Abstract
Purpose of Review
Monogenic diabetes is an uncommon but important form of diabetes, with the most common causes benefitting from management that accounts for the genetic mutation. This often results in decreased costs and treatment burden for affected individuals. Misdiagnosis as type 1 and type 2 diabetes is common. Given the significant burden of diabetes costs to the healthcare system, it is important to assess the economic impact of incorporating genetic testing for monogenic diabetes into clinical care through formal cost-effectiveness analyses (CEAs). This article briefly summarizes the barriers to timely monogenic diabetes diagnosis and then summarizes findings from CEAs on genetic testing for monogenic diabetes.
Recent Findings
CEAs have shown that routine genetic testing of all patients with a clinical diagnosis of type 1 diabetes can be cost-saving when applied to the scenarios of neonatal diabetes or in a pediatric population. Routine screening has not been shown to be cost-effective in adult populations. However, next-generation sequencing strategies and applying biomarkers to identify and limit genetic testing to people most likely to have monogenic diabetes are promising ways to make testing strategies cost-effective.
Summary
CEAs have shown that genetic testing for monogenic diabetes diagnosis can be cost-effective or cost-saving and should guide insurers to consider broader coverage of these tests, which would lead to accurate and timely diagnosis and impact treatment and clinical outcomes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. American Diabetes Association. 2018;41(5):917–28.
American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. American Diabetes Association. 2016;40(Supplement 1):S11–24.
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. Springer-Verlag. 2012;55(6):1577–96.
Raz I, Riddle MC, Rosenstock J, Buse JB, Inzucchi SE, Home PD, et al. Personalized management of hyperglycemia in type 2 diabetes: reflections from a diabetes care editors’ expert forum. Diabetes Care American Diabetes Association. 2013;36(6):1779–88.
Bacon S, Kyithar MP, Rizvi SR, Donnelly E, McCarthy A, Burke M, et al. Successful maintenance on sulphonylurea therapy and low diabetes complication rates in a HNF1A-MODY cohort. Diabet Med. 2016;33(7):976–84.
Shepherd MH, Shields BM, Hudson M, Pearson ER, Hyde C, Ellard S, et al. A UK nationwide prospective study of treatment change in MODY: genetic subtype and clinical characteristics predict optimal glycaemic control after discontinuing insulin and metformin. Diabetologia. Springer Berlin Heidelberg. 2018;61(12):2520–7.
Pihoker C, Gilliam LK, Ellard S, Dabelea D, Davis C, Dolan LM, et al. Prevalence, characteristics and clinical diagnosis of maturity onset diabetes of the young due to mutations in HNF1A, HNF4A, and glucokinase: results from the SEARCH for diabetes in youth. J Clin Endocrinol Metab. Endocrine Society Chevy Chase, MD. 2013;98(10):4055–62.
Shepherd M, Shields B, Hammersley S, Hudson M, McDonald TJ, Colclough K, et al. Systematic population screening, using biomarkers and genetic testing, identifies 2.5% of the U.K. Pediatric diabetes population with monogenic diabetes. Diabetes Care. American Diabetes Association. 2016;39(11):1879–88.
Shields BM, Shepherd M, Hudson M, McDonald TJ, Colclough K, Peters J, et al. Population-based assessment of a biomarker-based screening pathway to aid diagnosis of monogenic diabetes in young-onset patients. Diabetes Care. American Diabetes Association. 2017;40(8):dc170224–1025.
Kanakatti Shankar R, Pihoker C, Dolan LM, Standiford D, Badaru A, Dabelea D, et al. Permanent neonatal diabetes mellitus: prevalence and genetic diagnosis in the SEARCH for Diabetes in Youth Study. Pediatr Diabetes. John Wiley & Sons, Ltd (10.1111). 2013;14(3):174–80.
Zammit MA, Agius SM, Calleja-Agius J. Transient neonatal diabetes mellitus: a challenge and opportunity for specialized nursing care. Neonatal Netw World Health Organization. 2017;36(4):196–205.
Mackay DJG, Temple IK. Transient neonatal diabetes mellitus type 1. Weksberg R, Temple K, editors. American Journal of Medical Genetics Part C: Seminars in Medical Genetics. John Wiley & Sons, Ltd; 2010;154C(3):335–42.
Letourneau LR, Greeley SAW. Congenital forms of diabetes: the beta-cell and beyond. Curr Opin Genet Dev Elsevier Current Trends. 2018;50:25–34.
Naylor R, Knight AJ, del Gaudio D. Maturity-onset diabetes of the young overview. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews [Internet]. Seattle: University of Washington, Seattle; 2018.
Shields BM, Hicks S, Shepherd MH, Colclough K, Hattersley AT, Ellard S. Maturity-onset diabetes of the young (MODY): how many cases are we missing? Diabetologia Springer-Verlag. 2010;53(12):2504–8.
Pearson ER, Liddell WG, Shepherd M, Corrall RJ, Hattersley AT. Sensitivity to sulphonylureas in patients with hepatocyte nuclear factor-1alpha gene mutations: evidence for pharmacogenetics in diabetes. Diabet Med. 2000;17(7):543–5.
Shepherd M, Shields B, Ellard S, Cabezas OR, Hattersley AT. A genetic diagnosis of HNF1A diabetes alters treatment and improves glycaemic control in the majority of insulin-treated patients. Diabet Med. Wiley/Blackwell (10.1111). 2009;26(4):437–41.
