates, since DLI may require a prolonged time to be effective [2••]. Nevertheless, as previously mentioned, there has been ample evidence of a GVL effect against AML post allo-HCT. This is inferred from the observation that allo-HCT recipients from syngeneic donors (lacking significant antigenic disparity) have a higher relapse rate, and additional evidence that GVHD is associated with a lower relapse rate [34]. It is interesting, therefore, that a large prospective randomized trial showed similar relapse rates for AML patients who were transplanted with T cell depleted grafts versus unmanipulated grafts from unrelated donors [35].
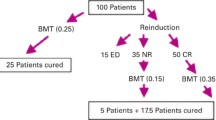
Two large retrospective analyses published estimated a response rate of 15–29 % for AML relapse treated with DLI [36, 37]. Interestingly, many of these patients relapse with extramedullary disease, suggesting areas that are sanctuary sites [38]. A European Group for Blood and Marrow Transplantation retrospective analysis surveyed 399 relapsed AML patients, in which 171 received DLI (including those who received mobilized PBSC or marrow concentrates), and 75 % received chemotherapy prior to the infusion. The estimated 2-year survival in the DLI group was 21 % versus 9 % in the untreated cohort, and fewer patients from the DLI group were sent to a second transplant procedure. Factors associated with improved outcomes by univariate analysis included: age <37 years, relapse later than 5 months after allo-HCT, and the use of DLI. Favorable elements on multivariate analysis included: female sex, favorable cytogenetics, remission at time of DLI, and less than 35 % bone marrow blasts. Thirty-five of 106 DLI patients with active leukemia achieved complete remission. Remarkably, acute GVHD was associated with a poorer outcome; however, chronic GVHD was linked to improved outcomes [39]. These results suggest that DLI can improve survival in the setting of relapse after allo-HCT, likely due to an intensified GVL effect that is often accompanied by chronic GVHD.
Augmented DLI
DLI strategies have included co-administration of immunomodulatory cytokines or chemotherapy to reduce relapse. Levine et al. treated 65 patients with relapsed AML using augmented cytarabine based chemotherapy prior to DLI. Median time to relapse was 100 days after allo-HCT in these patients, and the median period between relapse and DLI was 19 days. Forty-two percent of patients achieved a CR with DLI, yet only 14 % were in CR at 29 months after infusion. The most important predictor of OS was the time from allo-HCT to relapse [40]. This approach seemed to provide temporary disease control in the setting of post-transplant relapse. However the prognostic importance of time to relapse is a surrogate for the aggressive nature of AML, which may outpace the GVL effect of DLI. Donor lymphocyte priming has been investigated using ex vivo activation of the DLI product with the intent of further augmenting GVL. While the technique can be labor intensive and costly, there have been small studies applying this approach in humans. Porter et al. used anti-CD3 and anti-CD28 coated beads for ex-vivo co-stimulation of donor T cells. Eighteen patients were treated with conventional DLI, followed by activated product in escalating doses. Eight patients achieved CR, including 2/4 patients with AML [41]. Future targets for donor lymphocyte priming could generate tumor specific T cells using peptides specific to myeloid blasts, such as PR1 and WT1.
Alternate DLI Timing
Prophylactic DLI (infusion prior to clinical evidence of relapse) has been employed following allo-HCT for AML. Schmid et al. planned prophylactic DLI for day 120, following reduced-intensity allo-HCT for high risk AML or MDS. However, only 12 of 75 patients were eligible at that time, due to relapse or sustained GVHD requiring immunosuppression [42]. However, of these 12 patients, only two had relapsed, with the rest of the patients remaining in CR, with a median follow-up of 31.5 months after allo-HCT. In contrast, prophylactic DLI was administered after full intensity T cell depleted allogeneic transplants with promising results by Kobbe et al. Seventy-four percent of 14 patients with AML/MDS showed disease-free survival at 1 year, with minimal GVHD [43]. Of the six AML/MDS patients who died, three had relapsed. Currently, it is unclear whether prophylactic DLI is a feasible approach that significantly improves relapse rates after allo-HCT.
Targeted Tyrosine Kinase Inhibitors Pre and Post-HCT for AML
As discussed in the pre-transplant section of this article, the tyrosine kinase inhibitors (TKI) sorafenib, sunitinib, midostaurin, PLX3397, and AC220 have been used singly or in combination with chemotherapy in adult AML, targeting c-Kit and FLT3 mutations. An exciting potential maneuver after allo-HCT has been the use of TKIs as relapse treatment or maintenance therapy, vis a vis Imatinib after allo-HCT for CML. In the work by Metzelder and colleagues, two of three patients treated sorafenib after allo-HCT survived 216 and 221 days, and the other remained in molecular remission at the time of publication [8]. However, Sharma et al. also treated 16 post-HCT relapsed patients with the FLT3-ITD mutation with sorafenib alone or in combination with systemic chemotherapy. None of these advanced patients achieved a CR, and while three patients achieved a partial remission, the median OS of these patients was only 83 days, with no one surviving longer than 1 year [44]. AC220 is a second generation FLT3 inhibitor that is thought to be more specific and potent than sorafenib, with ongoing studies evaluating its efficacy as prophylaxis for relapse after allo-HCT.
Epigenetic Modifiers Peri-transplant
5-azacitidine and decitabine are hypomethylating agents used in the treatment of de novo MDS and AML, and they may have a role for relapse prophylaxis or treatment after allo-HCT. 5-azacitidine is thought to promote blast differentiation and increase the GVL effect by upregulating HLA-DR1 and other tumor associated antigens [45, 46]. Pre-clinical data from Choi et al. suggests that hypomethylating agents induce the activation of regulatory T cells, suppressing GVHD while preserving GVL in mice [47]. Moreover, in humans with relapsed AML after allo-HCT, a retrospective analysis of ten patients revealed that treatment with 5-azacitidine in this setting induced CR in six patients and stabilized disease in one patient, with no GVHD flares observed. To date, median OS for the group was >400 days, suggesting that this approach may be important for managing relapse in these high-risk post-HCT patients [48]. De Lima et al. treated 45 patients with MDS or AML using various doses of 5-azacitidine as maintenance after allogeneic HCT. Although median follow-up was only 20.5 months at the time of publication, the 1-year event-free and OS proved encouraging at 58 % and 77 % respectively, providing support for further studies [49]. Suberoylanilide hydroxamic acid (SAHA), a histone deacetylase (HDAC) inhibitor, may also have activity against AML and has the potential to prevent allo-HCT relapse in future approaches. A Phase I study investigated the safety of the HDAC inhibitor without allo-HCT in 41 leukemia patients, 31 of which had AML. Seven patients had hematologic improvement (reduction of blasts by >50 %), including two CR and two CR with incomplete count recovery. All of the responding patients had AML, treated at or below the maximum tolerated dose, perhaps paving the way for exploration of HDAC inhibitors in the setting of relapse prophylaxis [50].
Vaccine Therapy for AML
Research is ongoing to manipulate the recipient or donor immune response, so that tumor specific antigens are recognized and targeted. Various antigen, APC and cytokine stimulants are being tested to promote a lasting immune response in the setting of relapsed leukemia or MRD after transplant. This challenge is compounded by cancer’s ability to evade ones native immunity via down regulation of tumor antigens, MHC complexes or costimulatory molecules [51].
WT-1 (Wilm’s Tumor gene) and PR1 have been the predominant antigens targeted for leukemia vaccine development. WT-1 codes for a transcription factor that has been shown to be over-expressed in myeloid leukemias and involved in cell proliferation [52, 53]. Mailander et al. reported a promising CR after an HLA-A2 patient with relapsed AML was treated with a combination vaccine that included WT-1 peptide primed T cells combined with a T helper protein and GM-CSF [54]. The same group then treated 17 AML and two MDS HLA-A2 positive patients with a WT-1 peptide vaccine in a Phase II trial. Ten patients maintained stability of their disease, including four patients with stable disease, with more than 50 % blast reduction, and one patient who obtained CR. Significantly, these results correlated with demonstrable increase in WT-1 specific T cells and decreased WT-1 mRNA [55]. Rezvani et al. treated eight patients with myeloid malignancies using a combination vaccine against both WT-1 and PR1 peptides. After one vaccination, peptide specific T cells increased and WT-1 and PR1 mRNA decreased. However, subsequent vaccination led to rapid loss of high-avidity peptide specific CD8+ cells, correlating to loss of clinical response [56].