Colclough K, Bellanné-Chantelot C, Saint-Martin C, Flanagan SE, Ellard S. Mutations in the genes encoding the transcription factors hepatocyte nuclear factor 1 alpha and 4 alpha in maturity-onset diabetes of the young and hyperinsulinemic hypoglycemia. Hum Mutat. 2013;34(5):669–85.
Steele AM, Wensley KJ, Ellard S, Murphy R, Shepherd M, Colclough K, et al. Use of HbA1c in the identification of patients with hyperglycaemia caused by a glucokinase mutation: observational case control studies. Lin XE, editor. PLoS ONE. 2013;8(6):e65326.
Stride A, Shields B, Gill-Carey O, Chakera AJ, Colclough K, Ellard S, et al. Cross-sectional and longitudinal studies suggest pharmacological treatment used in patients with glucokinase mutations does not alter glycaemia. Diabetologia. Springer Berlin Heidelberg. 2014;57(1):54–6.
Steele AM, Shields BM, Wensley KJ, Colclough K, Ellard S, Hattersley AT. Prevalence of vascular complications among patients with glucokinase mutations and prolonged, Mild Hyperglycemia. JAMA American Medical Association. 2014;311(3):279–86.
Ellard S, Bellanné-Chantelot C, Hattersley AT, Group EMGQNEM. Best practice guidelines for the molecular genetic diagnosis of maturity-onset diabetes of the young. Diabetologia. Springer-Verlag. 2008;51(4):546–53.
Carmody D, Naylor RN, Bell CD, Berry S, Montgomery JT, Tadie EC, et al. GCK-MODY in the US National Monogenic Diabetes Registry: frequently misdiagnosed and unnecessarily treated. Acta Diabetol Springer Milan. 2016;53(5):703–8.
Kleinberger JW, Copeland KC, Gandica RG, Haymond MW, LEVITSKY LL, Linder B, et al. Monogenic diabetes in overweight and obese youth diagnosed with type 2 diabetes: the TODAY clinical trial. Genet Med Nature Publishing Group. 2018;20(6):583–90.
Ramsey S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force Report. Value in Health. John Wiley & Sons, Ltd (10.1111). 2005;8(5):521–33.
Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull Oxford University Press. 2010;96(1):5–21.
Braithwaite RS, Meltzer DO, King JT Jr, Leslie D, Roberts MS.What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. 2008;46(4):349-56.
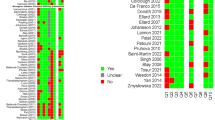
• Greeley SAW, John PM, Winn AN, Ornelas J, Lipton RB, Philipson LH, et al. The cost-effectiveness of personalized genetic medicine: the case of genetic testing in neonatal diabetes. Diabetes Care. 2011;34(3):622–7. This study assesses the cost-effectiveness of routine genetic testing for monogenic neonatal diabetes in a hypothetical patient cohort with infancy-onset diabetes.
• Peters JL, Anderson R, Hyde C. Development of an economic evaluation of diagnostic strategies: the case of monogenic diabetes. BMJ Open. 2013;3(5):e002905. This study defines five test-treatment strategies for monogenic diabetes relevant for cost-effectiveness analyses.
• Naylor RN, John PM, Winn AN, Carmody D, Greeley SAW, Philipson LH, et al. Cost-effectiveness of MODY genetic testing: translating genomic advances into practical health applications. Diabetes Care. 2014;37(1):202–9. This study assesses the cost-effectiveness of routine genetic testing in a hypothetical patient cohort with young-onset, presumed type 2 diabetes.
Clarke PM, Gray AM, Briggs A, Farmer AJ, Fenn P, Stevens RJ, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia Springer-Verlag. 2004;47(10):1747–59.
•• Nguyen HV, Finkelstein EA, Mital S, Gardner DS-L. Incremental cost-effectiveness of algorithm-driven genetic testing versus no testing for Maturity Onset Diabetes of the Young (MODY) in Singapore. J Med Genet. 2017;54(11):747–53. This study assesses the cost-effectiveness of algorithm-driven genetic testing in a patient cohort with young-onset diabetes.
•• Johnson SR, Carter HE, Leo P, Hollingworth SA, Davis EA, Jones TW, et al. Cost-effectiveness analysis of routine screening using massively parallel sequencing for maturity-onset diabetes of the young in a pediatric diabetes cohort: reduced health system costs and improved patient quality of life. Diabetes Care. 2018;dc180261. This study assesses the cost-effectiveness of routine genetic testing using mass parallel sequencing for MODY in a pediatric patient cohort with presumed type 1 diabetes.
Thokala P, Kruger J, Brennan A, Basarir H, Duenas A, Pandor A, et al. Assessing the cost-effectiveness of type 1 diabetes interventions: the Sheffield Type 1 Diabetes Policy Model. Diabet Med. John Wiley & Sons, Ltd (10.1111). 2014;31(4):477–86.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Economics And Policy In Diabetes
Rights and permissions
About this article
Cite this article
Naylor, R. Economics of Genetic Testing for Diabetes. Curr Diab Rep 19, 23 (2019). https://doi.org/10.1007/s11892-019-1140-7
Published:
DOI: https://doi.org/10.1007/s11892-019-1140-7