Unfortunately, vaccine trials have not produced prolonged, clinically significant improvement of AML to date, and their role in relapse prevention remains unknown. Several questions remain regarding the optimal antigen, effector cell, timing or cytokine adjuncts that may produce a durable specific response. In the setting of HLA-matched allo-HCT, minor histocompatability antigens may also be a potential target for stimulating a GVL effect. Minor histocompatability antigens such as HA-1 and HA-2 expressed exclusively on hematopoietic derived cells of the recipient could be targets of reactive T cells [57]. Li et al. infused memory T cells from donors vaccinated against a single minor histocompatability antigen (H60) expressed by leukemia cells. This strategy showed a promising GVL effect in a mouse model of CML [58]. Currently Phase I/II trials are underway to evaluate the potential role of peptide vaccines for myeloid malignancies in the post-HCT setting, and results are eagerly anticipated.
Conclusions
The landscape of AML treatment and relapse prevention after allogeneic HCT continues to evolve with advancing developments using a variety of novel approaches. We are discovering that every step of the disease treatment is essential in decision making and improving the chances of survival. Cytogenetic and molecular mutations greatly affect response to induction, as well as relapse rates and success after transplant. Our attempt to manipulate the balance between GVL and GVHD via ex vivo graft modification and vaccines proves to be arduous and costly. However, advances in conditioning regimens, graft engineering, vaccines, and epigenetic modifiers have provided insight into the future of allo-HCT for AML, with a promise of significantly less relapse.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Porter DL, Alyea EP, Antin JH, et al. NCI First International Workshop on the Biology, Prevention, and Treatment of Relapse After Allogeneic Hematopoietic Stem Cell Transplantation: report from the committee on treatment of relapse after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2010;16:1467–503.
•• Alyea EP, DeAngelo DJ, Moldrem J, et al. NCI First International Workshop on The Biology, Prevention and Treatment of Relapse after Allogeneic Hematopoietic Cell Transplantation: report from the committee on prevention of relapse following allogeneic cell transplantation for hematologic malignancies. Biol Blood Marrow Transplant. 2010;16:1037–69. This workshop review annotates various strategies used to decrease relapse of myeloid diseases after allogeneic hematopoeitic transplant.
Kim DH, Sohn SK, Kim JG, et al. Parameters for predicting allogeneic PBSCT outcome of acute myeloid leukemia: cytogenetics at presentation versus disease status at transplantation. Ann Hematol. 2005;84:25–32.
Byrd JC, Mrózek K, Dodge RK, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100:4325–36.
Ferrant A, Labopin M, Frassoni F, et al. Karyotype in acute myeloblastic leukemia: prognostic significance for bone marrow transplantation in first remission: a European Group for Blood and Marrow Transplantation study. Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Blood. 1997;90:2931–8.
Tallman MS, Dewald GW, Gandham S, et al. Impact of cytogenetics on outcome of matched unrelated donor hematopoietic stem cell transplantation for acute myeloid leukemia in first or second complete remission. Blood. 2007;110:409–17.
Paschka P, Marcucci G, Ruppert AS, et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol. 2006;24:3904–11.
Metzelder S, Wang Y, Wollmer E, et al. Compassionate use of sorafenib in FLT3-ITD-positive acute myeloid leukemia: sustained regression before and after allogeneic stem cell transplantation. Blood. 2009;113:6567–71.
Cortes JE ea. Abstract #2576: A phase II open-label, AC220 monotherapy efficacy study in patients with refractory/relapsed Flt3-Itd positive acute myeloid leukemia : Updated interim results. American Society of Hematology. San Diego, CA: Oral Poster and Abstract; 2011.
Burton E ea. Abstract#3632: The novel inhibitor PLX3397 effectively inhibits FLT3-mutant AML. American Society of Hematology. San Diego, CA: Oral Poster and Abstract; 2011.
Al-Mawali A, Gillis D, Hissaria P, Lewis I. Incidence, sensitivity, and specificity of leukemia-associated phenotypes in acute myeloid leukemia using specific five-color multiparameter flow cytometry. Am J Clin Pathol. 2008;129:934–45.
• Walter RB, Gooley TA, Wood BL, et al. Impact of pretransplantation minimal residual disease, as detected by multiparametric flow cytometry, on outcome of myeloablative hematopoietic cell transplantation for acute myeloid leukemia. J Clin Oncol. 2011;29:1190–7. This data supports the concept that MRD is a significant predictor of post-transplant survival for patients with AML.
• Chen Y, Cortes J, Estrov Z, et al. Persistence of cytogenetic abnormalities at complete remission after induction in patients with acute myeloid leukemia: prognostic significance and the potential role of allogeneic stem-cell transplantation. J Clin Oncol. 2011;29:2507–13. Examines the prognostic role of persistent cytogenetic abnormalities despite morphologic CR, and its prognostic effect.
Löwenberg B, Ossenkoppele GJ, van Putten W, et al. High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med. 2009;361:1235–48.
Fernandez HF, Sun Z, Yao X, et al. Anthracycline dose intensification in acute myeloid leukemia. N Engl J Med. 2009;361:1249–59.
Scandura JM, Roboz GJ, Moh M, et al. Phase 1 study of epigenetic priming with decitabine prior to standard induction chemotherapy for patients with AML. Blood. 2011;118:1472–80.
Faderl S, Ravandi F, Huang X, et al. A randomized study of clofarabine versus clofarabine plus low-dose cytarabine as front-line therapy for patients aged 60 years and older with acute myeloid leukemia and high-risk myelodysplastic syndrome. Blood. 2008;112:1638–45.
Faderl S, Ravandi F, Huang X, et al. Clofarabine plus low-dose cytarabine followed by clofarabine plus low-dose cytarabine alternating with decitabine in acute myeloid leukemia frontline therapy for older patients. Cancer 2012.
Clift RA, Buckner CD, Appelbaum FR, et al. Allogeneic marrow transplantation in patients with acute myeloid leukemia in first remission: a randomized trial of two irradiation regimens. Blood. 1990;76:1867–71.
• Magenau J, Tobai H, Pawarode A, et al. Clofarabine and busulfan conditioning facilitates engraftment and provides significant antitumor activity in nonremission hematologic malignancies. Blood. 2011;118:4258–64. Provides some encouraging data for the use of Clofarabine for transplant conditioning of myeloid malignancies.
Andersson BS, Valdez BC, de Lima M, et al. Clofarabine ± fludarabine with once daily i.v. busulfan as pretransplant conditioning therapy for advanced myeloid leukemia and MDS. Biol Blood Marrow Transplant. 2011;17:893–900.
Pagel JM, Appelbaum FR, Eary JF, et al. 131I-anti-CD45 antibody plus busulfan and cyclophosphamide before allogeneic hematopoietic cell transplantation for treatment of acute myeloid leukemia in first remission. Blood. 2006;107:2184–91.
• Pagel JM, Gooley TA, Rajendran J, et al. Allogeneic hematopoietic cell transplantation after conditioning with 131I-anti-CD45 antibody plus fludarabine and low-dose total body irradiation for elderly patients with advanced acute myeloid leukemia or high-risk myelodysplastic syndrome. Blood. 2009;114:5444–53. Provides encouraging data regarding the potential use of targeted radioimmunotherapy in conditioning regimens for myeloid malignancies.
Sorror ML, Sandmaier BM, Storer BE, et al. Long-term outcomes among older patients following nonmyeloablative conditioning and allogeneic hematopoietic cell transplantation for advanced hematologic malignancies. JAMA. 2011;306:1874–83.
Hegenbart U, Niederwieser D, Sandmaier BM, et al. Treatment for acute myelogenous leukemia by low-dose, total-body, irradiation-based conditioning and hematopoietic cell transplantation from related and unrelated donors. J Clin Oncol. 2006;24:444–53.
Alatrash G, de Lima M, Hamerschlak N, et al. Myeloablative reduced-toxicity i.v. busulfan-fludarabine and allogeneic hematopoietic stem cell transplant for patients with acute myeloid leukemia or myelodysplastic syndrome in the sixth through eighth decades of life. Biol Blood Marrow Transplant. 2011;17:1490–6.
Popat U, de Lima MJ, Saliba RM, et al. Long-term outcome of reduced-intensity allogeneic hematopoietic SCT in patients with AML in CR. Bone Marrow Transplant 2011.
Jakubowski AA, Small TN, Young JW, et al. T cell depleted stem-cell transplantation for adults with hematologic malignancies: sustained engraftment of HLA-matched related donor grafts without the use of antithymocyte globulin. Blood. 2007;110:4552–9.
Jakubowski AA, Small TN, Kernan NA, et al. T cell-depleted unrelated donor stem cell transplantation provides favorable disease-free survival for adults with hematologic malignancies. Biol Blood Marrow Transplant. 2011;17:1335–42.
Devine SM, Carter S, Soiffer RJ, et al. Low risk of chronic graft-versus-host disease and relapse associated with T cell-depleted peripheral blood stem cell transplantation for acute myelogenous leukemia in first remission: results of the blood and marrow transplant clinical trials network protocol 0303. Biol Blood Marrow Transplant. 2011;17:1343–51.
André-Schmutz I, Le Deist F, Hacein-Bey-Abina S, et al. Immune reconstitution without graft-versus-host disease after haemopoietic stem-cell transplantation: a phase 1/2 study. Lancet. 2002;360:130–7.
Solomon SR, Mielke S, Savani BN, et al. Selective depletion of alloreactive donor lymphocytes: a novel method to reduce the severity of graft-versus-host disease in older patients undergoing matched sibling donor stem cell transplantation. Blood. 2005;106:1123–9.
Luznik L, O'Donnell PV, Symons HJ, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Baron F, Maris MB, Sandmaier BM, et al. Graft-versus-tumor effects after allogeneic hematopoietic cell transplantation with nonmyeloablative conditioning. J Clin Oncol. 2005;23:1993–2003.
Wagner JE, Thompson JS, Carter SL, Kernan NA, Trial UDMT. Effect of graft-versus-host disease prophylaxis on 3-year disease-free survival in recipients of unrelated donor bone marrow (T-cell Depletion Trial): a multi-centre, randomised phase II-III trial. Lancet. 2005;366:733–41.
Collins RH, Shpilberg O, Drobyski WR, et al. Donor leukocyte infusions in 140 patients with relapsed malignancy after allogeneic bone marrow transplantation. J Clin Oncol. 1997;15:433–44.
Kolb HJ, Schattenberg A, Goldman JM, et al. Graft-versus-leukemia effect of donor lymphocyte transfusions in marrow grafted patients. Blood. 1995;86:2041–50.
Linn YC, Goh YT, Tan HC. Relapse of leukemia and lymphoma after marrow transplant: a review of cases with extramedullary relapse. Leuk Lymphoma. 2000;38:137–46.
Schmid C, Labopin M, Nagler A, et al. Donor lymphocyte infusion in the treatment of first hematological relapse after allogeneic stem-cell transplantation in adults with acute myeloid leukemia: a retrospective risk factors analysis and comparison with other strategies by the EBMT Acute Leukemia Working Party. J Clin Oncol. 2007;25:4938–45.
Levine JE, Braun T, Penza SL, et al. Prospective trial of chemotherapy and donor leukocyte infusions for relapse of advanced myeloid malignancies after allogeneic stem-cell transplantation. J Clin Oncol. 2002;20:405–12.
Porter DL, Levine BL, Bunin N, et al. A phase 1 trial of donor lymphocyte infusions expanded and activated ex vivo via CD3/CD28 costimulation. Blood. 2006;107:1325–31.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5675–87.
Kobbe G, Fenk R, Neumann F, et al. Transplantation of allogeneic CD34 + -selected cells followed by early T-cell add-backs: favorable results in acute and chronic myeloid leukemia. Cytotherapy. 2004;6:533–42.
Sharma M, Ravandi F, Bayraktar UD, et al. Treatment of FLT3-ITD-positive acute myeloid leukemia relapsing after allogeneic stem cell transplantation with sorafenib. Biol Blood Marrow Transplant. 2011;17:1874–7.
Pinto A, Maio M, Attadia V, Zappacosta S, Cimino R. Modulation of HLA-DR antigens expression in human myeloid leukaemia cells by cytarabine and 5-aza-2'-deoxycytidine. Lancet. 1984;2:867–8.
Coral S, Sigalotti L, Gasparollo A, et al. Prolonged upregulation of the expression of HLA class I antigens and costimulatory molecules on melanoma cells treated with 5-aza-2'-deoxycytidine (5-AZA-CdR). J Immunother. 1999;22:16–24.
Choi J, Ritchey J, Prior JL, et al. In vivo administration of hypomethylating agents mitigate graft-versus-host disease without sacrificing graft-versus-leukemia. Blood. 2010;116:129–39.
Bolaños-Meade J, Smith BD, Gore SD, et al. 5-azacytidine as salvage treatment in relapsed myeloid tumors after allogeneic bone marrow transplantation. Biol Blood Marrow Transplant. 2011;17:754–8.
de Lima M, Giralt S, Thall PF, et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer. 2010;116:5420–31.
Garcia-Manero G, Yang H, Bueso-Ramos C, et al. Phase 1 study of the histone deacetylase inhibitor vorinostat (suberoylanilide hydroxamic acid [SAHA]) in patients with advanced leukemias and myelodysplastic syndromes. Blood. 2008;111:1060–6.
Dermime S, Mavroudis D, Jiang YZ, Hensel N, Molldrem J, Barrett AJ. Immune escape from a graft-versus-leukemia effect may play a role in the relapse of myeloid leukemias following allogeneic bone marrow transplantation. Bone Marrow Transplant. 1997;19:989–99.
Tsuboi A, Oka Y, Ogawa H, et al. Constitutive expression of the Wilms' tumor gene WT1 inhibits the differentiation of myeloid progenitor cells but promotes their proliferation in response to granulocyte-colony stimulating factor (G-CSF). Leuk Res. 1999;23:499–505.
Hewitt SM, Hamada S, McDonnell TJ, Rauscher FJ, Saunders GF. Regulation of the proto-oncogenes bcl-2 and c-myc by the Wilms' tumor suppressor gene WT1. Cancer Res. 1995;55:5386–9.
Mailänder V, Scheibenbogen C, Thiel E, Letsch A, Blau IW, Keilholz U. Complete remission in a patient with recurrent acute myeloid leukemia induced by vaccination with WT1 peptide in the absence of hematological or renal toxicity. Leukemia. 2004;18:165–6.
Keilholz U, Letsch A, Busse A, et al. A clinical and immunologic phase 2 trial of Wilms tumor gene product 1 (WT1) peptide vaccination in patients with AML and MDS. Blood. 2009;113:6541–8.
Rezvani K, Yong AS, Mielke S, et al. Repeated PR1 and WT1 peptide vaccination in Montanide-adjuvant fails to induce sustained high-avidity, epitope-specific CD8+ T cells in myeloid malignancies. Haematologica. 2011;96:432–40.
de Bueger M, Bakker A, Van Rood JJ, Van der Woude F, Goulmy E. Tissue distribution of human minor histocompatibility antigens. Ubiquitous versus restricted tissue distribution indicates heterogeneity among human cytotoxic T lymphocyte-defined non-MHC antigens. J Immunol. 1992;149:1788–94.
Li N, Matte-Martone C, Zheng H, et al. Memory T cells from minor histocompatibility antigen-vaccinated and virus-immune donors improve GVL and immune reconstitution. Blood. 2011;118:5965–76.
Conflict of Interest
The authors declare no competing financial interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mawad, R., Lionberger, J.M. & Pagel, J.M. Strategies to Reduce Relapse after Allogeneic Hematopoietic Cell Transplantation in Acute Myeloid Leukemia. Curr Hematol Malig Rep 8, 132–140 (2013). https://doi.org/10.1007/s11899-013-0153-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-013-0153-6